Gametogenesis is the development of gametes from primordial germ cells. This process differs between the sexes. In males, spermatogenesis produces spermatozoa. In females, oogenesis results in an ovum. The process starts with the migration of primordial germ cells from the yolk sac Yolk Sac The first of four extra-embryonic membranes to form during embryogenesis. In reptiles and birds, it arises from endoderm and mesoderm to incorporate the egg yolk into the digestive tract for nourishing the embryo. In placental mammals, its nutritional function is vestigial; however, it is the source of intestinal mucosa; blood cells; and germ cells. It is sometimes called the vitelline sac, which should not be confused with the vitelline membrane of the egg. Embryoblast and Trophoblast Development to the gonadal ridge Gonadal ridge Development of the Urogenital System. Oogenesis starts during the embryonic and fetal periods, whereas spermatogenesis starts at puberty Puberty Puberty is a complex series of physical, psychosocial, and cognitive transitions usually experienced by adolescents (11-19 years of age). Puberty is marked by a growth in stature and the development of secondary sexual characteristics, achievement of fertility, and changes in most body systems. Puberty. However, the phases of gametogenesis are similar, with germ cells progressing through mitosis Mitosis A type of cell nucleus division by means of which the two daughter nuclei normally receive identical complements of the number of chromosomes of the somatic cells of the species. Cell Cycle, meiosis I Meiosis I Following DNA replication, meiosis I creates 2 daughter cells containing half the genetic information of the mother cell (1n) but the same number of chromosomes (2c) by segregating sister chromatids into the same daughter cell Meiosis, meiosis II Meiosis II Meiosis II is a cellular division event wherein the number of chromosomes in the daughter cells is halved from that of the mother cell. Meiosis II: similar to meiosis I but not preceded by interphase (DNA replication) Meiosis, and maturation. This process results in gametes that are haploid Haploid The chromosomal constitution of cells, in which each type of chromosome is represented once. Symbol: n. Basic Terms of Genetics, with 23 chromosomes Chromosomes In a prokaryotic cell or in the nucleus of a eukaryotic cell, a structure consisting of or containing DNA which carries the genetic information essential to the cell. DNA Types and Structure.
Last updated: Sep 1, 2022
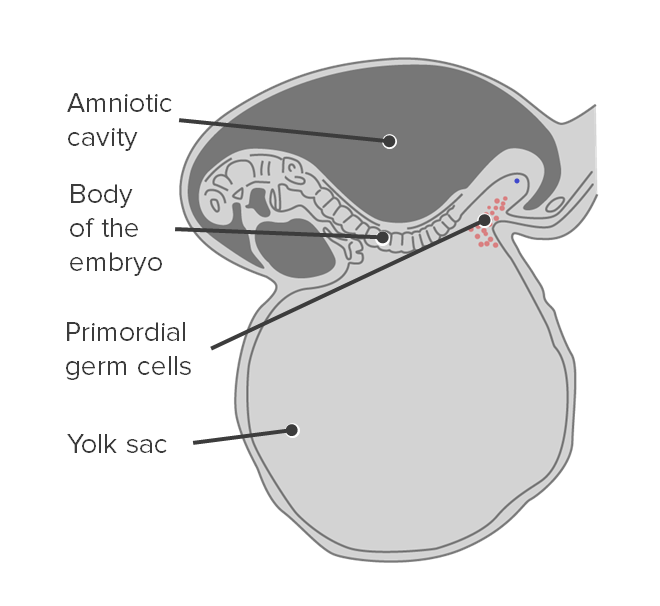
Origin of primordial germ cells:
Primordial germ cells originate in the yolk sac.
