Olfaction represents an ancient, evolutionarily critical physiologic system. Humans have the ability to detect and discriminate at least 10,000 different odorants. The sense of smell, or olfaction, begins in a small area on the roof of the nasal cavity Nasal cavity The proximal portion of the respiratory passages on either side of the nasal septum. Nasal cavities, extending from the nares to the nasopharynx, are lined with ciliated nasal mucosa. Nose Anatomy (External & Internal), which is covered in specialized mucosa. From there, the olfactory nerve Olfactory nerve The 1st cranial nerve. The olfactory nerve conveys the sense of smell. It is formed by the axons of olfactory receptor neurons which project from the olfactory epithelium (in the nasal epithelium) to the olfactory bulb. Nose Anatomy (External & Internal) transmits the sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology perception Perception The process by which the nature and meaning of sensory stimuli are recognized and interpreted. Psychiatric Assessment of smell via the olfactory pathway. This pathway is composed of the olfactory cells and bulb, the tractus and striae olfactoriae, and the primary olfactory cortex and amygdala Amygdala Almond-shaped group of basal nuclei anterior to the inferior horn of the lateral ventricle of the temporal lobe. The amygdala is part of the limbic system. Limbic System: Anatomy. Olfaction is responsible for the detection of hazards, pheromones, and food.
Last updated: Jan 3, 2025
The olfactory epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology is a pseudostratified columnar epithelium Pseudostratified columnar epithelium Cells vary in height, with all cells resting on the basement membrane but only some reaching all the way to the apical surface. Surface Epithelium: Histology overlying a lamina propria Lamina propria Whipple’s Disease and consists of the following cell types:
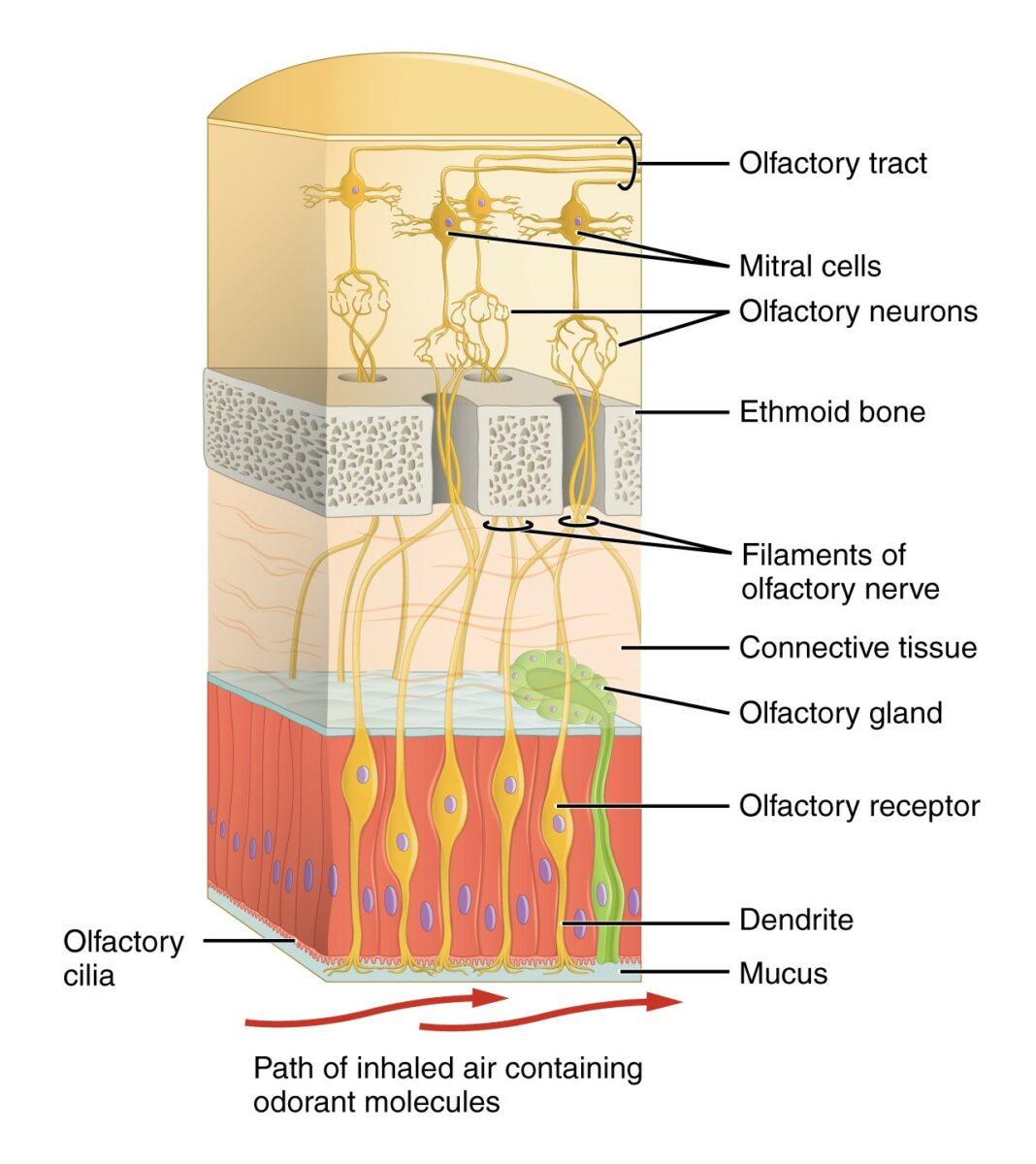
Diagram depicting the 1st structures of the olfactory system:
Odorants are perceived by specialized cilia within the nasal mucosa, which send an electrical signal via the olfactory nerve through the ethmoid bone to the olfactory bulb and tract.
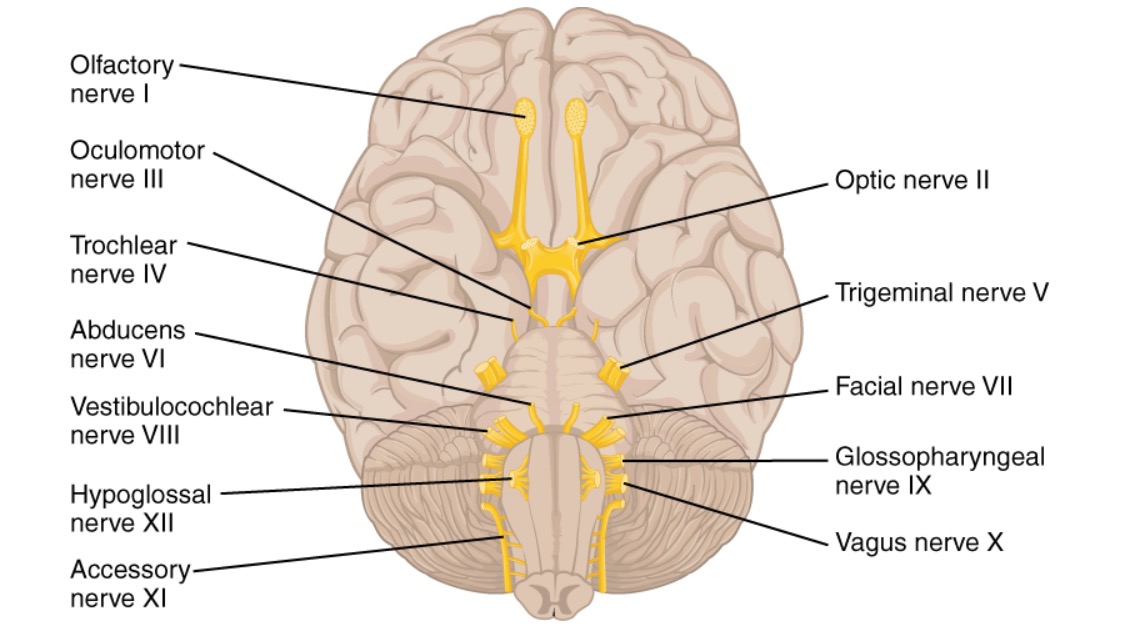
Inferior view of the brain, featuring the origin of the 12 cranial nerves (CNs):
Note the location and short length of the olfactory nerve (CN I).
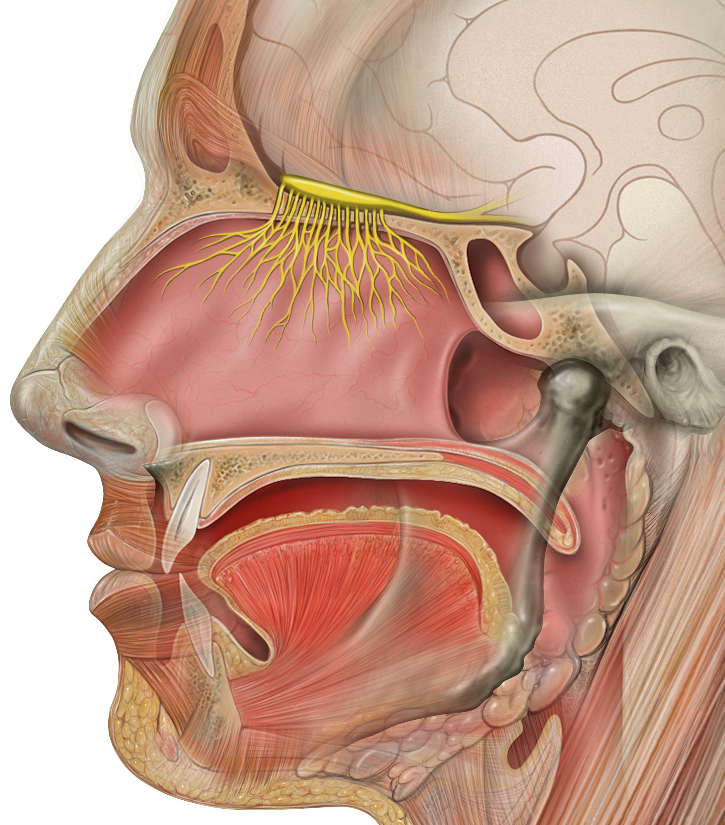
Sagittal section of the head, featuring the location of the olfactory cilia originating within the olfactory mucosa, combining to compose the fibers of the olfactory nerve and ascending through the cribriform plate of the ethmoid to the olfactory bulb (highlighted in yellow)
Image: “Head anatomy with olfactory nerve” by P. J. Lynch. License: CC BY 2.5Odors are first detected at the olfactory bulb, where the information is received and transmitted posteriorly along the olfactory tract to the olfactory cortex.
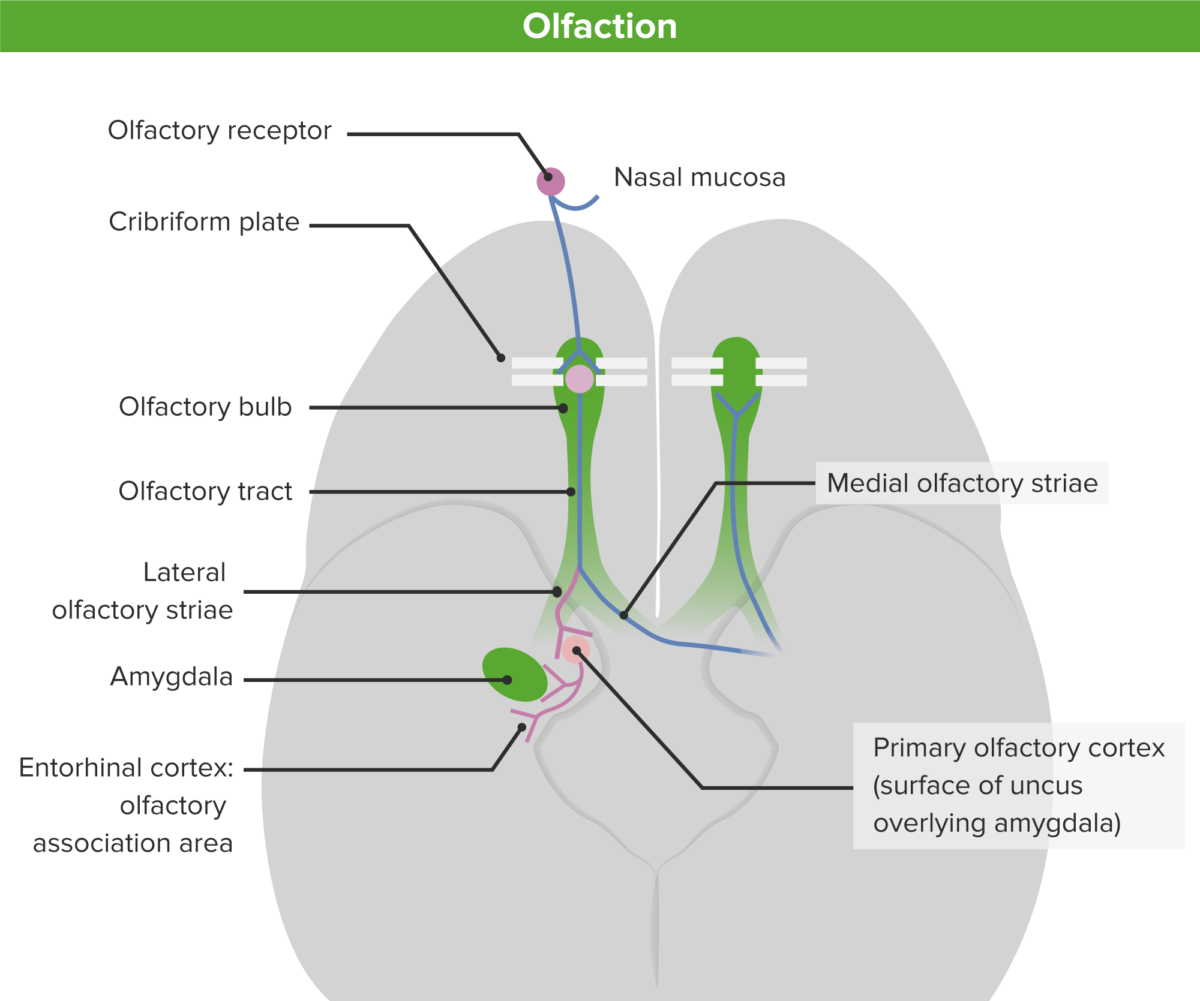
Schematic diagram of the olfactory pathway from the nasal mucosa to the primary and secondary olfactory cortex:
Note the ipsilateral and contralateral projections of the middle and lateral olfactory striae.
The olfactory cortex is unique in receiving direct sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology inputs from the mitral cells of the olfactory bulb. This process differs from the classic sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology pathway, where sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology information is 1st relayed in the thalamus Thalamus The thalamus is a large, ovoid structure in the dorsal part of the diencephalon that is located between the cerebral cortex and midbrain. It consists of several interconnected nuclei of grey matter separated by the laminae of white matter. The thalamus is the main conductor of information that passes between the cerebral cortex and the periphery, spinal cord, or brain stem. Thalamus: Anatomy before reaching the neocortex Neocortex The largest portion of the cerebral cortex in which the neurons are arranged in six layers in the mammalian brain: molecular, external granular, external pyramidal, internal granular, internal pyramidal and multiform layers. Cerebral Cortex: Anatomy.
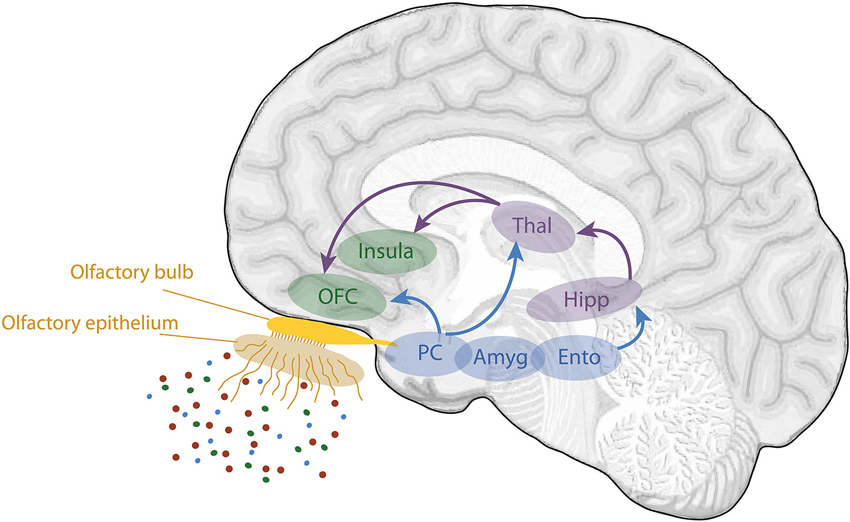
Schematic view of the human olfactory system:
The primary and secondary olfactory cortices are represented in blue and green, respectively.
Amyg: amygdala
Ento: entorhinal cortex
Hipp: hippocampus
OFC: orbitofrontal cortex
PC: piriform cortex
Thal: thalamus