Ovaries are the paired gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types of the female reproductive system that contain haploid Haploid The chromosomal constitution of cells, in which each type of chromosome is represented once. Symbol: n. Basic Terms of Genetics gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy, just posterior to the broad ligament Broad Ligament A broad fold of peritoneum that extends from the side of the uterus to the wall of the pelvis. Uterus, Cervix, and Fallopian Tubes: Anatomy, and are connected to the pelvic sidewall laterally by the suspensory ligament of the ovary and to the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy medially by the utero-ovarian ligament. These organs function to secrete hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types (estrogen and progesterone Progesterone The major progestational steroid that is secreted primarily by the corpus luteum and the placenta. Progesterone acts on the uterus, the mammary glands and the brain. It is required in embryo implantation; pregnancy maintenance, and the development of mammary tissue for milk production. Progesterone, converted from pregnenolone, also serves as an intermediate in the biosynthesis of gonadal steroid hormones and adrenal corticosteroids. Gonadal Hormones) and to produce the female germ cells Germ Cells The reproductive cells in multicellular organisms at various stages during gametogenesis. Gametogenesis (oocytes), which are expelled and then “captured” by the uterine tubes. The primary blood supply to the ovary is provided by the ovarian artery, a direct branch of the abdominal aorta Abdominal Aorta The aorta from the diaphragm to the bifurcation into the right and left common iliac arteries. Posterior Abdominal Wall: Anatomy; the ovarian artery anastomoses with the ascending branch of the uterine artery Uterine Artery A branch arising from the internal iliac artery in females, that supplies blood to the uterus. Uterus, Cervix, and Fallopian Tubes: Anatomy, providing excellent collateral blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure.
Last updated: Nov 19, 2024
The ovaries are the female gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types, located within the pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy as paired structures. The ovaries contain haploid Haploid The chromosomal constitution of cells, in which each type of chromosome is represented once. Symbol: n. Basic Terms of Genetics gametes known as oocytes.
Weeks 5–10:
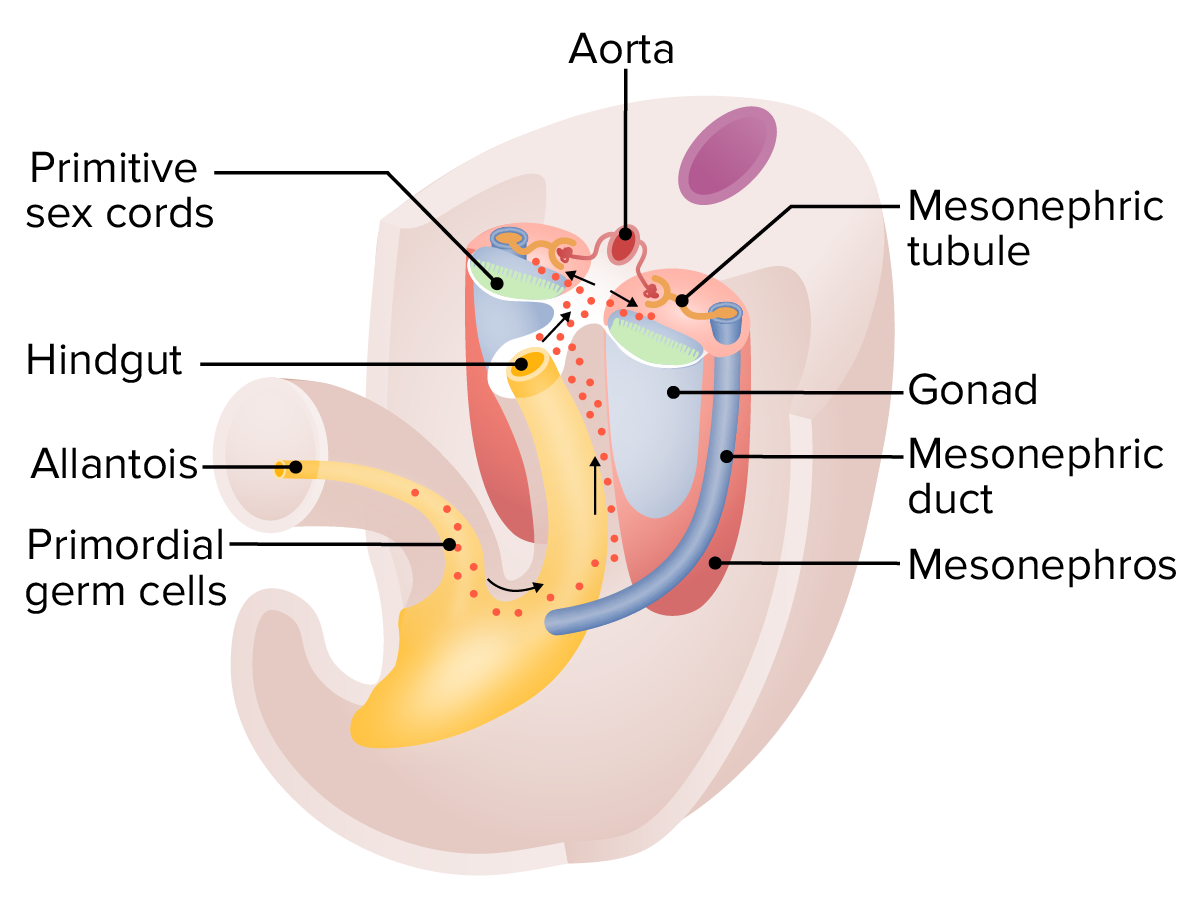
Migration of the primordial germ cells at around 5 weeks:
These germ cells begin as epiblast cells and start developing within the yolk sac. The cells then migrate down the allantois, along the dorsal mesentery of the hindgut, and then invade the gonadal ridges, which are beginning to form the early gonads.
Weeks 10–20:
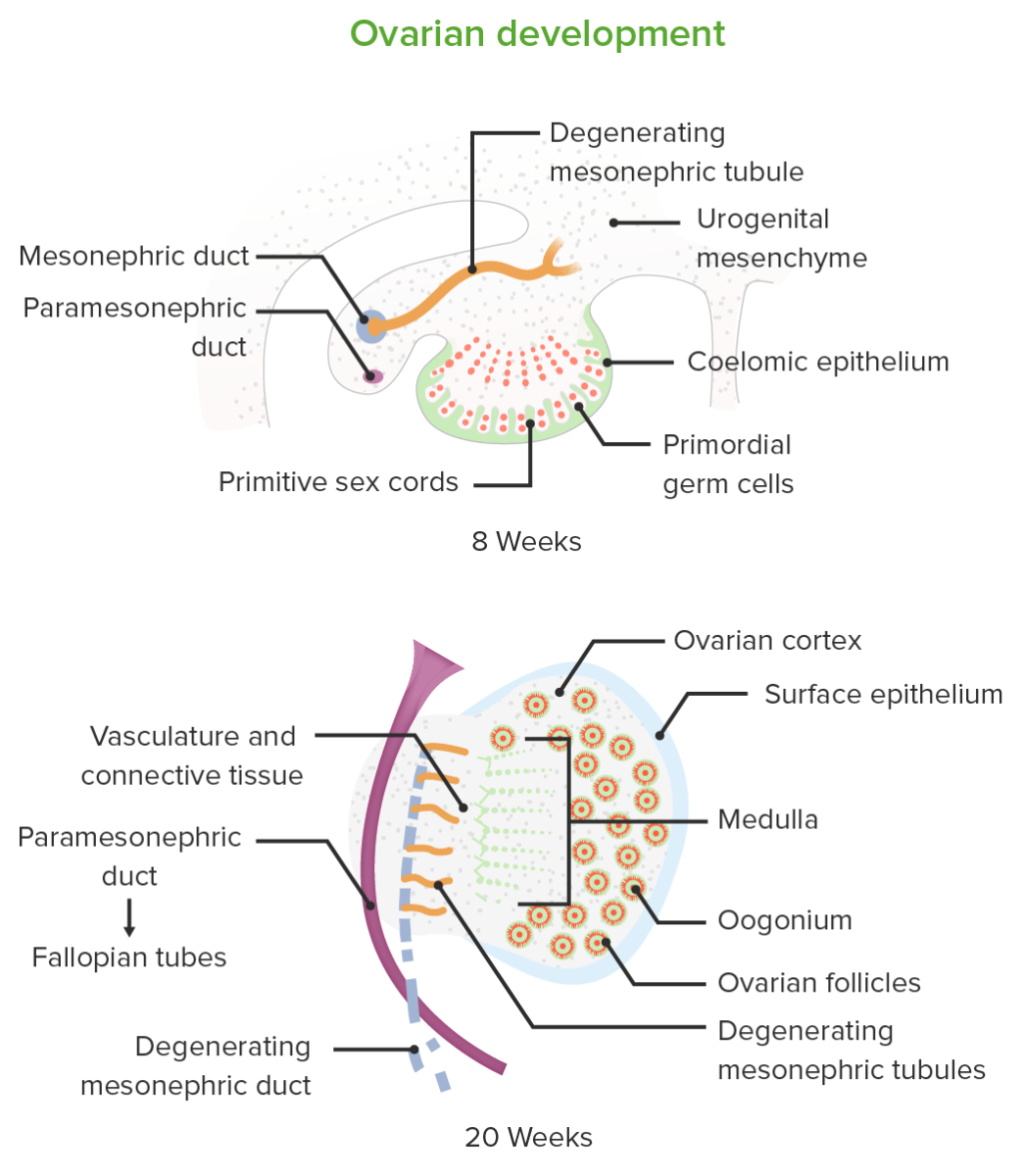
Embryologic development of the ovaries
Image by Lecturio.
Posterior superior view of the the female pelvic anatomy
Image by Lecturio.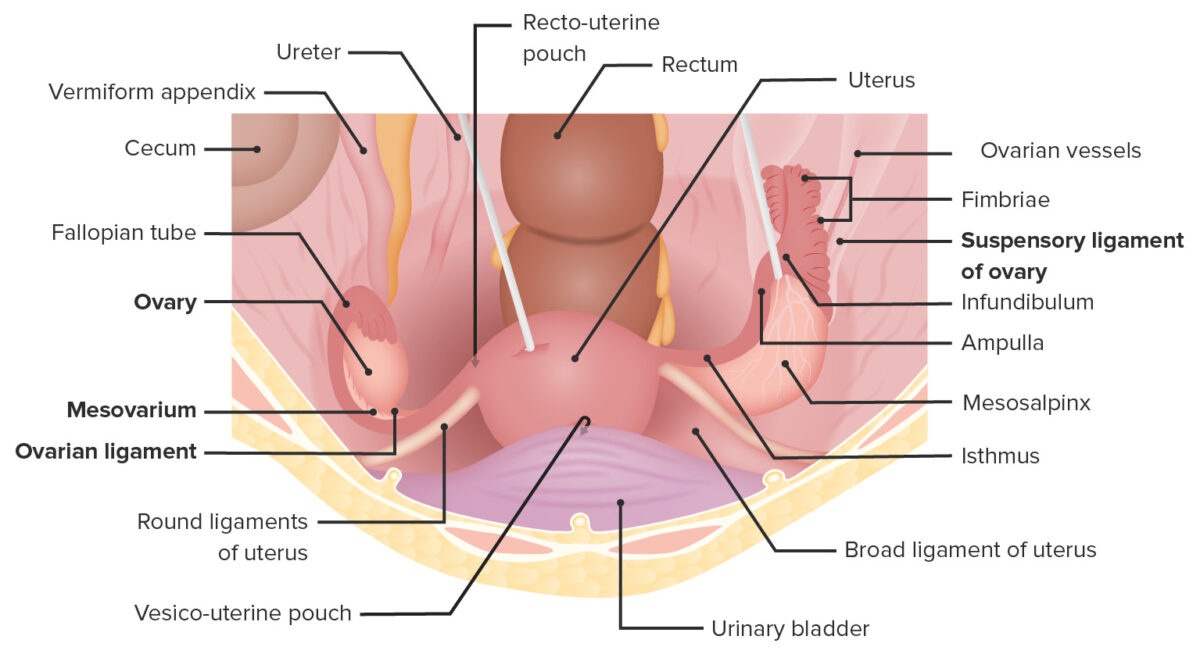
Superior view of the female pelvis depicting the uterus in situ, its supporting ligaments, and its relation to the ovaries and neighboring organs
Image by Lecturio. License: CC BY-NC-SA 4.0Ovaries are suspended within the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy between the pelvic sidewall and uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy via the several important ligaments.
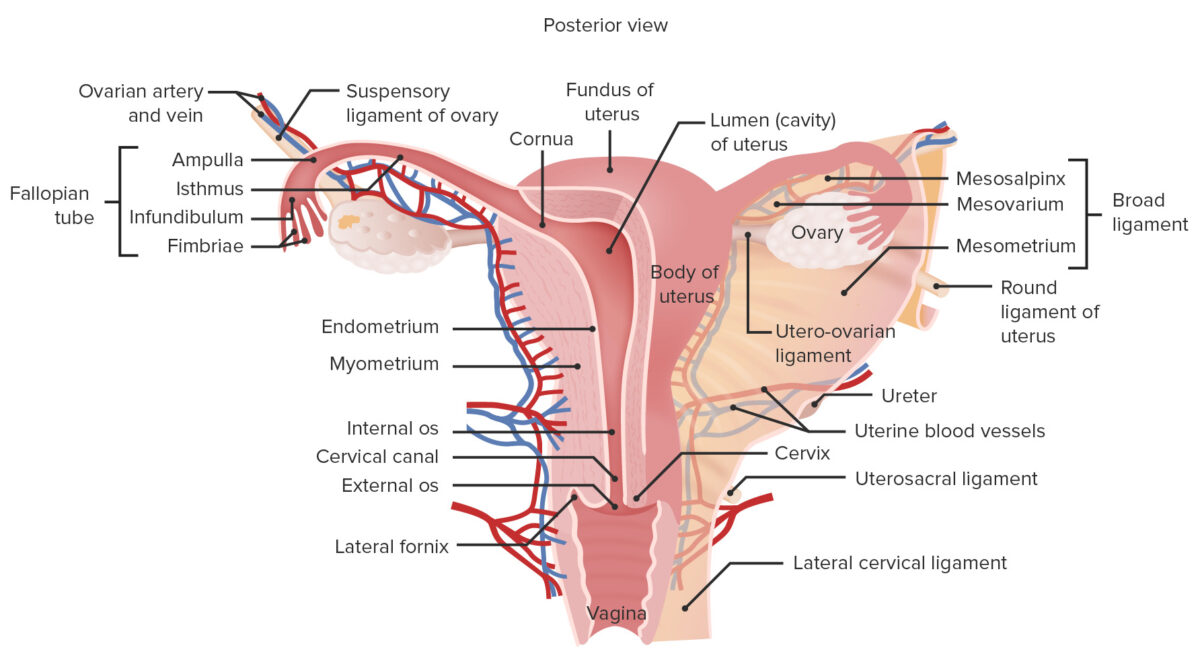
Gross anatomy of the female reproductive system
Image by Lecturio.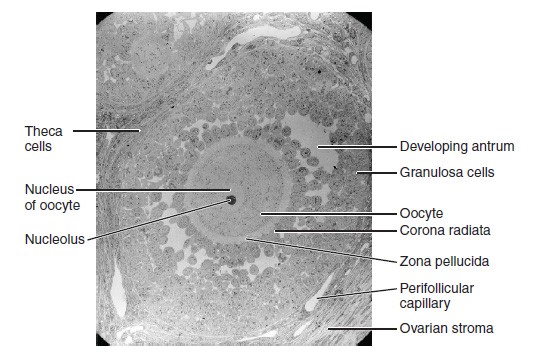
Electron micrograph (× 1100) of a secondary follicle
Image: “Folliculogenesis” by Phil Schatz. License: CC BY 4.0Oogenesis Oogenesis The process of germ cell development in the female from the primordial germ cells through oogonia to the mature haploid ova (ovum). Gametogenesis is the process of ovum production from primordial germ cells Primordial germ cells Gametogenesis.
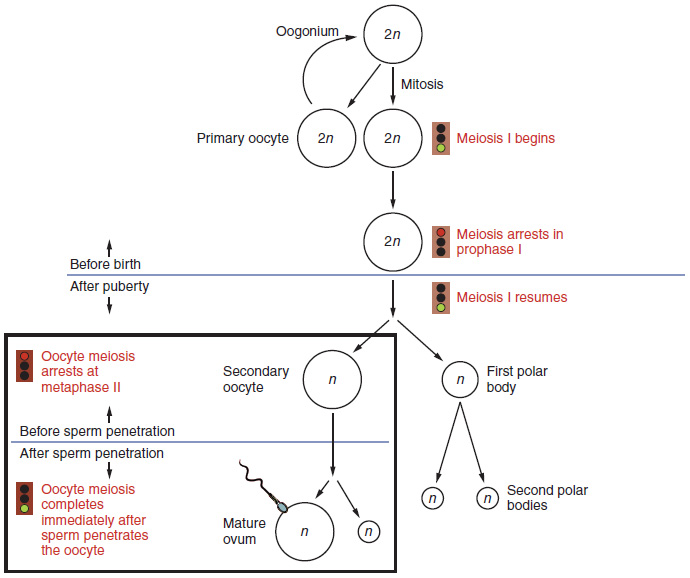
The process of oogenesis
Image: “Oogenesis” by Phil Schatz. License: CC BY 4.0Folliculogenesis is a complex process in which an ovarian follicle, containing an oocyte, matures through several stages.
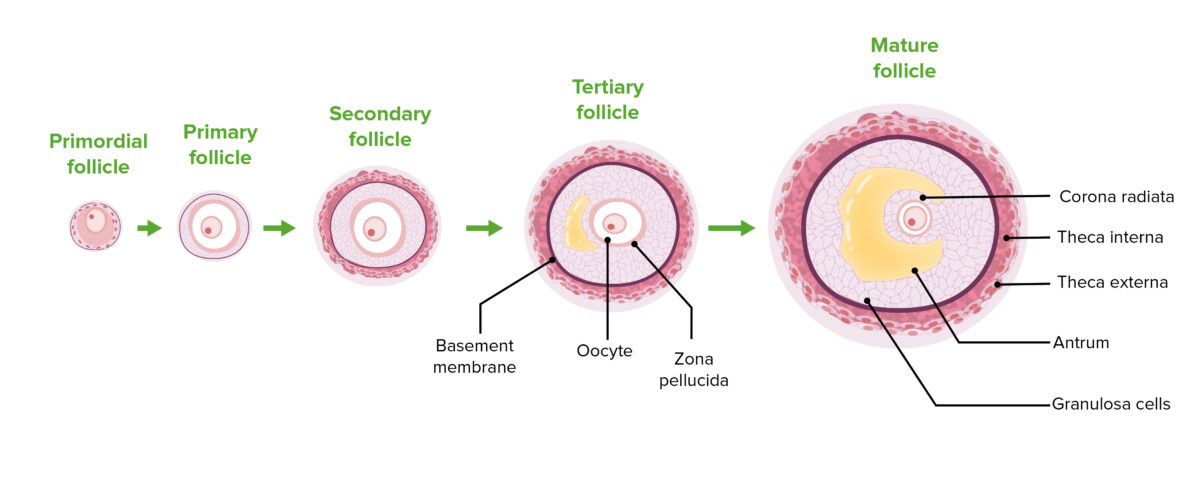
The stages of folliculogenesis:
Note the progression of follicular cell proliferation, thecal cell differentiation, and antrum enlargement.
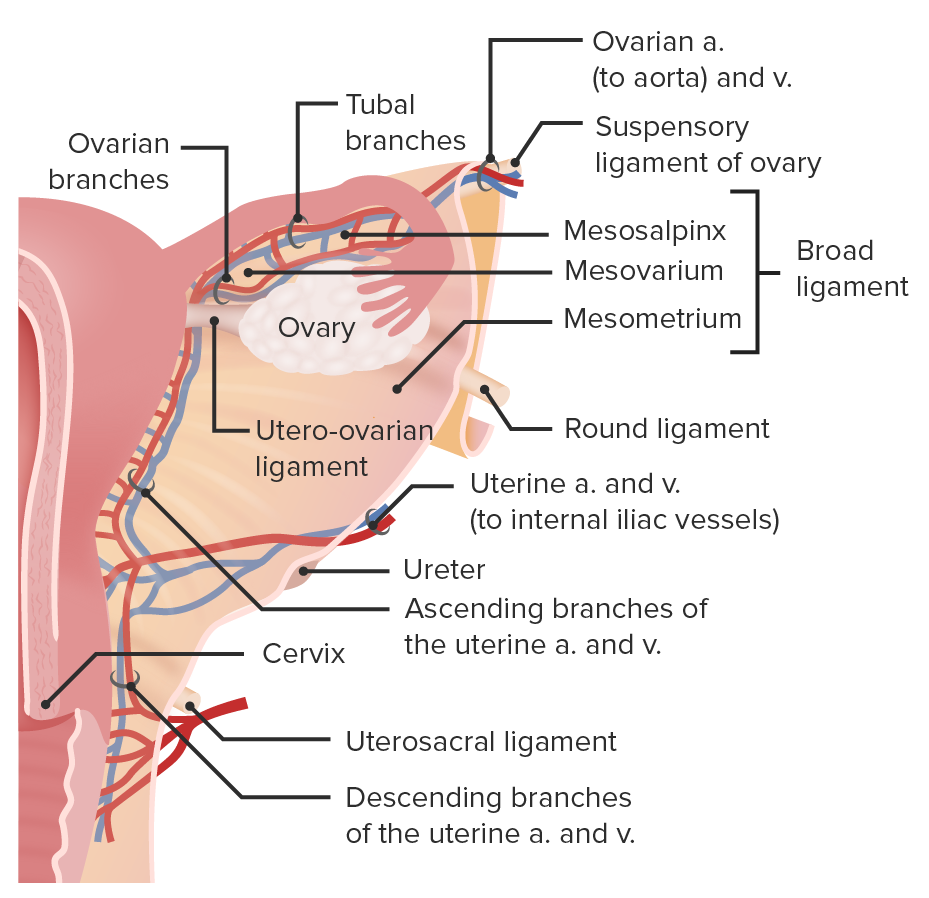
Blood supply and venous drainage to the ovary
Image by Lecturio.