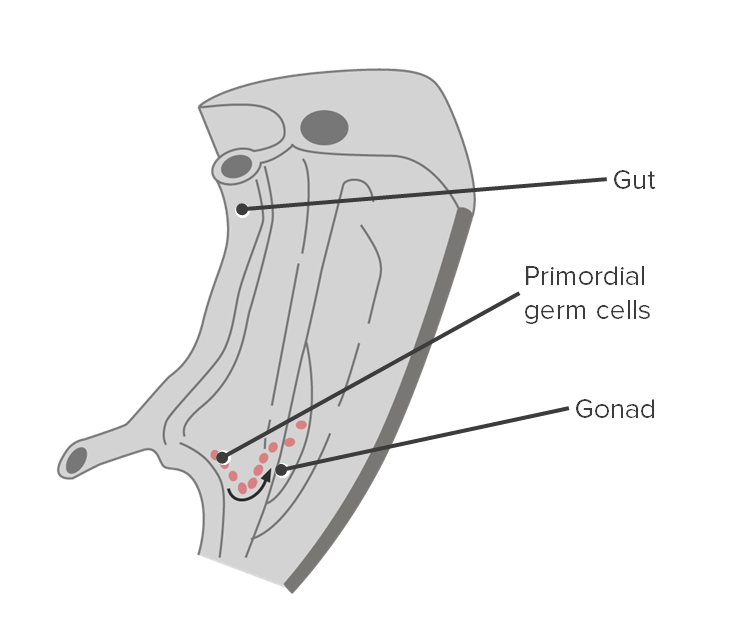
Migration of primordial germ cells:
Primordial germ cells migrate along the hindgut to reach the gonadal ridge.
Cross section showing the migration of primordial germ cells to the gonads
Image by Lecturio.
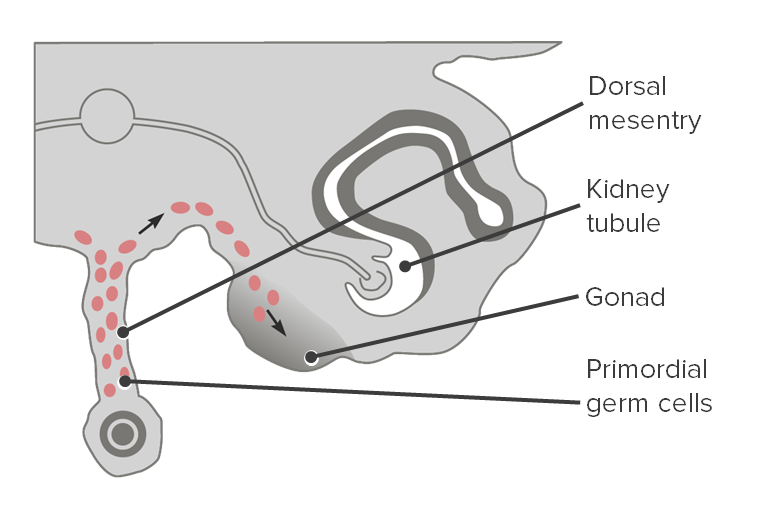
Primordial germ cells become associated with primary sex cords
Image by Lecturio.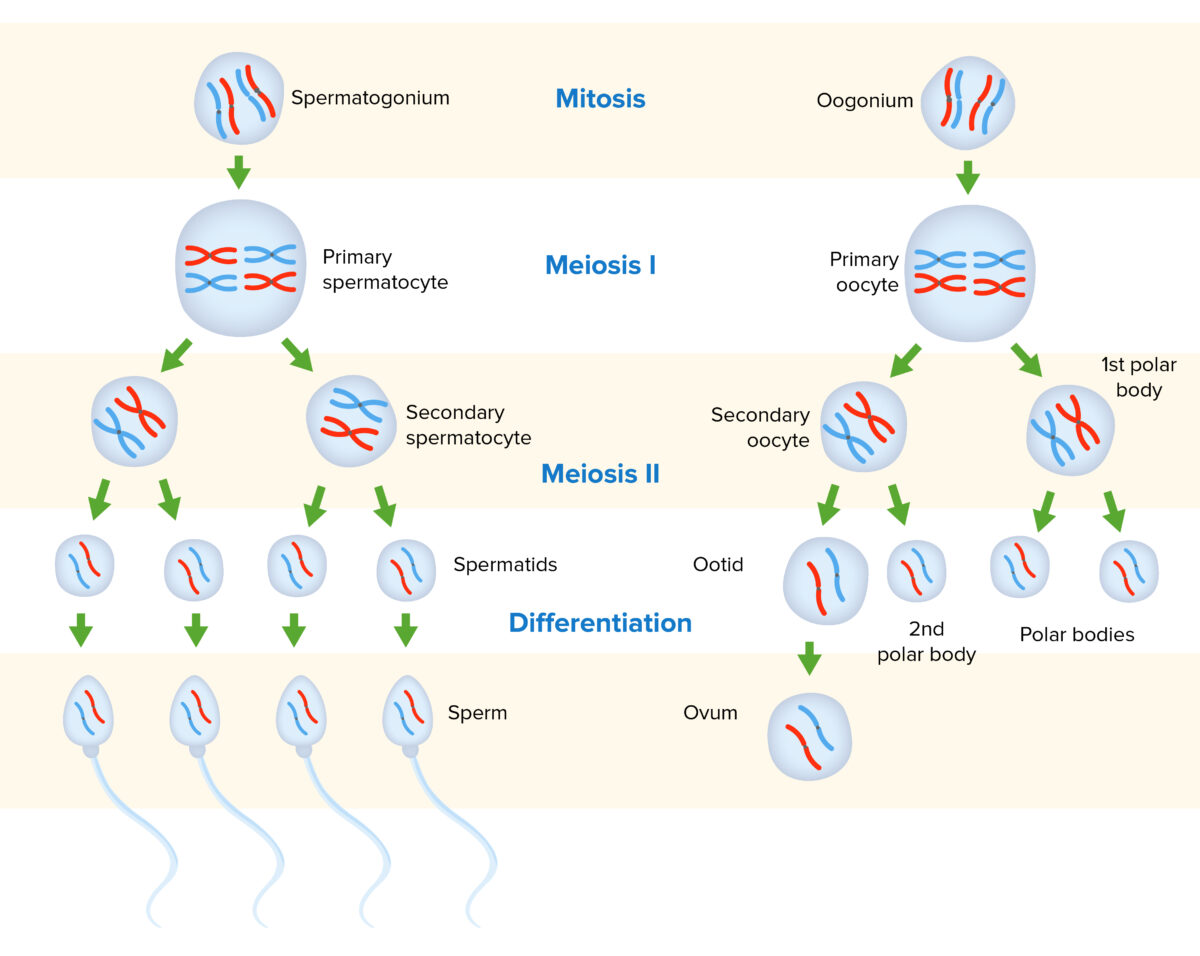
Gametogenesis in males and females:
Diploid gametogonia undergo mitosis. Some daughter cells will remain as gametogonia, while others differentiate into primary gametocytes. From there, meiosis I occurs, resulting in secondary gametocytes that are haploid. Meiosis II leads to gametids, with 1 representative strand of DNA from each chromosome. Gametids undergo a separate process for differentiation/maturation to produce mature gametes.
Oogenesis is the process of ovum production from PGCs.
Folliculogenesis Folliculogenesis Ovaries: Anatomy is a complex process in which an ovarian follicle, containing an oocyte, matures through several stages.
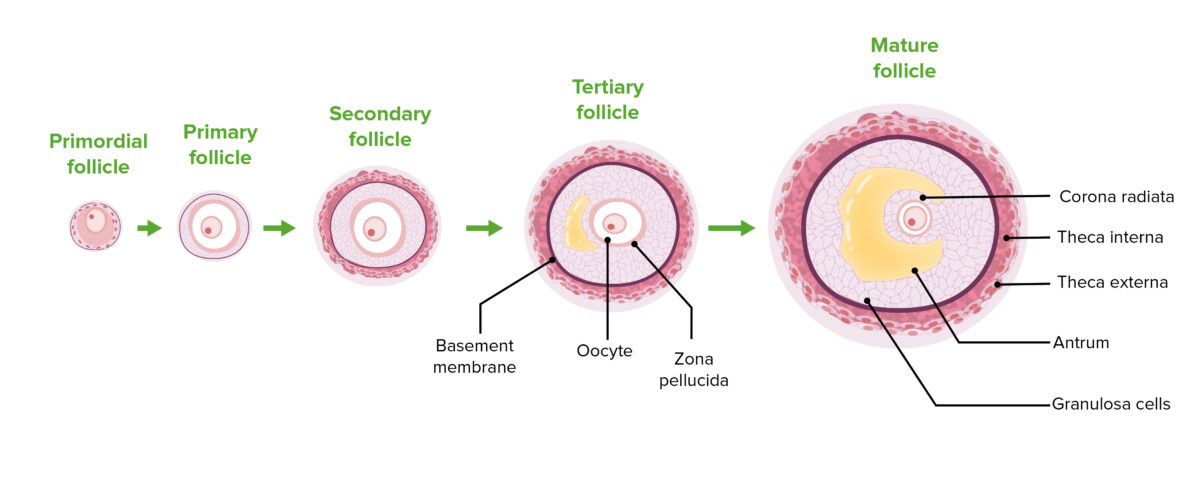
The stages of folliculogenesis:
Note the progression of follicular cell proliferation, thecal cell differentiation, and antrum enlargement.
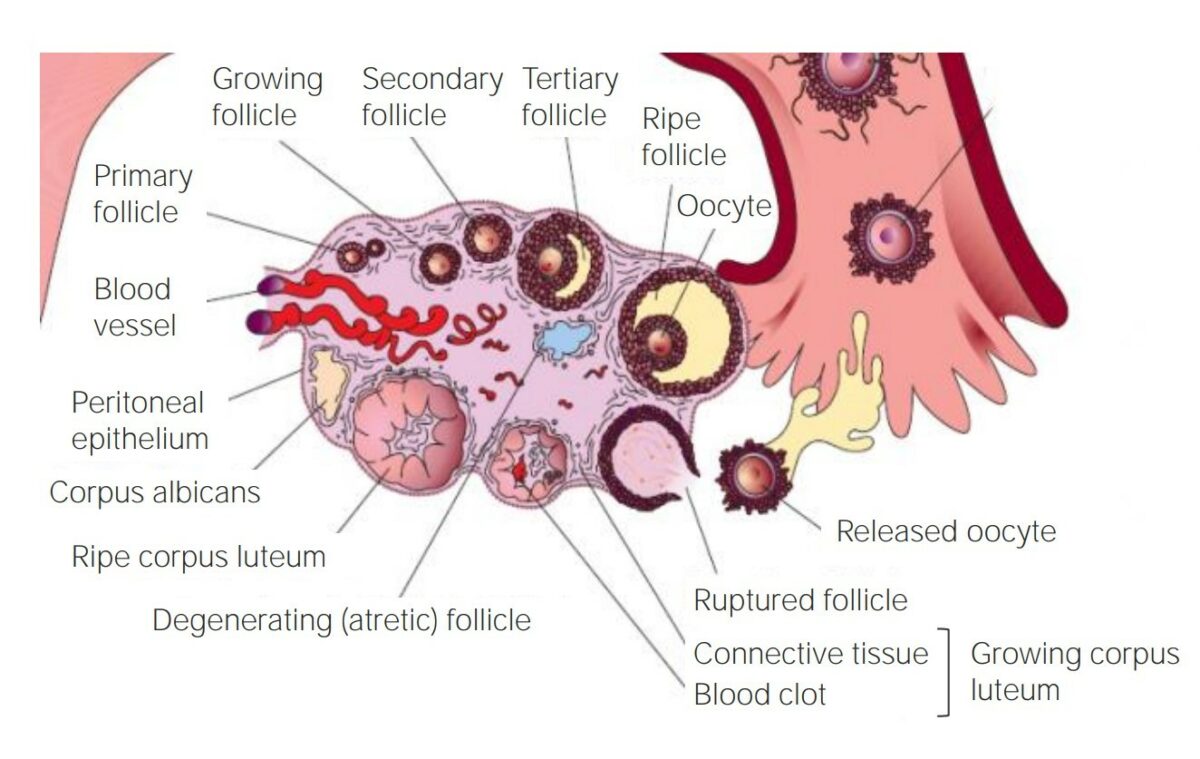
The development of a follicle within the ovary
Image by Lecturio.Spermatogenesis is the process of sperm production from PGCs.
Overview:
Sertoli cells Sertoli Cells Supporting cells projecting inward from the basement membrane of seminiferous tubules. They surround and nourish the developing male germ cells and secrete androgen-binding protein and hormones such as anti-mullerian hormone. The tight junctions of sertoli cells with the spermatogonia and spermatocytes provide a blood-testis barrier. Testicles: Anatomy:
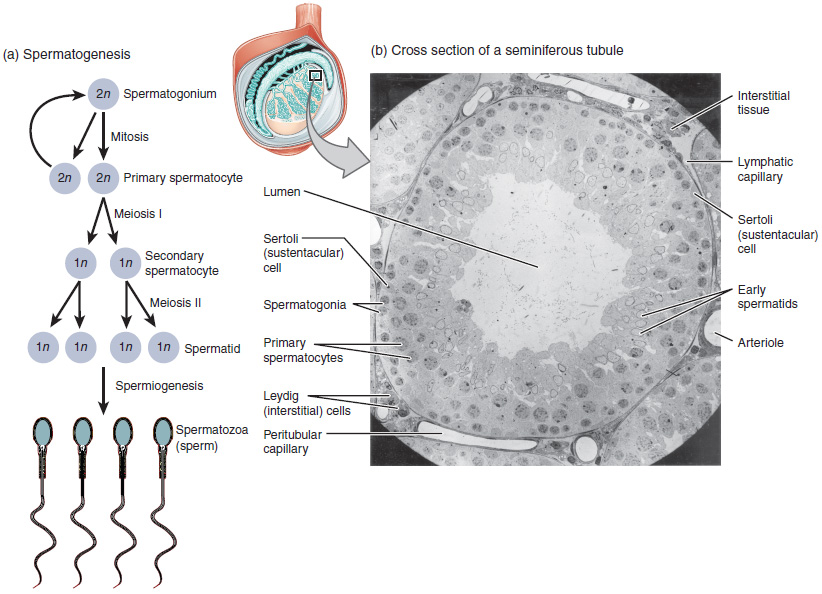
The process of spermatogenesis as the cells progress from primary spermatocytes to secondary spermatocytes to spermatids to sperm
Image: “Illustration from Anatomy & Physiology, Connexions” by OpenStax College. License: CC BY 4.0Spermiogenesis results in characteristic morphologic changes associated with spermatozoa.
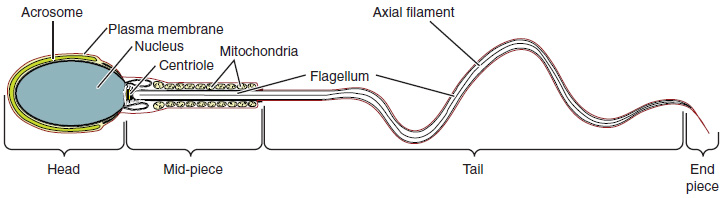
Structure of sperm
Image: “Structure of Sperm: Sperm cells are divided into a head, containing DNA; a mid-piece, containing mitochondria; and a tail, providing motility. The acrosome is oval and somewhat flattened.” by OpenStax College. License: CC BY 4.0