Pain has accompanied humans since they first existed, first lamented as the curse of existence and later understood as an adaptive mechanism that ensures survival. Pain is the most common symptomatic complaint and the main reason why people seek medical care Medical care Conflict of Interest. Pain symptoms are seen every day, by every physician, in every clinic and hospital in the world. Understanding pain physiology is the cornerstone to understanding how to treat it and to providing the individual with their first sigh of relief as definitive management is undertaken.
Last updated: May 17, 2024
| Physiologic change | Acute pain Acute pain Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, with well-defined location, character, and timing. Pain Management | Chronic pain Chronic pain Aching sensation that persists for more than a few months. It may or may not be associated with trauma or disease, and may persist after the initial injury has healed. Its localization, character, and timing are more vague than with acute pain. Pain Management |
|---|---|---|
| Vital signs | May vary consistently with degree of pain severity | No or minimal change |
| Purpose of pain | Useful | Inhibits function and not useful |
| Central sensitization | Short term; improves with healing of injury | Remains present despite absence of ongoing injury |
| Neuropathic pain | Increases likelihood of chronic pain Chronic pain Aching sensation that persists for more than a few months. It may or may not be associated with trauma or disease, and may persist after the initial injury has healed. Its localization, character, and timing are more vague than with acute pain. Pain Management when present in acute phase Acute phase Short Bowel Syndrome | Common etiology of chronic pain Chronic pain Aching sensation that persists for more than a few months. It may or may not be associated with trauma or disease, and may persist after the initial injury has healed. Its localization, character, and timing are more vague than with acute pain. Pain Management |
| Nociceptive pain | Often found during acute pain Acute pain Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, with well-defined location, character, and timing. Pain Management state | Commonly presents with some neuropathic pain |
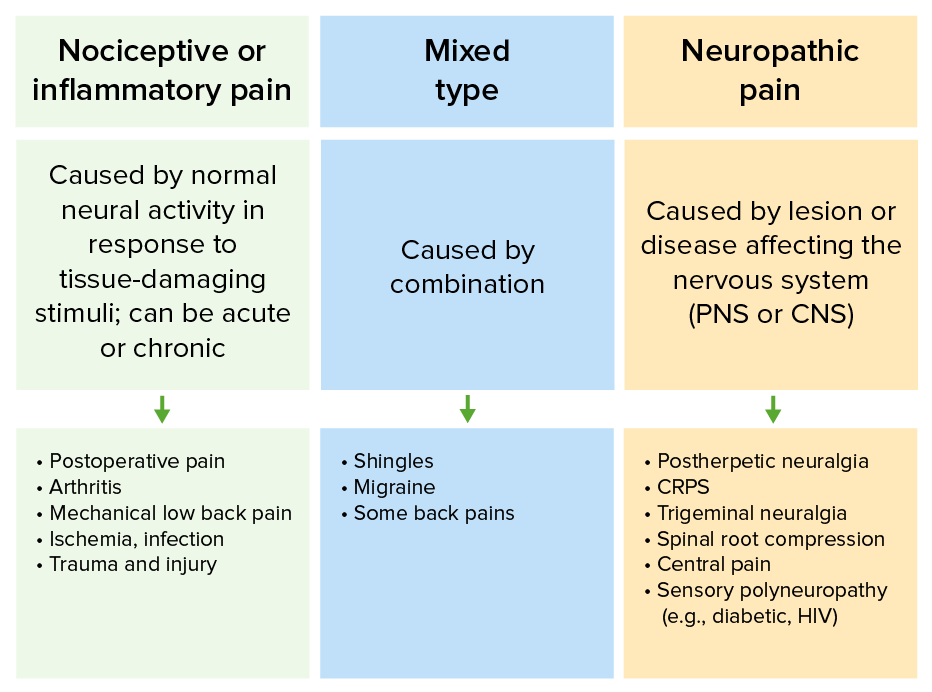
Differences in types of pain and their common etiologies
CRPS: complex regional pain syndrome
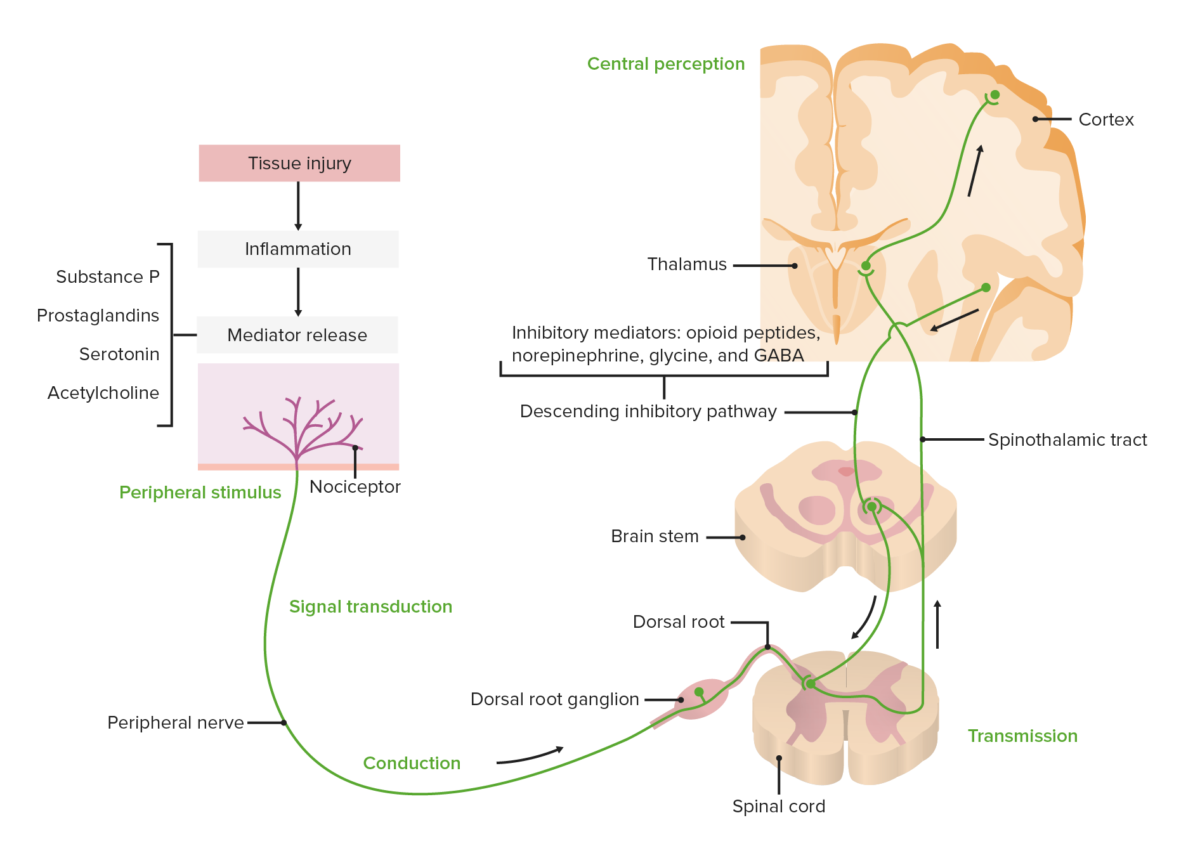
Diagram showing the pathway of pain transduction, transmission, modulation, and central perception
Image by Lecturio.Type A fibers:
Type B fibers:
Type C fibers:
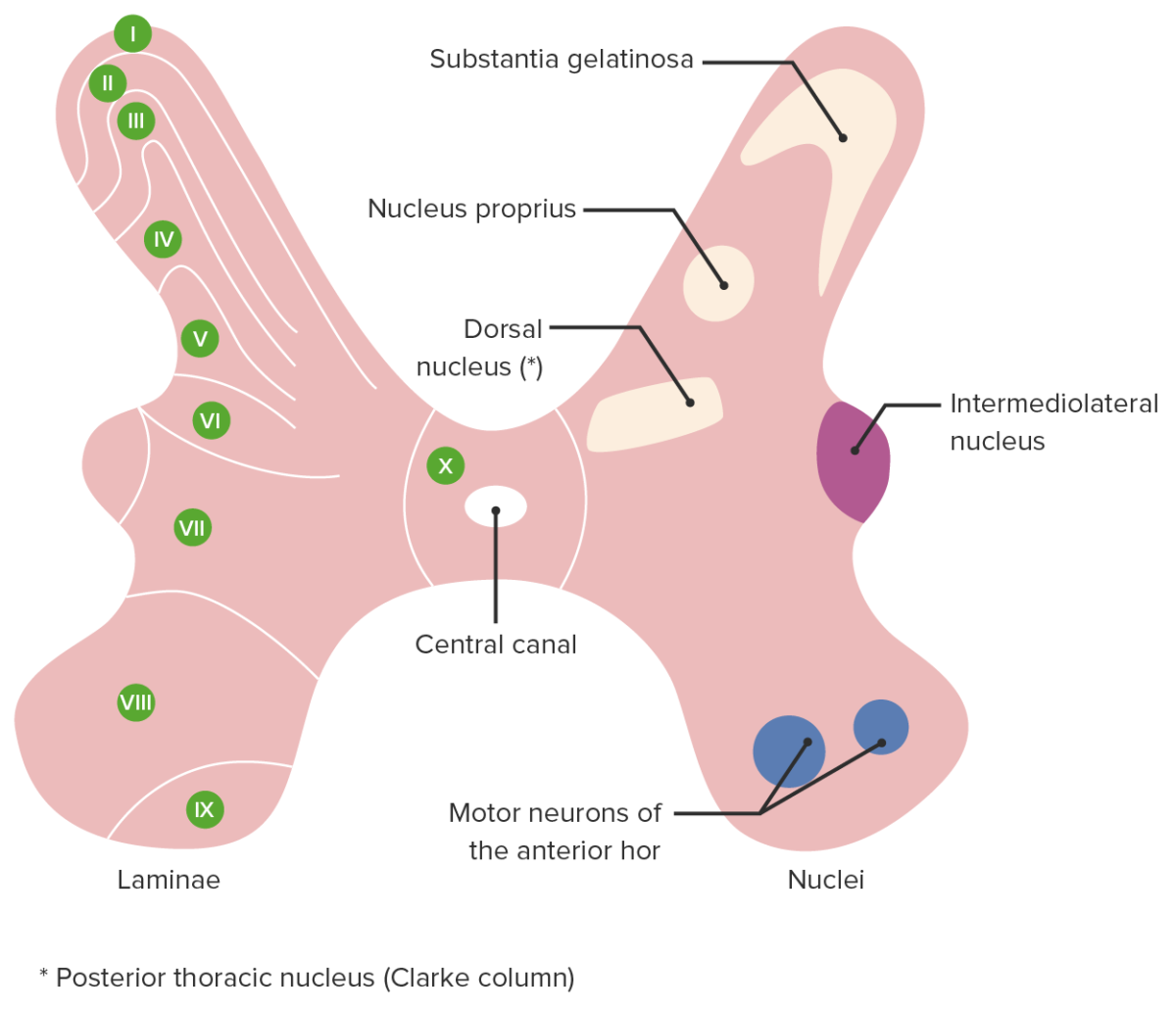
Cross section of the spinal cord showing the rexed laminae (left) and associated nuclei (right)
Image by Lecturio.Ascending pathway of pain:
Descending pathway of pain:
The hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus and cortical regions process painful stimuli and signal for the release of inhibitory mediators and hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types (e.g., opioid Opioid Compounds with activity like opiate alkaloids, acting at opioid receptors. Properties include induction of analgesia or narcosis. Constipation peptides, norepinephrine Norepinephrine Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers, and of the diffuse projection system in the brain that arises from the locus ceruleus. Receptors and Neurotransmitters of the CNS, glycine Glycine A non-essential amino acid. It is found primarily in gelatin and silk fibroin and used therapeutically as a nutrient. It is also a fast inhibitory neurotransmitter. Synthesis of Nonessential Amino Acids, and GABA GABA The most common inhibitory neurotransmitter in the central nervous system. Receptors and Neurotransmitters of the CNS) that make pain suppression Suppression Defense Mechanisms more effective → pain modulation
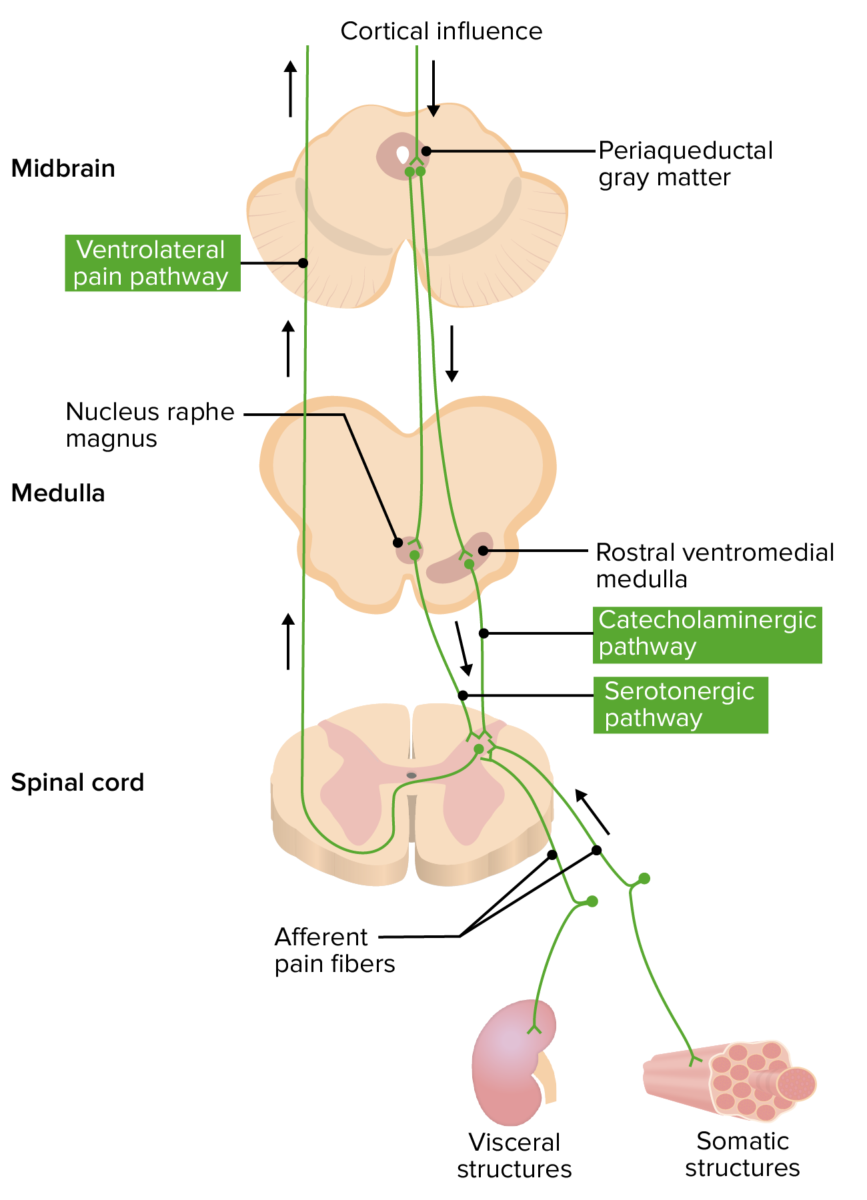
Diagram illustrating the convergence-projection theory of visceral pain
Image by Lecturio.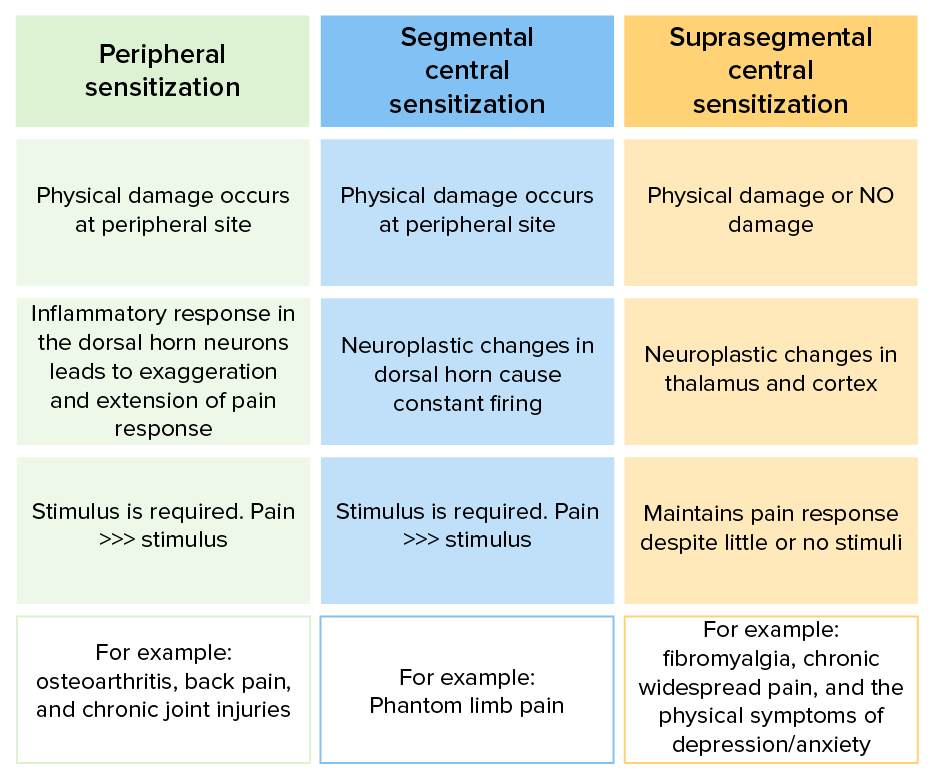
Mechanisms of peripheral and central pain sensitization
Image by Lecturio.