Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. The work of hormones allows the body to maintain homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death and regulate growth and development. Hormones are typically either made from amino acids Amino acids Organic compounds that generally contain an amino (-NH2) and a carboxyl (-COOH) group. Twenty alpha-amino acids are the subunits which are polymerized to form proteins. Basics of Amino Acids or derived from cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism (the latter group being known as steroid hormones). Hormones exert their effects by binding to receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors either on the cell surface (most amino acid Amino acid Amino acids (AAs) are composed of a central carbon atom attached to a carboxyl group, an amino group, a hydrogen atom, and a side chain (R group). Basics of Amino Acids–based hormones) or within the cytosol Cytosol A cell's cytoskeleton is a network of intracellular protein fibers that provides structural support, anchors organelles, and aids intra- and extracellular movement. The Cell: Cytosol and Cytoskeleton (steroid hormones). Ultimately, binding to receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors triggers changes in gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics expression or enzymatic activity within the cell.
Last updated: Jun 27, 2025
Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body.
Major functions of hormones include:
The major endocrine glands Endocrine glands Ductless glands that secrete hormones directly into the blood circulation. These hormones influence the metabolism and other functions of cells in the body. Glandular Epithelium: Histology in the body include:
| Gland/organ | Hormone secreted by the gland/organ | Primary effect of the hormone |
|---|---|---|
| Hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus | Thyrotropin-releasing hormone Thyrotropin-releasing hormone A tripeptide that stimulates the release of thyrotropin and prolactin. It is synthesized by the neurons in the paraventricular nucleus of the hypothalamus. After being released into the pituitary portal circulation, TRH stimulates the release of TSH and PRL from the anterior pituitary gland. Hypothalamic and Pituitary Hormones (TRH) | Stimulates pituitary thyrotropes to secrete thyroid-stimulating hormone Thyroid-stimulating hormone A glycoprotein hormone secreted by the adenohypophysis. Thyrotropin stimulates thyroid gland by increasing the iodide transport, synthesis and release of thyroid hormones (thyroxine and triiodothyronine). Thyroid Hormones (TSH) |
| Corticotropin-releasing hormone Corticotropin-releasing hormone A peptide of about 41 amino acids that stimulates the release of adrenocorticotropic hormone. Crh is synthesized by neurons in the paraventricular nucleus of the hypothalamus. After being released into the pituitary portal circulation, crh stimulates the release of acth from the pituitary gland. Crh can also be synthesized in other tissues, such as placenta; adrenal medulla; and testis. Hypothalamic and Pituitary Hormones (CRH) | Stimulates pituitary corticotropes to secrete adrenocorticotropic hormone Adrenocorticotropic hormone An anterior pituitary hormone that stimulates the adrenal cortex and its production of corticosteroids. Acth is a 39-amino acid polypeptide of which the n-terminal 24-amino acid segment is identical in all species and contains the adrenocorticotropic activity. Upon further tissue-specific processing, acth can yield alpha-msh and corticotropin-like intermediate lobe peptide (clip). Adrenal Hormones (ACTH) | |
| Gonadotropin-releasing hormone Gonadotropin-releasing hormone A decapeptide that stimulates the synthesis and secretion of both pituitary gonadotropins, luteinizing hormone and follicle stimulating hormone. Gnrh is produced by neurons in the septum preoptic area of the hypothalamus and released into the pituitary portal blood, leading to stimulation of gonadotrophs in the anterior pituitary gland. Puberty (GnRH) | Stimulates pituitary gonadotropes to secrete FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle and LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle | |
| Growth hormone–releasing hormone ( GHRH GHRH A peptide of 44 amino acids in most species that stimulates the release and synthesis of growth hormone. GHRF (or GRF) is synthesized by neurons in the arcuate nucleus of the hypothalamus. After being released into the pituitary portal circulation, GHRF stimulates gh release by the somatotrophs in the pituitary gland. Hypothalamic and Pituitary Hormones) | Stimulates pituitary somatotropes to secrete GH | |
| Somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions | Inhibits the release of GH and TSH from the pituitary | |
| Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS | Inhibits the release of prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy from pituitary lactotropes | |
| Anterior pituitary | TSH | Stimulates secretion Secretion Coagulation Studies of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy hormones |
| Adrenocorticotropic hormone Adrenocorticotropic hormone An anterior pituitary hormone that stimulates the adrenal cortex and its production of corticosteroids. Acth is a 39-amino acid polypeptide of which the n-terminal 24-amino acid segment is identical in all species and contains the adrenocorticotropic activity. Upon further tissue-specific processing, acth can yield alpha-msh and corticotropin-like intermediate lobe peptide (clip). Adrenal Hormones (ACTH) | Stimulates secretion Secretion Coagulation Studies of hormones by the adrenal cortex Adrenal Cortex The outer layer of the adrenal gland. It is derived from mesoderm and comprised of three zones (outer zona glomerulosa, middle zona fasciculata, and inner zona reticularis) with each producing various steroids preferentially, such as aldosterone; hydrocortisone; dehydroepiandrosterone; and androstenedione. Adrenal cortex function is regulated by pituitary adrenocorticotropin. Adrenal Glands: Anatomy | |
| Follicle-stimulating hormone ( FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle) | Stimulates gamete Gamete Gametogenesis production in the gonads | |
| Luteinizing hormone ( LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle) | Stimulates gonadal androgen production | |
| Growth hormone (GH) | Promotes the growth of body tissues | |
| Prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy (PRL) | Promotes the production of breast milk | |
| Posterior pituitary | Antidiuretic hormone Antidiuretic hormone Antidiuretic hormones released by the neurohypophysis of all vertebrates (structure varies with species) to regulate water balance and osmolarity. In general, vasopressin is a nonapeptide consisting of a six-amino-acid ring with a cysteine 1 to cysteine 6 disulfide bridge or an octapeptide containing a cystine. All mammals have arginine vasopressin except the pig with a lysine at position 8. Vasopressin, a vasoconstrictor, acts on the kidney collecting ducts to increase water reabsorption, increase blood volume and blood pressure. Hypernatremia (ADH) | Stimulates water absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption by the kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy |
| Oxytocin | Stimulates:
|
|
| Pineal gland | Melatonin | Regulates sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep cycles |
| Thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland |
Thyroid
Thyroid
The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck.
Thyroid Gland: Anatomy hormones:
|
Stimulates cellular metabolism Cellular metabolism The chemical reactions in living organisms by which energy is provided for vital processes and activities and new material is assimilated. Thyroid Hormones |
| Calcitonin Calcitonin A peptide hormone that lowers calcium concentration in the blood. In humans, it is released by thyroid cells and acts to decrease the formation and absorptive activity of osteoclasts. Its role in regulating plasma calcium is much greater in children and in certain diseases than in normal adults. Other Antiresorptive Drugs | ↓ Serum Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)2+ | |
| Parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy gland | Parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone (PTH) | ↑ Serum Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)2+ |
| Adrenal cortex Adrenal Cortex The outer layer of the adrenal gland. It is derived from mesoderm and comprised of three zones (outer zona glomerulosa, middle zona fasciculata, and inner zona reticularis) with each producing various steroids preferentially, such as aldosterone; hydrocortisone; dehydroepiandrosterone; and androstenedione. Adrenal cortex function is regulated by pituitary adrenocorticotropin. Adrenal Glands: Anatomy | Mineralocorticoids Mineralocorticoids Mineralocorticoids are a drug class within the corticosteroid family and fludrocortisone is the primary medication within this class. Fludrocortisone is a fluorinated analog of cortisone. The fluorine moiety protects the drug from isoenzyme inactivation in the kidney, allowing it to exert its mineralocorticoid effect. Mineralocorticoids: aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia |
|
Glucocorticoids
Glucocorticoids
Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs.
Glucocorticoids:
|
|
|
| Androgens Androgens Androgens are naturally occurring steroid hormones responsible for development and maintenance of the male sex characteristics, including penile, scrotal, and clitoral growth, development of sexual hair, deepening of the voice, and musculoskeletal growth. Androgens and Antiandrogens | Stimulates secondary sex characteristics Secondary sex characteristics Gonadal Hormones | |
| Adrenal medulla Adrenal Medulla The inner portion of the adrenal gland. Derived from ectoderm, adrenal medulla consists mainly of chromaffin cells that produces and stores a number of neurotransmitters, mainly adrenaline (epinephrine) and norepinephrine. The activity of the adrenal medulla is regulated by the sympathetic nervous system. Adrenal Glands: Anatomy |
Catecholamines
Catecholamines
A general class of ortho-dihydroxyphenylalkylamines derived from tyrosine.
Adrenal Hormones:
|
Stimulates fight-or-flight reaction |
| Gonads | Testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens | Stimulates:
|
| Estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy and progesterone Progesterone The major progestational steroid that is secreted primarily by the corpus luteum and the placenta. Progesterone acts on the uterus, the mammary glands and the brain. It is required in embryo implantation; pregnancy maintenance, and the development of mammary tissue for milk production. Progesterone, converted from pregnenolone, also serves as an intermediate in the biosynthesis of gonadal steroid hormones and adrenal corticosteroids. Gonadal Hormones |
|
|
| Inhibin | Selectively inhibits the release of FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle | |
| Placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity | Estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy | Supports maternal physiology during pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care |
| Progesterone Progesterone The major progestational steroid that is secreted primarily by the corpus luteum and the placenta. Progesterone acts on the uterus, the mammary glands and the brain. It is required in embryo implantation; pregnancy maintenance, and the development of mammary tissue for milk production. Progesterone, converted from pregnenolone, also serves as an intermediate in the biosynthesis of gonadal steroid hormones and adrenal corticosteroids. Gonadal Hormones |
|
|
| Human chorionic gonadotropin (hCG) | Maintains the endocrine activity of the corpus luteum Corpus Luteum The yellow body derived from the ruptured ovarian follicle after ovulation. The process of corpus luteum formation, luteinization, is regulated by luteinizing hormone. Ovaries: Anatomy | |
| Human placental lactogen (hPL) | Alters maternal insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin secretion Secretion Coagulation Studies in order to ↑ glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance for the fetus | |
| Insulin-like growth factor | Regulates fetal growth | |
| Placental CRH and glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids | Regulate organ development and maturation |
| Gland/organ | Hormone secreted by the gland/organ | Primary effect of the hormone |
|---|---|---|
| Stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy | Gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions, histamine | Stimulates HCl HCL Hairy cell leukemia (HCL) is a rare, chronic, B-cell leukemia characterized by the accumulation of small mature B lymphocytes that have “hair-like projections” visible on microscopy. The abnormal cells accumulate in the peripheral blood, bone marrow (causing fibrosis), and red pulp of the spleen, leading to cytopenias. Hairy Cell Leukemia secretion Secretion Coagulation Studies in the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy |
| Serotonin Serotonin A biochemical messenger and regulator, synthesized from the essential amino acid l-tryptophan. In humans it is found primarily in the central nervous system, gastrointestinal tract, and blood platelets. Serotonin mediates several important physiological functions including neurotransmission, gastrointestinal motility, hemostasis, and cardiovascular integrity. Receptors and Neurotransmitters of the CNS | Stimulates gastric motility Gastric motility Gastrointestinal Motility | |
| Pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy | Insulin Insulin Insulin is a peptide hormone that is produced by the beta cells of the pancreas. Insulin plays a role in metabolic functions such as glucose uptake, glycolysis, glycogenesis, lipogenesis, and protein synthesis. Exogenous insulin may be needed for individuals with diabetes mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance. Insulin | ↓ Blood sugar levels by moving glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance across cell membranes into the intracellular space |
| Glucagon Glucagon A 29-amino acid pancreatic peptide derived from proglucagon which is also the precursor of intestinal glucagon-like peptides. Glucagon is secreted by pancreatic alpha cells and plays an important role in regulation of blood glucose concentration, ketone metabolism, and several other biochemical and physiological processes. Gastrointestinal Secretions | ↑ Blood sugar levels by stimulating gluconeogenesis Gluconeogenesis Gluconeogenesis is the process of making glucose from noncarbohydrate precursors. This metabolic pathway is more than just a reversal of glycolysis. Gluconeogenesis provides the body with glucose not obtained from food, such as during a fasting period. The production of glucose is critical for organs and cells that cannot use fat for fuel. Gluconeogenesis and glycogenolysis Glycogenolysis The release of glucose from glycogen by glycogen phosphorylase (phosphorolysis). The released glucose-1-phosphate is then converted to glucose-6-phosphate by phosphoglucomutase before entering glycolysis. Glycogenolysis is stimulated by glucagon or epinephrine via the activation of phosphorylase kinase. Glycogen Metabolism | |
| Intestines | Secretin Secretin A peptide hormone of about 27 amino acids from the duodenal mucosa that activates pancreatic secretion and lowers the blood sugar level. Gastrointestinal Secretions |
|
| Cholecystokinin Cholecystokinin A peptide, of about 33 amino acids, secreted by the upper intestinal mucosa and also found in the central nervous system. It causes gallbladder contraction, release of pancreatic exocrine (or digestive) enzymes, and affects other gastrointestinal functions. Cholecystokinin may be the mediator of satiety. Gastrointestinal Secretions |
|
|
| Glucose-dependent insulinotropic polypeptide ( GIP GIP A gastrointestinal peptide hormone of about 43-amino acids. It is found to be a potent stimulator of insulin secretion and a relatively poor inhibitor of gatsric acid secretion. Gastrointestinal Neural and Hormonal Signaling) |
|
|
| Glucagon-like peptide-1 ( GLP-1 GLP-1 A peptide of 36 or 37 amino acids that is derived from proglucagon and mainly produced by the intestinal l cells. Glp-1(1-37 or 1-36) is further n-terminally truncated resulting in glp-1(7-37) or glp-1-(7-36) which can be amidated. These glp-1 peptides are known to enhance glucose-dependent insulin release, suppress glucagon release and gastric emptying, lower blood glucose, and reduce food intake. Insulinomas) |
|
