Bacteroides is a genus of opportunistic, anaerobic, gram-negative bacilli Bacilli Shigella. Bacteroides fragilis is the most common species involved in human disease and is part of the normal flora of the large intestine Large intestine The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy. Infection most commonly occurs when the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy wall is breached and bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology enter the peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy, which can cause intra-abdominal infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease and intra-abdominal abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease formation. Management involves antibiotics and abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease drainage.
Last updated: Mar 28, 2025
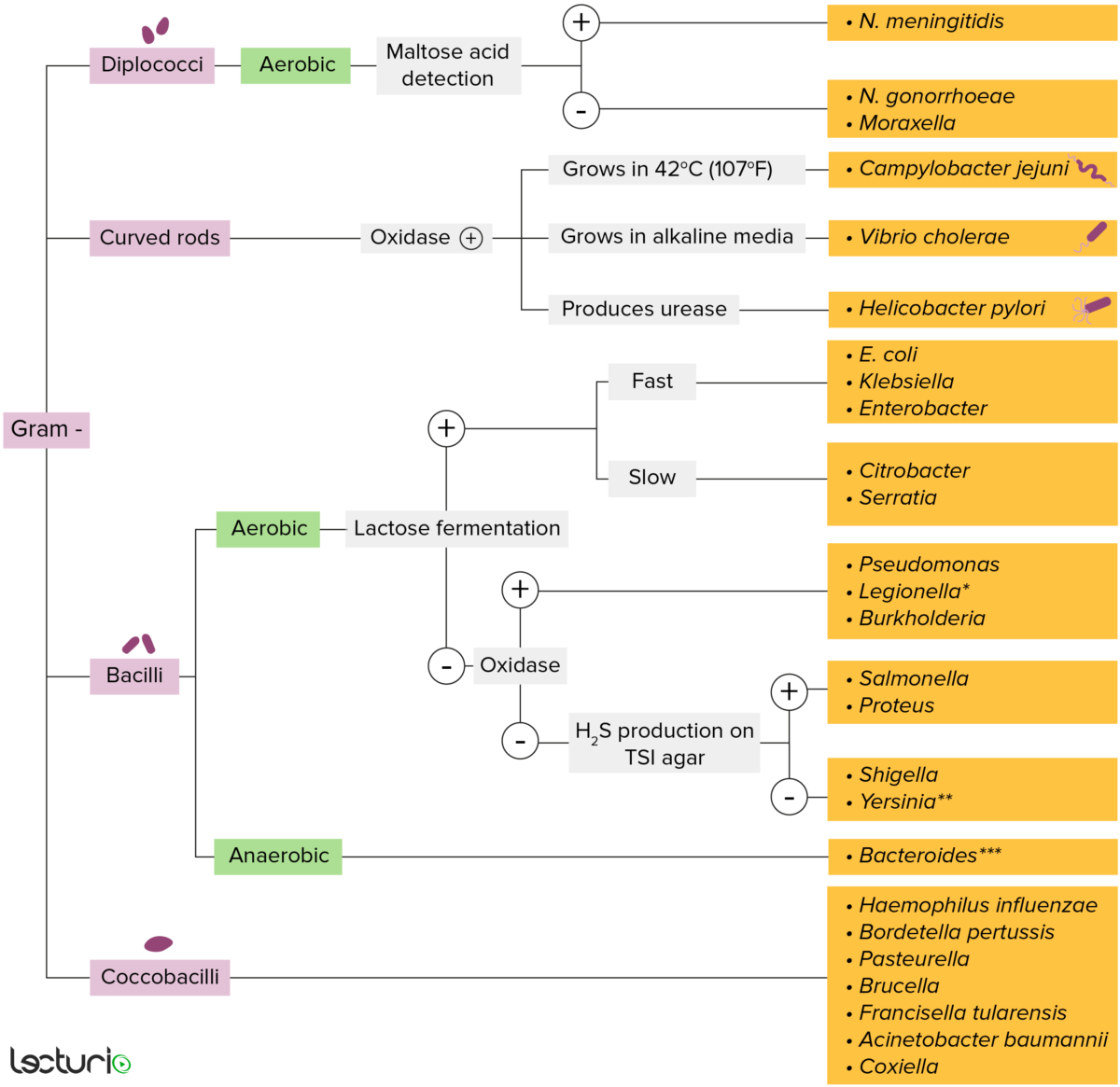
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media
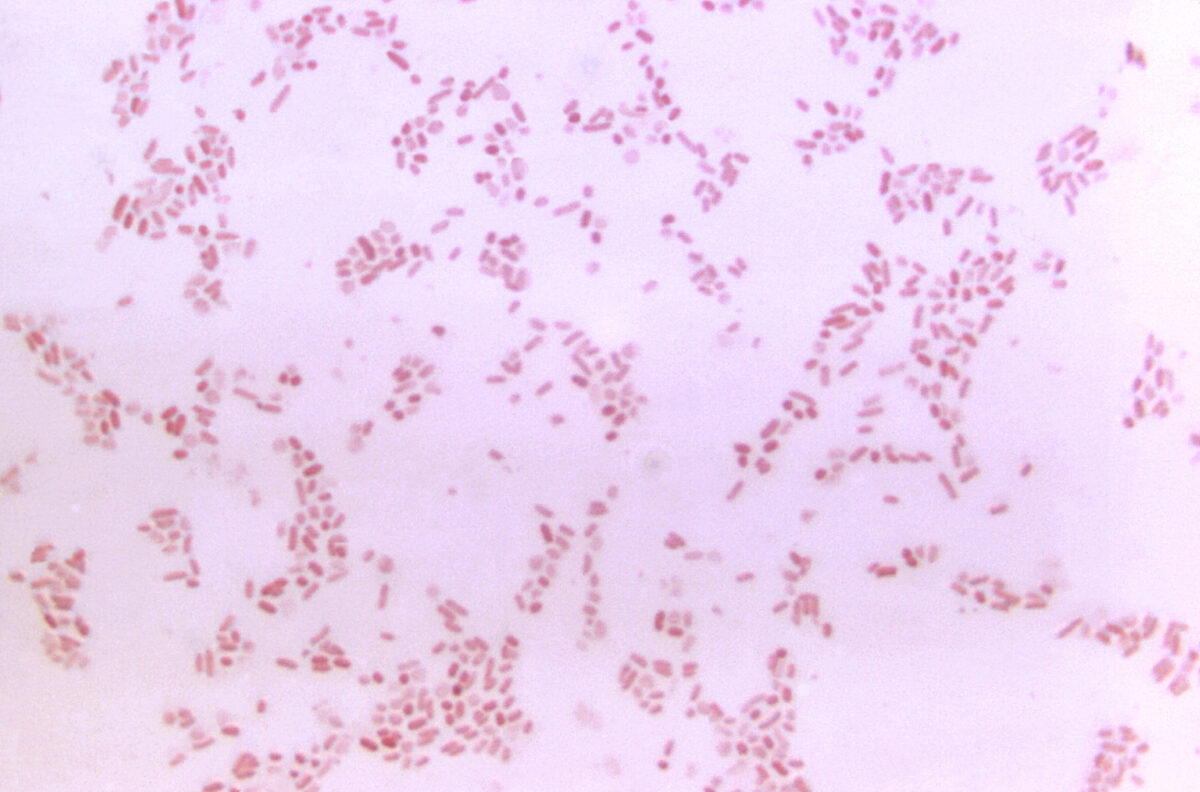
Micrograph of Bacteroides
Photomicrograph depicts the gram-negative bacterium Bacteroides fragilis.
Transmission and infection from the translocation of bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology from mucosal surfaces to other tissues may be due to:
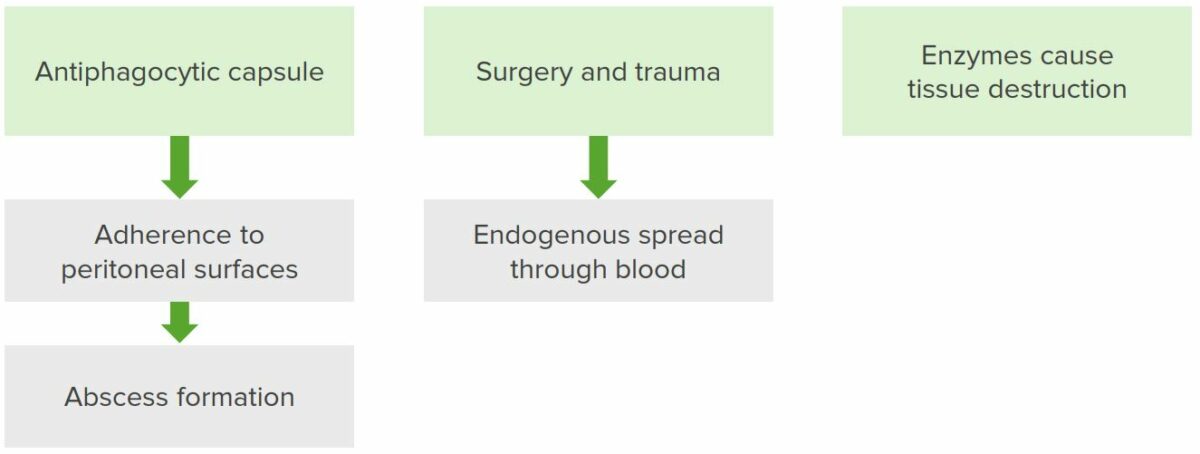
Pathogenesis of Bacteroides fragilis
The pathogen contains an antiphagocytic capsule, which adheres to the peritoneal surface. This results in abscess formation. Surgery and trauma accentuate the problem since they disrupt the abscess, allowing for the endogenous spread of the organism into the bloodstream. When this occurs, the pathogen releases degradative enzymes that destroy the host’s cells.
Bacteroides fragilis (B. fragilis) is naturally found in the large intestines as part of the natural flora. B. fragilis is an opportunistic pathogen Opportunistic pathogen Moraxella that rarely infects the gastrointestinal system, more often causing disease when bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology escape the large intestine Large intestine The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy.
| Condition | Characteristics | Infection type |
|---|---|---|
| Intra-abdominal | Intra-abdominal infection |
|
| Perforated appendicitis Appendicitis Appendicitis is the acute inflammation of the vermiform appendix and the most common abdominal surgical emergency globally. The condition has a lifetime risk of 8%. Characteristic features include periumbilical abdominal pain that migrates to the right lower quadrant, fever, anorexia, nausea, and vomiting. Appendicitis |
|
|
| Gastrointestinal | Inflammatory diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea |
|
| Gynecologic | Pelvic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
|
| Fallopian tube Fallopian Tube A pair of highly specialized canals extending from the uterus to its corresponding ovary. They provide the means for ovum transport from the ovaries and they are the site of the ovum’s final maturation and fertilization. The fallopian tube consists of an interstitium, an isthmus, an ampulla, an infundibulum, and fimbriae. Its wall consists of three layers: serous, muscular, and an internal mucosal layer lined with both ciliated and secretory cells. Uterus, Cervix, and Fallopian Tubes: Anatomy and ovarian abscesses |
|
|
| Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and soft tissue Soft Tissue Soft Tissue Abscess | Diabetic foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy infection |
|
| Animal bite infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease |
|
|
| Brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification | Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis and brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease |
|
| Disseminated | Bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides |
|