Precocious puberty Puberty Puberty is a complex series of physical, psychosocial, and cognitive transitions usually experienced by adolescents (11-19 years of age). Puberty is marked by a growth in stature and the development of secondary sexual characteristics, achievement of fertility, and changes in most body systems. Puberty (PP) is the appearance of secondary sexual characteristics due to elevated sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types before the age of 6–8 in girls and 9 in boys. Excess hormone secretion Secretion Coagulation Studies may occur only at the level of the sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormone or may involve the whole hypothalamic-pituitary-gonadal axis Hypothalamic-pituitary-gonadal axis Gonadal Hormones. Measurement of sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormone levels, as well as X-rays X-rays X-rays are high-energy particles of electromagnetic radiation used in the medical field for the generation of anatomical images. X-rays are projected through the body of a patient and onto a film, and this technique is called conventional or projectional radiography. X-rays to evaluate skeletal maturity, are used to diagnose and characterize PP. Correcting the hormonal excess at its root cause can appropriately delay the onset of puberty Puberty Puberty is a complex series of physical, psychosocial, and cognitive transitions usually experienced by adolescents (11-19 years of age). Puberty is marked by a growth in stature and the development of secondary sexual characteristics, achievement of fertility, and changes in most body systems. Puberty. A primary goal of treatment is the preservation of normal height potential.
Last updated: Jan 28, 2025
The prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of precocious puberty Puberty Puberty is a complex series of physical, psychosocial, and cognitive transitions usually experienced by adolescents (11-19 years of age). Puberty is marked by a growth in stature and the development of secondary sexual characteristics, achievement of fertility, and changes in most body systems. Puberty varies based on the race and ethnic makeup of the population.
| Causes of isosexual precocious puberty Puberty Puberty is a complex series of physical, psychosocial, and cognitive transitions usually experienced by adolescents (11-19 years of age). Puberty is marked by a growth in stature and the development of secondary sexual characteristics, achievement of fertility, and changes in most body systems. Puberty | Causes of heterosexual precocious puberty Puberty Puberty is a complex series of physical, psychosocial, and cognitive transitions usually experienced by adolescents (11-19 years of age). Puberty is marked by a growth in stature and the development of secondary sexual characteristics, achievement of fertility, and changes in most body systems. Puberty | |
|---|---|---|
| Girls |
|
|
| Boys |
|
|
Focused history looking for possible causes of PP:
| Tanner stage Tanner stage Sexual Physiology | Breasts Breasts The breasts are found on the anterior thoracic wall and consist of mammary glands surrounded by connective tissue. The mammary glands are modified apocrine sweat glands that produce milk, which serves as nutrition for infants. Breasts are rudimentary and usually nonfunctioning in men. Breasts: Anatomy (female) | Pubic hair | Genitals (male) |
|---|---|---|---|
| I | B1: No breast development; no palpable glandular tissue | P1: No pubic hair | G1: Pre-pubertal: testicular volume < 4 mL and small penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy |
| II | B2: Breast bud; areola Areola Examination of the Breast begins to widen; small area of glandular tissue | P2: Labia majora Labia majora Vagina, Vulva, and Pelvic Floor: Anatomy or mons pubis Mons pubis Vagina, Vulva, and Pelvic Floor: Anatomy: small amount of long, downy hair | G2: Testicular volume > 4 mL; skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions on scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy thins, reddens and enlarges; penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy unchanged |
| III | B3: Breast tissue enlarges; glandular tissue extends beyond the borders of the areola Areola Examination of the Breast | P3: Hair becomes darker and coarser, extends laterally over the symphysis | G3: Penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy begins to grow, testicular volume increases further |
| IV | B4: Breast bud: elevation of glandular tissue in the areola Areola Examination of the Breast area from other breast tissue | P4: Coarse hair (adult-like), less extended | G4: Penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy increases in length and circumference; testicular volume increases further; scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy enlarges further and darkens |
| V | B5: Fully developed breast; areola Areola Examination of the Breast returns to the contour of the surrounding breast | P5: Coarse hair (adult-like), extended to the groin Groin The external junctural region between the lower part of the abdomen and the thigh. Male Genitourinary Examination and medial thighs | G5: Adult size genitalia with a testicular volume 12.5–19 mL |
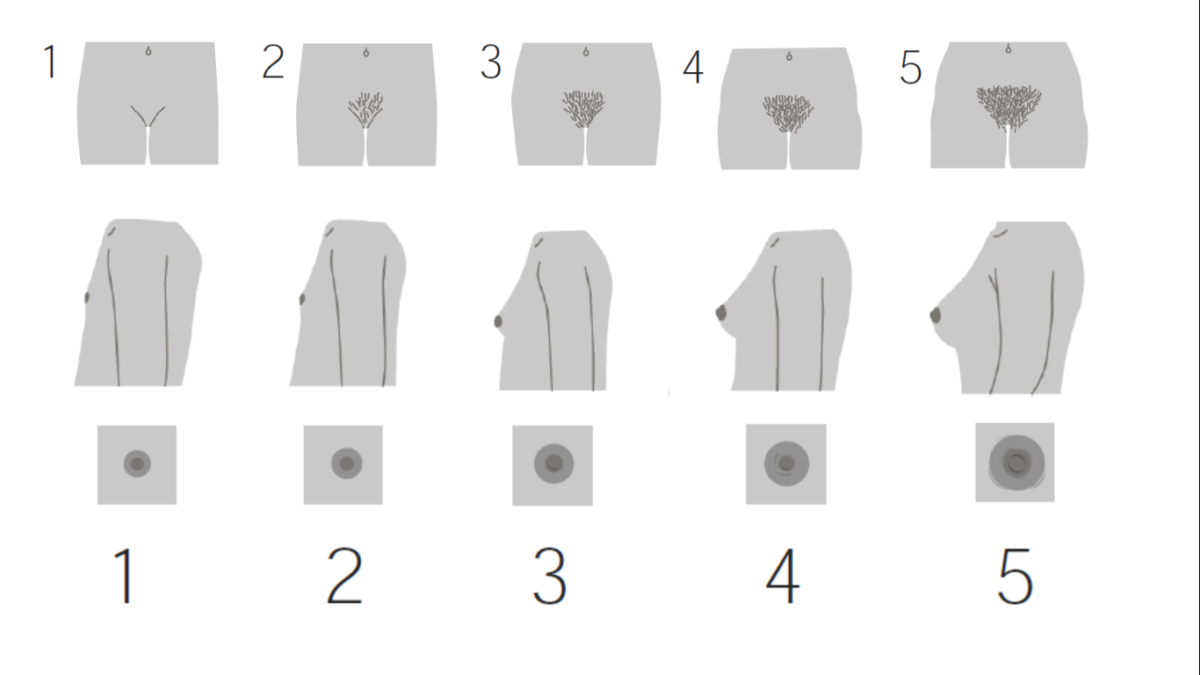
Tanner staging for girls
Image by Lecturio.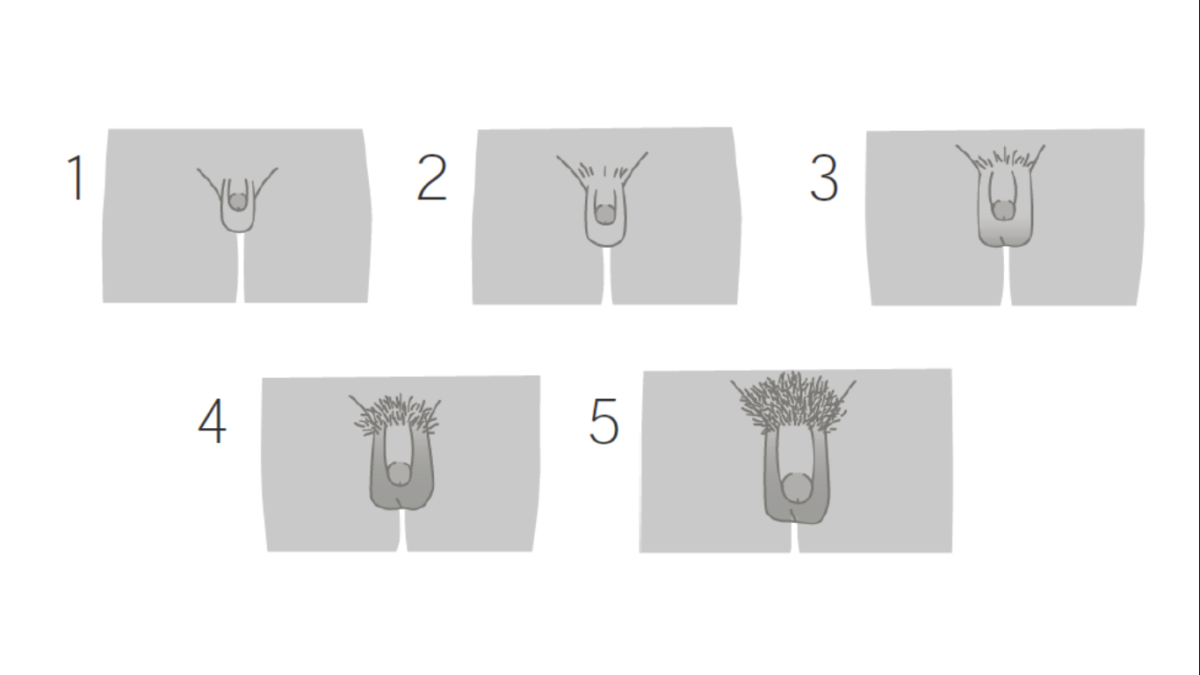
Tanner staging for boys
Image by Lecturio.Directed at the cause, such as: