Strongyloidiasis is a common parasitic disease caused by infection with the roundworm Strongyloides stercoralis. Transmission occurs through skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions penetration Penetration X-rays, most commonly from walking barefoot. Strongyloides has a unique life cycle that can be entirely completed in the human host, migrating from the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions to the pulmonary system and then to the GI system. Symptoms include cutaneous irritation, constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation, diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, dry cough, and wheezing Wheezing Wheezing is an abnormal breath sound characterized by a whistling noise that can be relatively high-pitched and shrill (more common) or coarse. Wheezing is produced by the movement of air through narrowed or compressed small (intrathoracic) airways. Wheezing, depending on where the parasite is in its life cycle. Effective eradication of the parasite can be obtained with anthelmintic medications, usually ivermectin Ivermectin A mixture of mostly avermectin h2b1a (rn 71827-03-7) with some avermectin h2b1b (rn 70209-81-3), which are macrolides from streptomyces avermitilis. It binds glutamate-gated chloride channel to cause increased permeability and hyperpolarization of nerve and muscle cells. It also interacts with other chloride channels. It is a broad spectrum antiparasitic that is active against microfilariae of onchocerca volvulus but not the adult form. Anthelmintic Drugs.
Last updated: Nov 7, 2022
Strongyloidiasis is caused by a parasitic infection by the roundworm ( nematode Nematode A phylum of unsegmented helminths with fundamental bilateral symmetry and secondary triradiate symmetry of the oral and esophageal structures. Many species are parasites. Toxocariasis) Strongyloides stercoralis. Roundworms Roundworms Anthelmintic Drugs are nonsegmented worms that can infect the GI tract, blood, or skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions.

Strongyloides sp.:
Photomicrograph with a magnification of 128X of a Strongyloides sp. filariform, a larval-staged organism
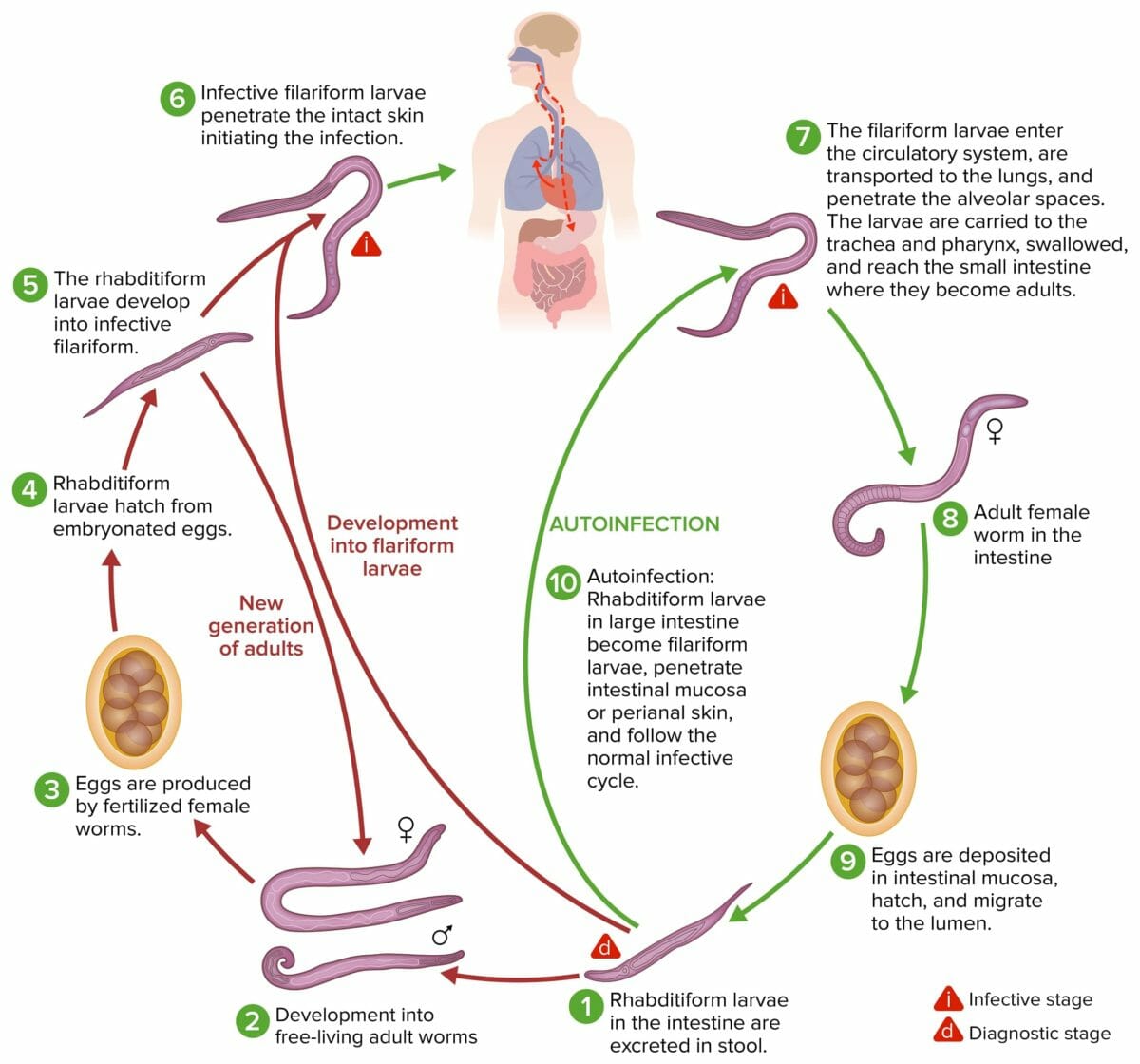
The life cycle of Strongyloides stercoralis:
The roundworm S. stercoralis has a unique lifecycle that can be completed within its definitive human host. The parasite is transmitted to other hosts through excreted feces, but in immunodeficient patients, autoinfection can occur, leading to more severe, chronic forms of the disease.
Strongyloidiasis can cause both acute and chronic infection. Symptoms correlate with the migration of the larvae Larvae Wormlike or grublike stage, following the egg in the life cycle of insects, worms, and other metamorphosing animals. Ascaris/Ascariasis from the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, lung, and intestine.
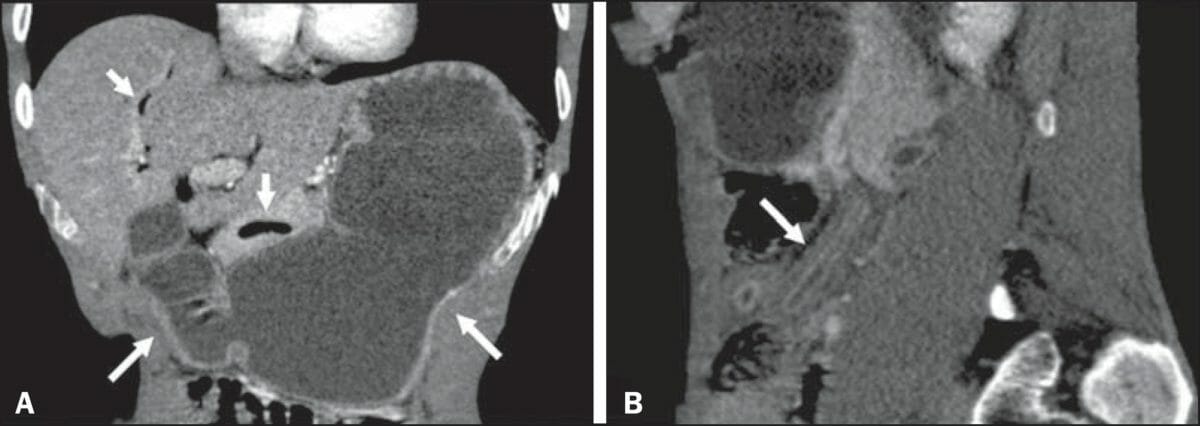
Intestinal strongyloidiasis:
A) Contrast-enhanced CT in the coronal plane shows accentuated duodenal and gastric distension (long arrows) and gas in the biliary tract and pancreas (short arrows).
B) CT in the sagittal plane shows the lead pipe sign, characterized by thickening of the walls, rigidity, and luminal narrowing of the small intestine (long arrow).
Diagnosis requires a high clinical suspicion test, based on symptoms.
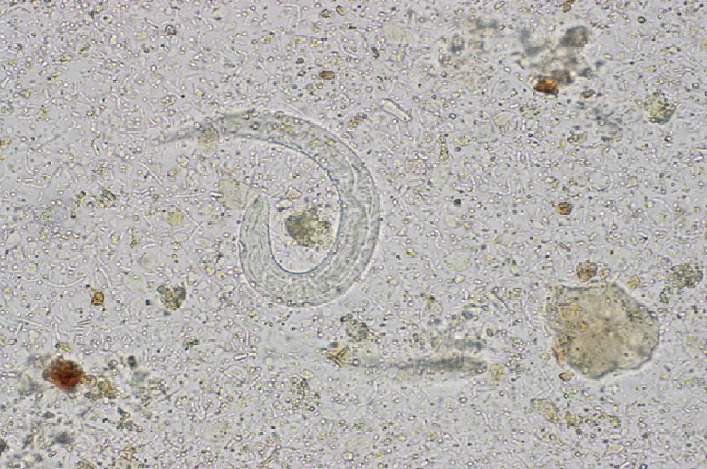
Wet mount of stool showing Strongyloides larvae
Image: “Strongyloides Hyperinfection in a Renal Transplant Patient: Always Be on the Lookout” by Case Reports in Infectious Diseases. License: CC BY 4.0