The testicles, also known as the testes or the male gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types, are a pair of egg-shaped glands suspended within the scrotum. The testicles have multiple layers: an outer tunica vaginalis, an intermediate tunica albuginea Tunica albuginea Penis: Anatomy, and an innermost tunica vasculosa. The testicles are composed of testicular lobules Lobules Breasts: Anatomy (contain interstitial tissue) and seminiferous tubules (produce spermatozoa). Blood supply to the testicles is primarily provided by the testicular artery. Venous drainage is through testicular veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology.
Last updated: Nov 19, 2024
Testes Testes Gonadal Hormones (the male gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types) are responsible for the production of sperm and testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens:
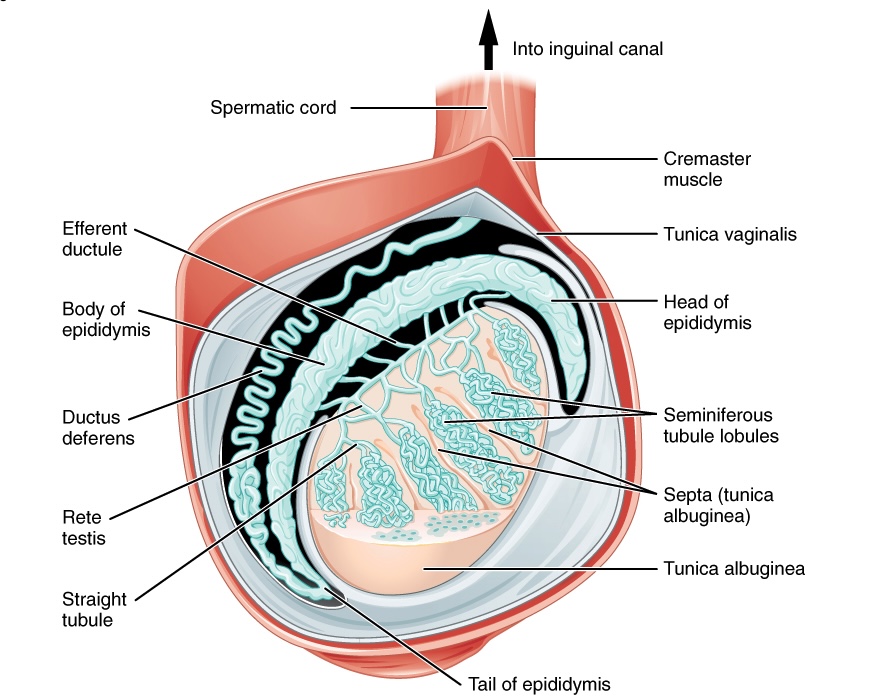
Various layers and structures comprising the testes:
Note the suspension from the spermatic cord, which permits temperature regulation.
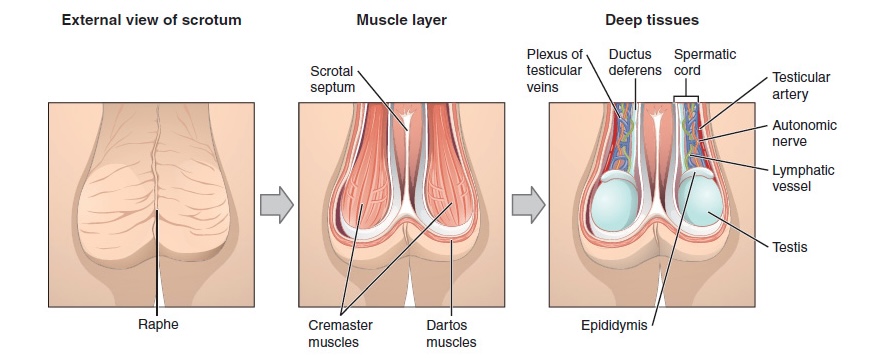
External scrotal view:
The central raphe on the far left represents the “seam” where the genital tubercles fused in development. In the central image, note the cremaster and dartos muscles, which are important for temperature regulation. On the right, note a deep layer demonstrating the external testes, epididymis, and neurovasculature.
Blood vessels, lymphatics, and the genital ducts enter the mediastinum Mediastinum The mediastinum is the thoracic area between the 2 pleural cavities. The mediastinum contains vital structures of the circulatory, respiratory, digestive, and nervous systems including the heart and esophagus, and major thoracic vessels. Mediastinum and Great Vessels: Anatomy of the testis and give rise to numerous lobules Lobules Breasts: Anatomy composed of seminiferous tubules and interstitial tissue:
The epididymis is posterolateral to the testis and consists of 3 sections:
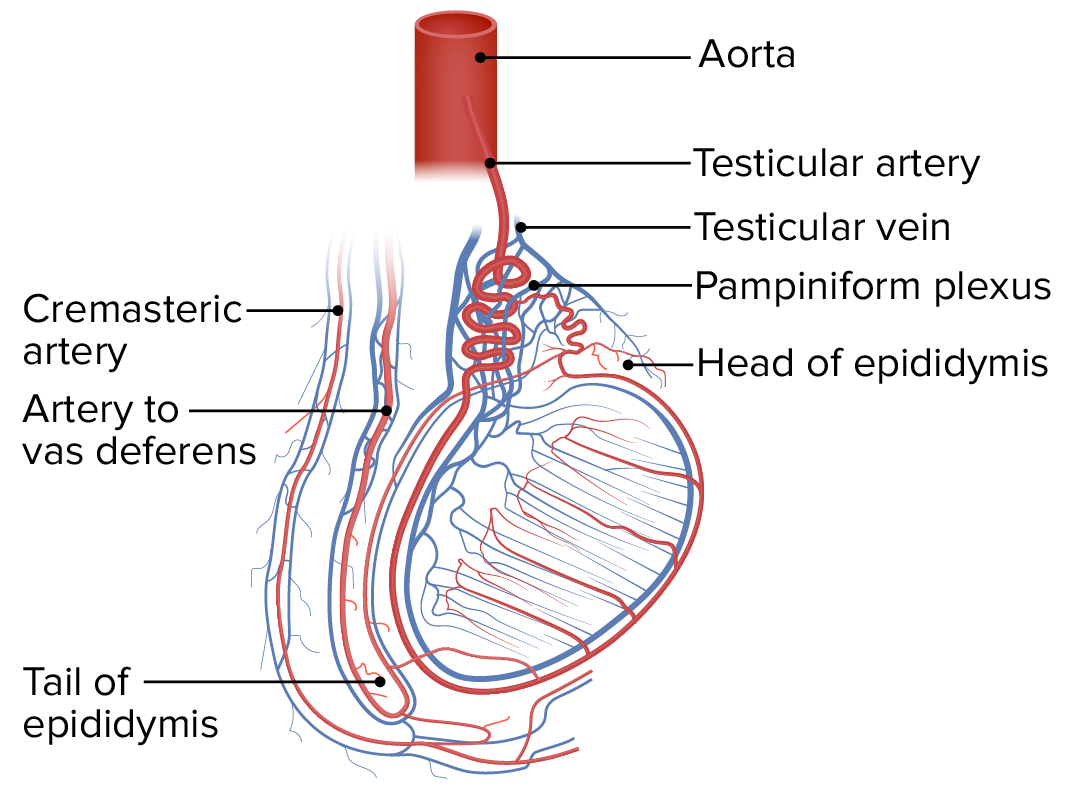
The robust vasculature of the testis and surrounding structures:
Note the largest arterial supply is the testicular artery, arising from the aorta. Also, note the large testicular vein and the pampiniform plexus.
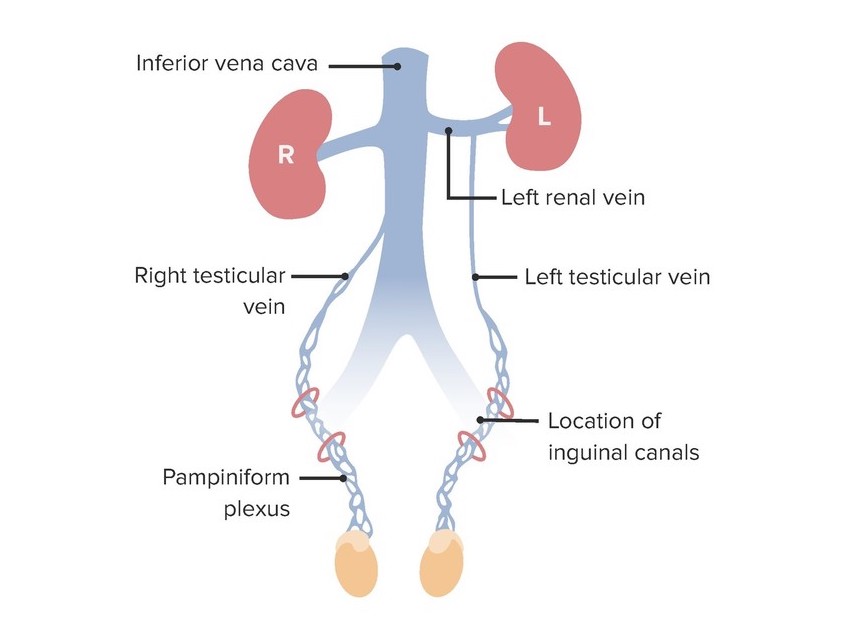
Venous drainage of the testes demonstrating the different routes of venous emptying between the left testicular vein and the right testicular vein:
Note the left testicular vein drains into the left renal vein, but the right testicular vein drains directly into the inferior vena cava.
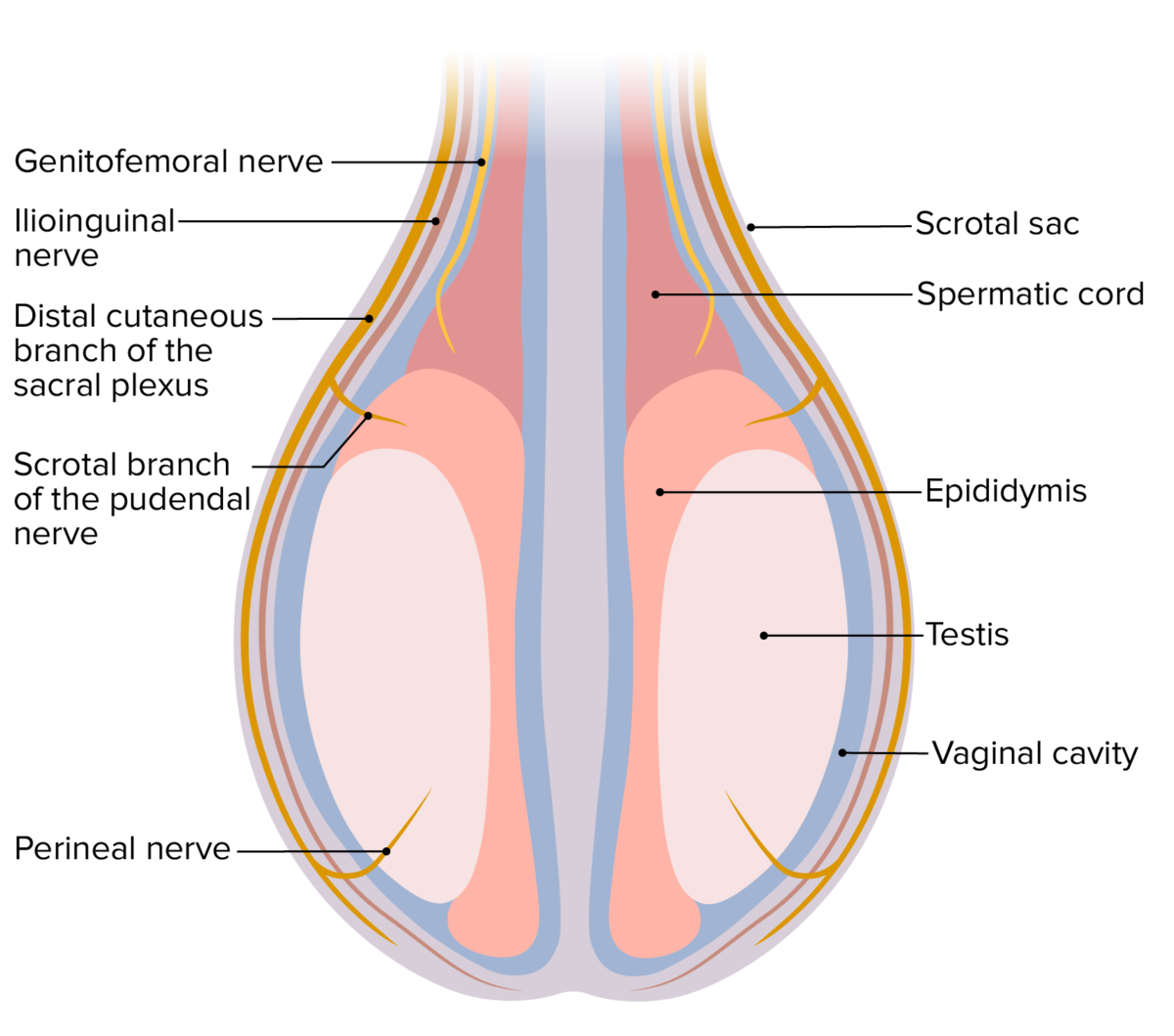
Nerve supply to the testes
Image by Lecturio.