Thymus Thymus A single, unpaired primary lymphoid organ situated in the mediastinum, extending superiorly into the neck to the lower edge of the thyroid gland and inferiorly to the fourth costal cartilage. It is necessary for normal development of immunologic function early in life. By puberty, it begins to involute and much of the tissue is replaced by fat. Lymphatic Drainage System: Anatomy | Thymopoietin | Regulates immune function |
| Adipose tissue Adipose tissue Adipose tissue is a specialized type of connective tissue that has both structural and highly complex metabolic functions, including energy storage, glucose homeostasis, and a multitude of endocrine capabilities. There are three types of adipose tissue, white adipose tissue, brown adipose tissue, and beige or “brite” adipose tissue, which is a transitional form. Adipose Tissue: Histology | Leptin Leptin A 16-kda peptide hormone secreted from white adipocytes. Leptin serves as a feedback signal from fat cells to the central nervous system in regulation of food intake, energy balance, and fat storage. Adipose Tissue: Histology | Suppresses food intake |
| Heart | Atrial natriuretic peptide Atrial natriuretic peptide A potent natriuretic and vasodilatory peptide or mixture of different-sized low molecular weight peptides derived from a common precursor and secreted mainly by the heart atrium. All these peptides share a sequence of about 20 amino acids. Renal Sodium and Water Regulation (ANP) | Reduces plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products volume by stimulating diuresis |
| Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy | Angiotensinogen | A precursor for angiotensin II Angiotensin II An octapeptide that is a potent but labile vasoconstrictor. It is produced from angiotensin I after the removal of two amino acids at the c-terminal by angiotensin converting enzyme. The amino acid in position 5 varies in different species. To block vasoconstriction and hypertension effect of angiotensin II, patients are often treated with ace inhibitors or with angiotensin II type 1 receptor blockers. Renal Sodium and Water Regulation, a potent vasoconstrictor that stimulates aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia |
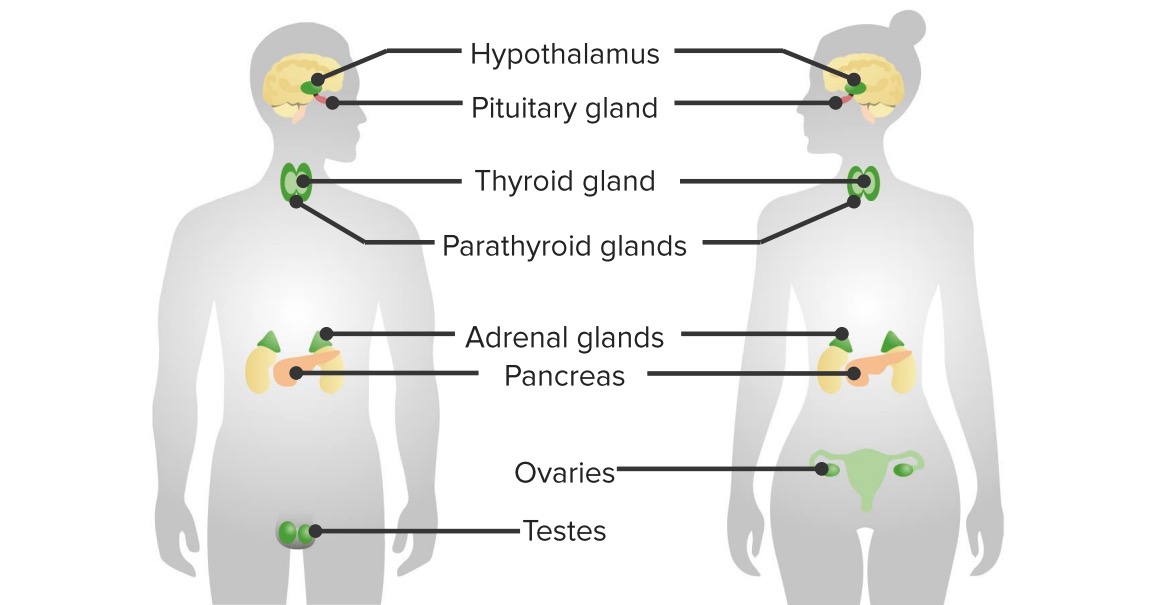
Major organs of the endocrine system
Image by Lecturio.Most hormones are amino acid Amino acid Amino acids (AAs) are composed of a central carbon atom attached to a carboxyl group, an amino group, a hydrogen atom, and a side chain (R group). Basics of Amino Acids–based.
Most hormones bind BIND Hyperbilirubinemia of the Newborn to receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors, which then convey their message through secondary messengers and/or signal cascades. Steroid hormones, when bound to their receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors, are able to directly bind BIND Hyperbilirubinemia of the Newborn DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure and affect gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics expression.
There are several ways hormones send messages throughout the body:
Plasma membrane Plasma membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors are typically required for amino acid Amino acid Amino acids (AAs) are composed of a central carbon atom attached to a carboxyl group, an amino group, a hydrogen atom, and a side chain (R group). Basics of Amino Acids–based hormones and use 2nd-messenger systems and signal cascades:
Intracellular receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors generally cause direct gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics activation:

Steroid hormone signaling
Image by Kevin Ahern, MD.Just about every hormone listed in the tables can be secreted in abnormal levels, resulting in a wide range of clinical conditions. Some of these conditions include: