The menstrual cycle is the cyclic pattern of hormonal and tissular activity that prepares a suitable uterine environment for the fertilization of an ovum and implantation of an embryo. The menstrual cycle involves both an endometrial and ovarian cycle that are dependent on one another for proper functioning. There are 2 phases of the ovarian cycle (follicular and luteal) and 3 phases of the endometrial cycle (desquamation or menses, proliferative, and secretory). The menstrual cycle is regulated by the hypothalamic-pituitary-ovarian axis via follicle-stimulating hormone (FSH) and luteinizing hormone (LH). A woman’s 1st menstrual cycle is referred to as menarche, and cycles continue until menopause.
Last updated: Dec 12, 2022
The menstrual cycle is divided into 2 components: ovarian cycle and endometrial cycle:
Ovarian cycle phases:
Endometrial cycle phases:
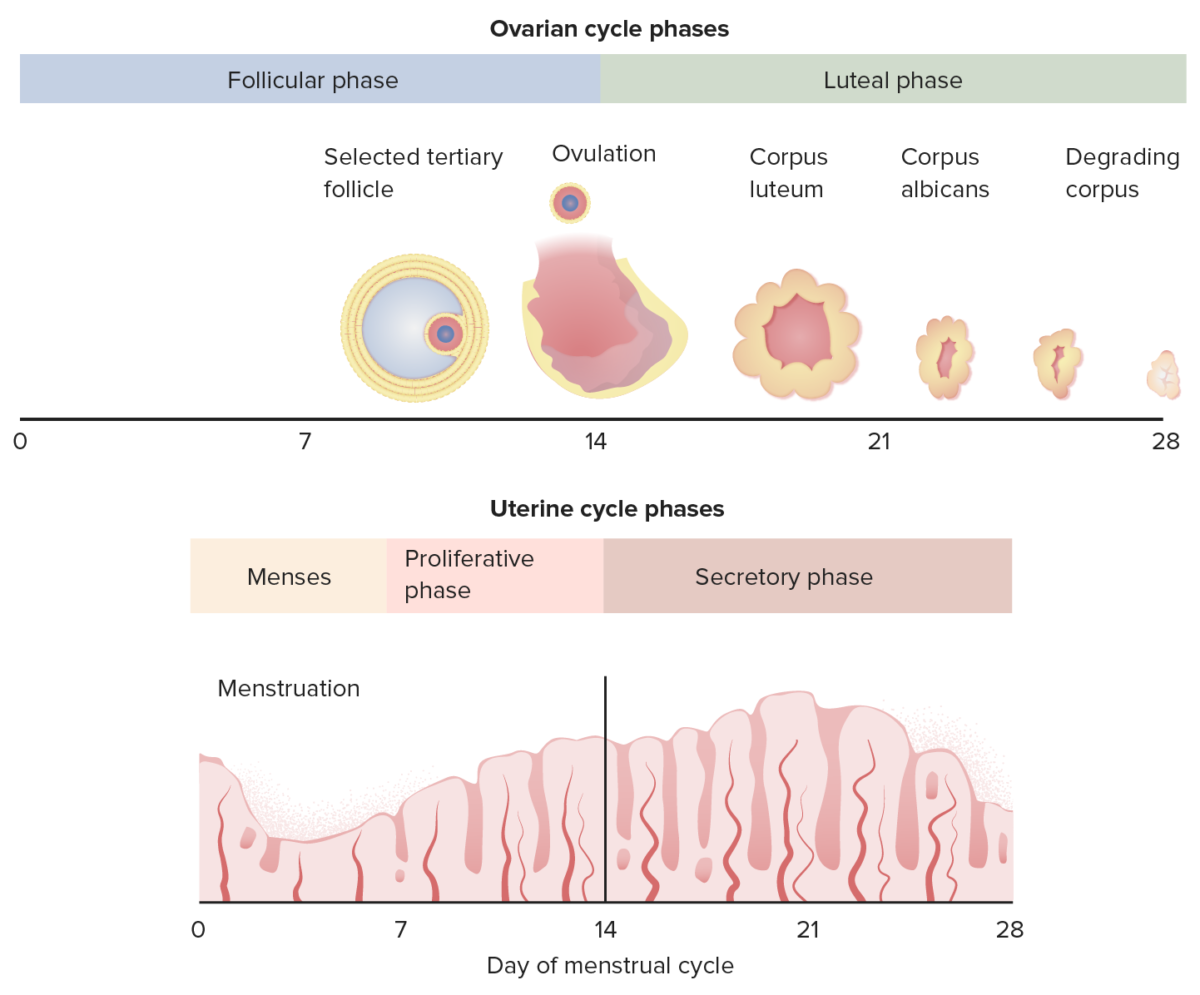
A diagram showing the correlation between the ovarian cycle and the endometrial cycle
Image by Lecturio.The menstrual cycle is regulated by the hypothalamic-pituitary-ovarian axis Hypothalamic-pituitary-ovarian axis Gonadal Hormones.
Hypothalamus Hypothalamus The hypothalamus is a collection of various nuclei within the diencephalon in the center of the brain. The hypothalamus plays a vital role in endocrine regulation as the primary regulator of the pituitary gland, and it is the major point of integration between the central nervous and endocrine systems. Hypothalamus:
Anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types:
Ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy:
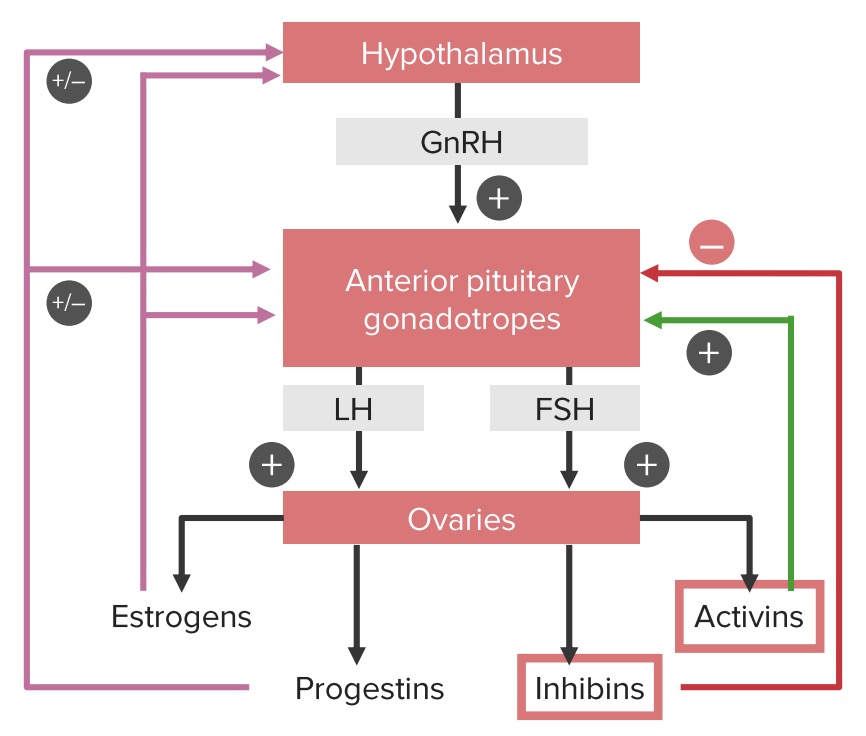
Positive and negative feedback loops of the hypothalamic-pituitary-ovarian axis:
Note that estrogens and progestins can have both a positive and a negative influence on the hypothalamus and pituitary gland, depending on the phase of the cycle. Estrogens provide negative feedback until the middle of the cycle. At this point, estrogen begins stimulating the gonadotropic cells in the pituitary, leading to the LH surge, which triggers ovulation.
LH: luteinizing hormone
FSH: follicle-stimulating hormone
GnRH: gonadotropin-releasing hormone
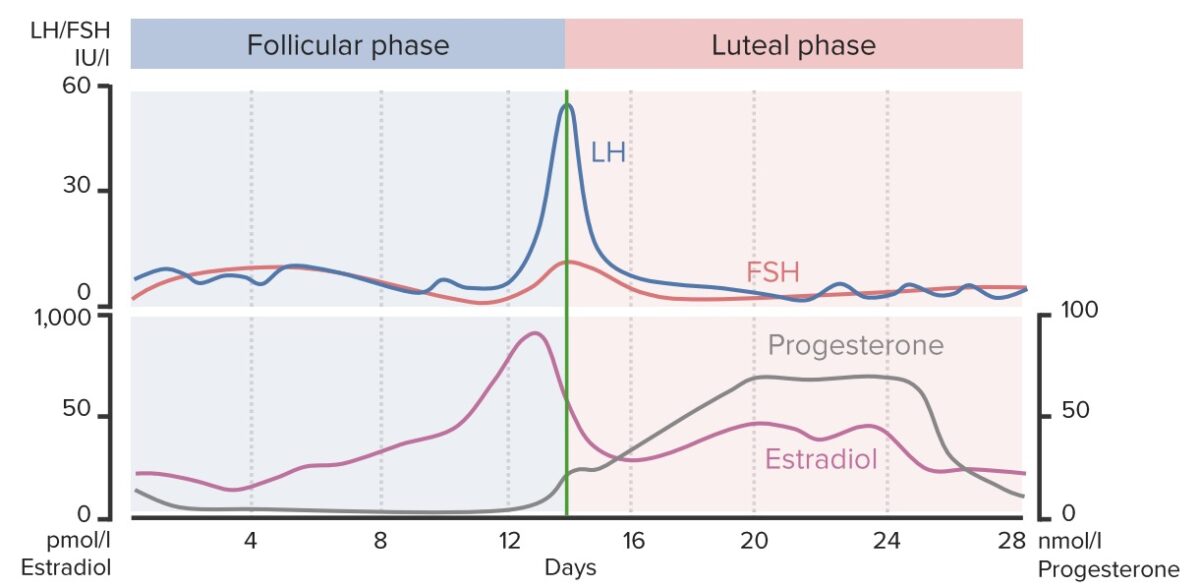
A chart showing the changing concentrations of key hormones throughout the length of the menstrual cycle: Notice the sudden rise in estradiol, LH and FSH around day 14 (ovulation), and the rise in progesterone during the luteal phase in anticipation of fertilization and implantation of the ovum.
Image by Lecturio.The phase representing the time during which the follicle (and the oocyte it contains) develop, leading up to ovulation. The follicular phase of the ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy coincides with menses and the proliferative phase of the endometrium Endometrium The mucous membrane lining of the uterine cavity that is hormonally responsive during the menstrual cycle and pregnancy. The endometrium undergoes cyclic changes that characterize menstruation. After successful fertilization, it serves to sustain the developing embryo. Embryoblast and Trophoblast Development.
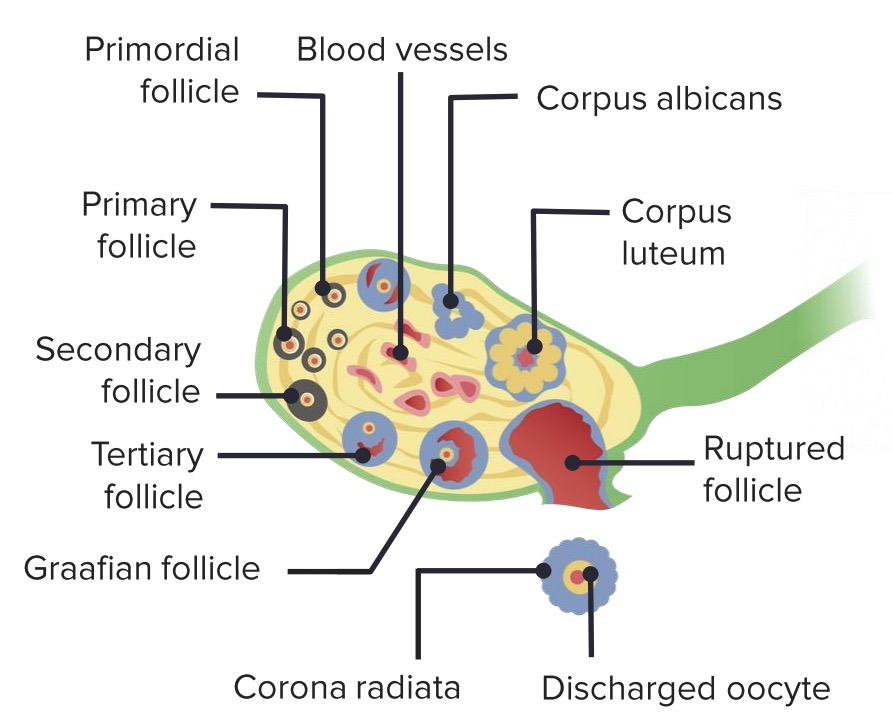
Stages of maturation of an ovarian follicle

Structure of a tertiary (antral) ovarian follicle
Image by Lecturio.The luteal phase of the ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy coincides with the secretory phase of the endometrium Endometrium The mucous membrane lining of the uterine cavity that is hormonally responsive during the menstrual cycle and pregnancy. The endometrium undergoes cyclic changes that characterize menstruation. After successful fertilization, it serves to sustain the developing embryo. Embryoblast and Trophoblast Development.
There are 3 phases of the endometrial cycle:
Day 1 of menstrual bleeding marks the beginning of the next cycle.
The following conditions are related to abnormalities of the menstrual cycle, known as abnormal uterine bleeding Abnormal Uterine Bleeding Abnormal uterine bleeding is the medical term for abnormalities in the frequency, volume, duration, and regularity of the menstrual cycle. Abnormal uterine bleeding is classified using the acronym PALM-COEIN, with PALM representing the structural causes and COEIN indicating the non-structural causes. Abnormal Uterine Bleeding ( AUB AUB Abnormal uterine bleeding is the medical term for abnormalities in the frequency, volume, duration, and regularity of the menstrual cycle. Abnormal uterine bleeding is classified using the acronym palm-coein, with palm representing the structural causes and coein indicating the non-structural causes. Abnormal Uterine Bleeding):