The brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy are enveloped by 3 overlapping layers of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. The meninges function to protect the contents of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy. Infection of the CNS presents with inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the meninges, and the etiology can be elicited by examining CSF, which is contained within the subarachnoid space Subarachnoid space The space between the arachnoid membrane and pia mater, filled with cerebrospinal fluid. It contains large blood vessels that supply the brain and spinal cord. Subarachnoid Hemorrhage.
Last updated: Mar 31, 2025
The meninges are layers of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology that protect the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy.
The meninges consist of 3 layers of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology, with potential spaces between them:
| Layer | Origin | Characteristics |
|---|---|---|
| Epidural space Epidural space Space between the dura mater and the walls of the vertebral canal. Epidural Hemorrhage | NA |
|
| Dura mater | Mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation |
|
| Subdural space Subdural space Potential cavity which separates the arachnoid mater from the dura mater. Subdural Hemorrhage | NA |
|
| Arachnoid mater (leptomeninges) | Neural crest Neural crest The two longitudinal ridges along the primitive streak appearing near the end of gastrulation during development of nervous system (neurulation). The ridges are formed by folding of neural plate. Between the ridges is a neural groove which deepens as the fold become elevated. When the folds meet at midline, the groove becomes a closed tube, the neural tube. Hirschsprung Disease |
|
| Subarachnoid space Subarachnoid space The space between the arachnoid membrane and pia mater, filled with cerebrospinal fluid. It contains large blood vessels that supply the brain and spinal cord. Subarachnoid Hemorrhage | Choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy plexus |
|
| Pia mater (leptomeninges) | Neural crest Neural crest The two longitudinal ridges along the primitive streak appearing near the end of gastrulation during development of nervous system (neurulation). The ridges are formed by folding of neural plate. Between the ridges is a neural groove which deepens as the fold become elevated. When the folds meet at midline, the groove becomes a closed tube, the neural tube. Hirschsprung Disease |
|
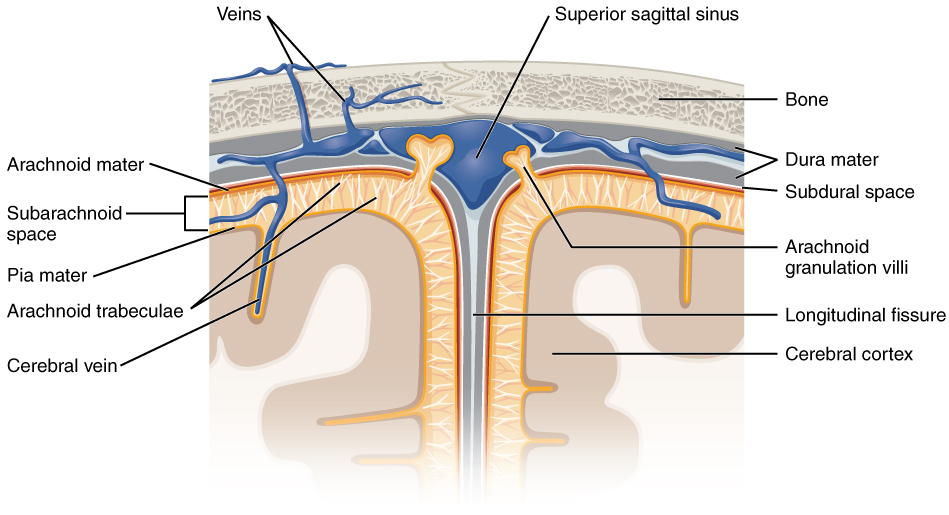
Layers of the meninges and their relationships beneath the skull
Image: “Diagram of section of top of brain showing the meninges and subarachnoid space” by OpenStax. License: CC BY 4.0The dura mater is the thickest layer of the meninges and provides structure to the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.
Dural foldings and dural sinuses come from the dura mater.
| Structure | Characteristics |
|---|---|
| Falx cerebri | Separates the right and left cerebral hemispheres |
| Falx cerebelli | Separates the right and left cerebellar hemispheres |
| Tentorium cerebelli | Tent, or roof, over the cerebellum Cerebellum The cerebellum, Latin for “little brain,” is located in the posterior cranial fossa, dorsal to the pons and midbrain, and its principal role is in the coordination of movements. The cerebellum consists of 3 lobes on either side of its 2 hemispheres and is connected in the middle by the vermis. Cerebellum: Anatomy |
| Diaphragma sellae | The roof over the pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland |
| Dural sinuses | The 2 layers of dura mater run together throughout most of the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy. Where they separate, the gap between them is called a dural venous sinus. These sinuses drain blood and CSF from the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and empty into the internal jugular vein Internal jugular vein Parapharyngeal Abscess. |
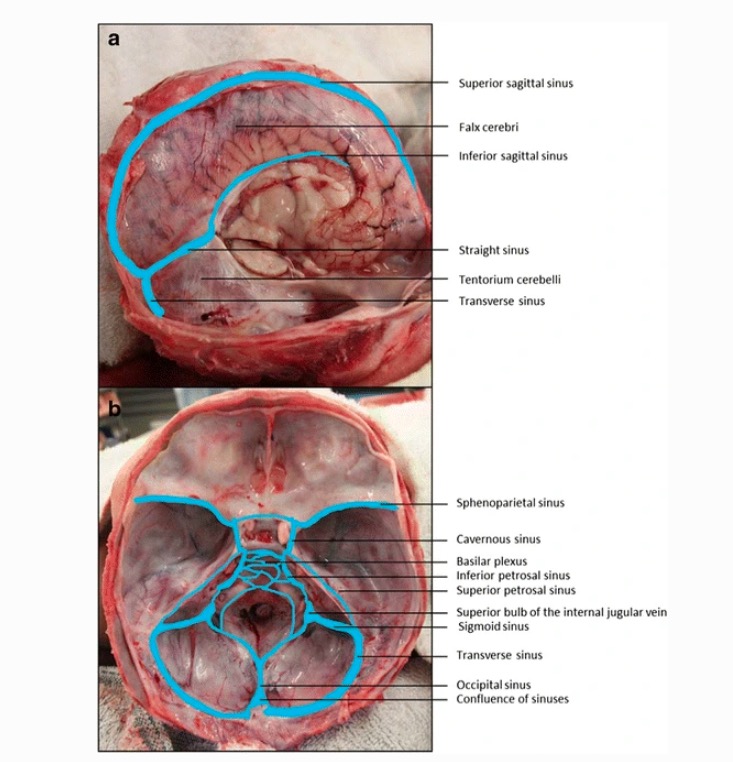
Dural venous sinuses
Image: “Dural venous sinuses” by Jmarchn. License: CC BY-SA 3.0, edited by Emma C. Cheshire et al. (2017).Neoplastic disorders:
Infectious disorders:
Traumatic disorders: