Epidural hemorrhage (EDH) is an event characterized by bleeding into the epidural space between the dural layers of the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy and the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy. The primary mechanism triggering bleeding is trauma (i.e., closed head injury Closed Head Injury Subdural Hemorrhage), which causes arterial injury Arterial Injury Hemothorax, most commonly middle meningeal artery injury. Epidural hemorrhage presents acutely, usually immediately (seconds to hours) following head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma, with an altered level of consciousness Altered Level of Consciousness Intracerebral Hemorrhage that may span from a momentary loss of consciousness to coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma. Diagnosis is based on clinical suspicion following head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma and is confirmed with neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant (i.e., noncontrast head CT). Management includes stabilization, stopping (possibly, the reversal) of all anticoagulants Anticoagulants Anticoagulants are drugs that retard or interrupt the coagulation cascade. The primary classes of available anticoagulants include heparins, vitamin K-dependent antagonists (e.g., warfarin), direct thrombin inhibitors, and factor Xa inhibitors. Anticoagulants, monitoring in a neurologic ICU ICU Hospital units providing continuous surveillance and care to acutely ill patients. West Nile Virus, and neurosurgical intervention.
Last updated: Jan 24, 2023
Epidural hemorrhage or epidural hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception (EDH) is an event characterized by bleeding into the epidural space between the dural layer of the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy and the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy. Epidural hemorrhage usually results from trauma.
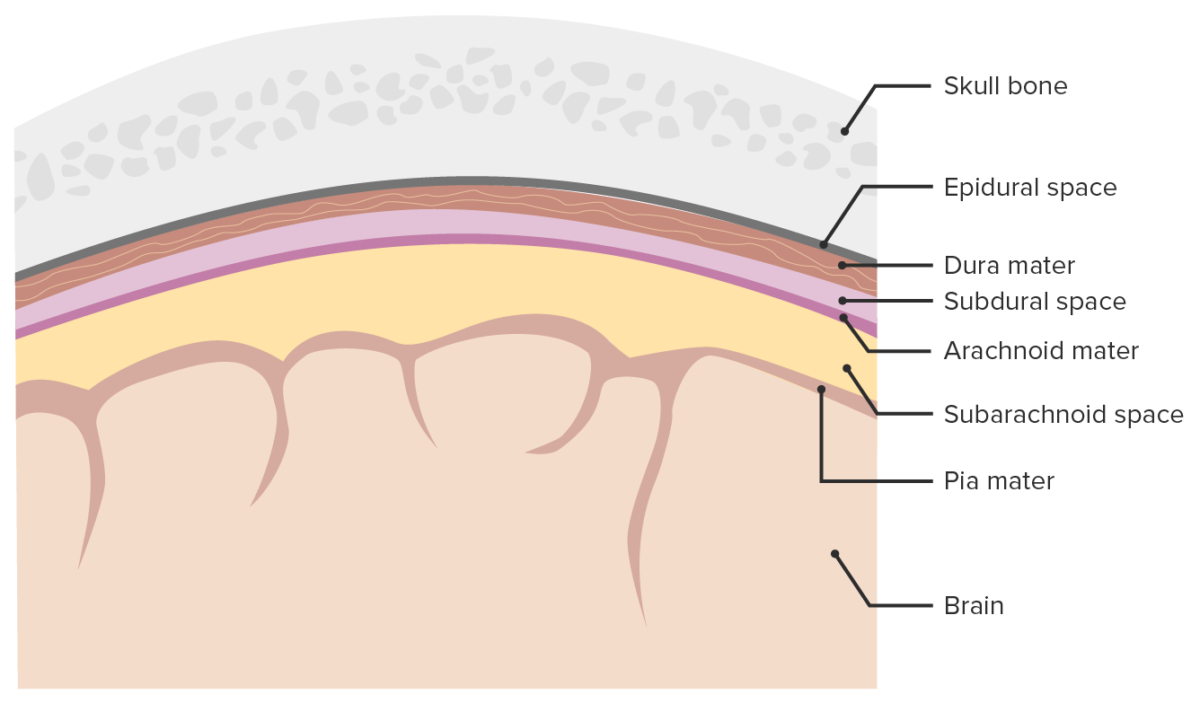
Meninges and meningeal spaces:
The image depicts the three layers (Dura mater, Arachnoid mater, Pia mater) surrounding the brain and spinal cord. The meninges serve as mechanical protection of the CNS. They also support the cerebral and spinal blood vessels and allow for passage of the cerebrospinal fluid (CSF). The subarachnoid space is filled with CSF.
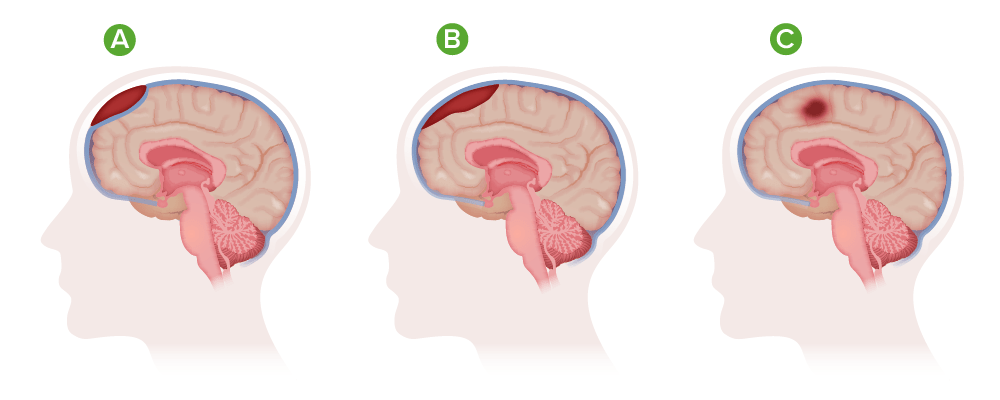
Types of hematoma:
A) Epidural hematoma;
B) Subdural hematoma;
C) Intracranial hematoma
Head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma/injury:
Nontraumatic EDH:
Head trauma Head trauma Head trauma occurs when external forces are directed to the skull and brain structures, resulting in damage to the skull, brain, and intracranial structures. Head injuries can be classified as open (penetrating) or closed (blunt), and primary (from the initial trauma) or secondary (indirect brain injury), and range from mild to severe and life-threatening. Head Trauma is the most common etiology of EDH. A “lucid interval” followed by rapid neurologic deterioration is common.
Noncontrast head CT:
Head MRI:
Angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery:
Lumbar puncture Lumbar Puncture Febrile Infant:
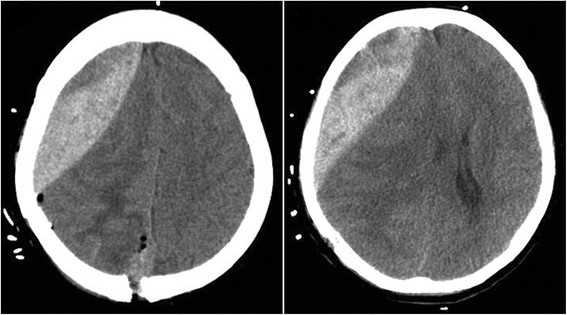
Epidural hematoma:
CT showing an epidural hematoma in front of the surgical field after tumor resection
Acute EDH, especially if presenting with neurologic compromise or coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma, is an emergent neurologic situation often requiring surgical intervention. Failure of prompt stabilization, diagnosis, evaluation, and intervention could result in hemorrhagic expansion, parenchymal brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification injury, elevated ICP ICP Normal intracranial pressure (ICP) is defined as < 15 mm Hg, whereas pathologically increased ICP is any pressure ≥ 20 mm Hg. Increased ICP may result from several etiologies, including trauma, intracranial hemorrhage, mass lesions, cerebral edema, increased CSF production, and decreased CSF absorption. Increased Intracranial Pressure (ICP), brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification herniation Herniation Omphalocele, and death.
Decision-making tools used clinically to determine operative or nonoperative management include: