A seizure is abnormal electrical activity of the neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology in the cerebral cortex Cerebral cortex The cerebral cortex is the largest and most developed part of the human brain and CNS. Occupying the upper part of the cranial cavity, the cerebral cortex has 4 lobes and is divided into 2 hemispheres that are joined centrally by the corpus callosum. Cerebral Cortex: Anatomy that can manifest in numerous ways depending on the region of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology, creating a net excitation. The 2 major classes of seizures are focal and generalized. Diagnosis is clinical, relying on history and physical exam, but also may use EEG and other tools. Management includes both abortive and preventive medications but may not be required in self-limited cases with no etiology found during workup.
Last updated: Dec 5, 2022
Seizures are episodes of neurologic dysfunction caused by abnormal excitatory activities of neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology characterized by a sudden change in senses, perception Perception The process by which the nature and meaning of sensory stimuli are recognized and interpreted. Psychiatric Assessment, motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology activity, or behavior.
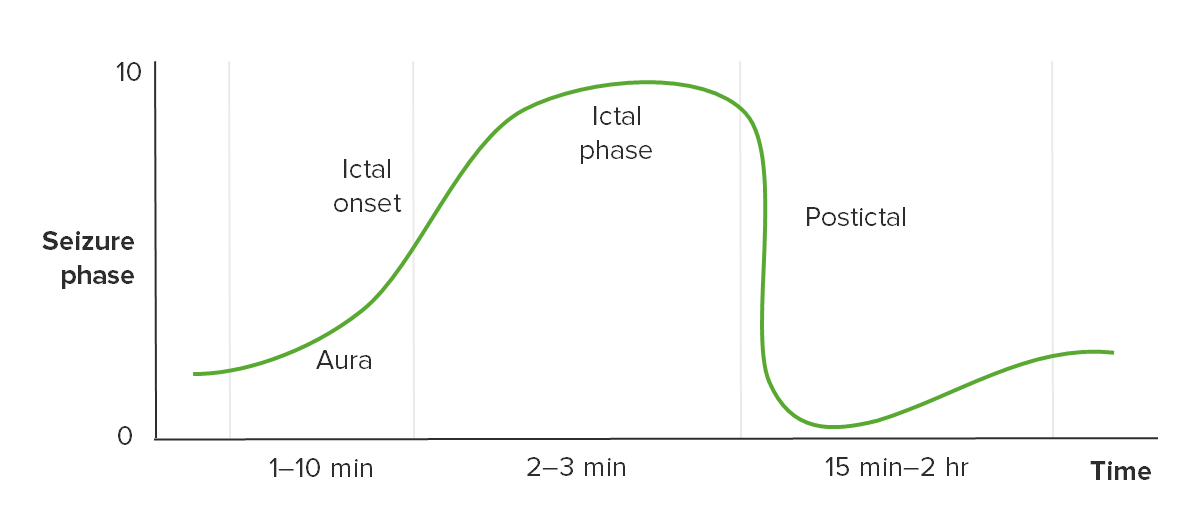
Timeline of seizure phases
Image by Lecturio.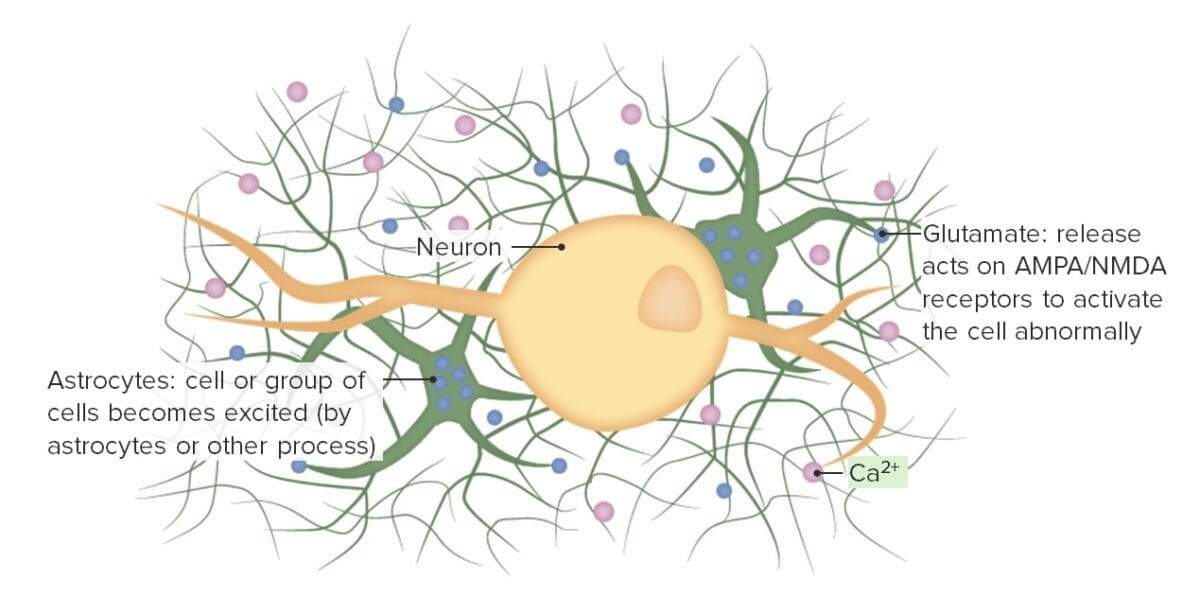
Step 1: short in the circuit describing the 1st step of the pathophysiology of seizures
AMPA: α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
NMDA: N-methyl-D-aspartate
Step 2 of the pathophysiology of seizures, driving of normal neighbors:
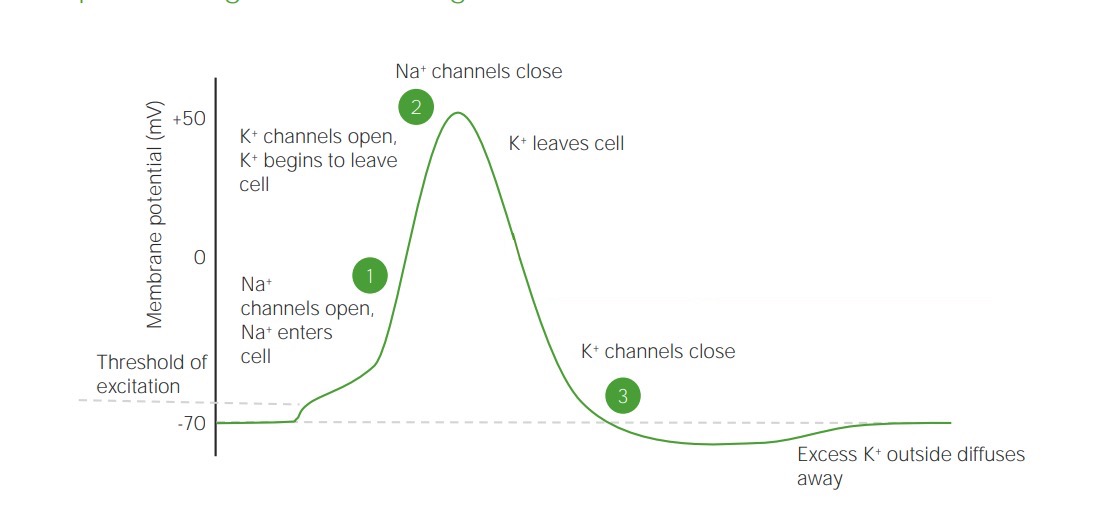
The diagram shows a membrane potential and steps that allow excess K+ to polarize surrounding cells.
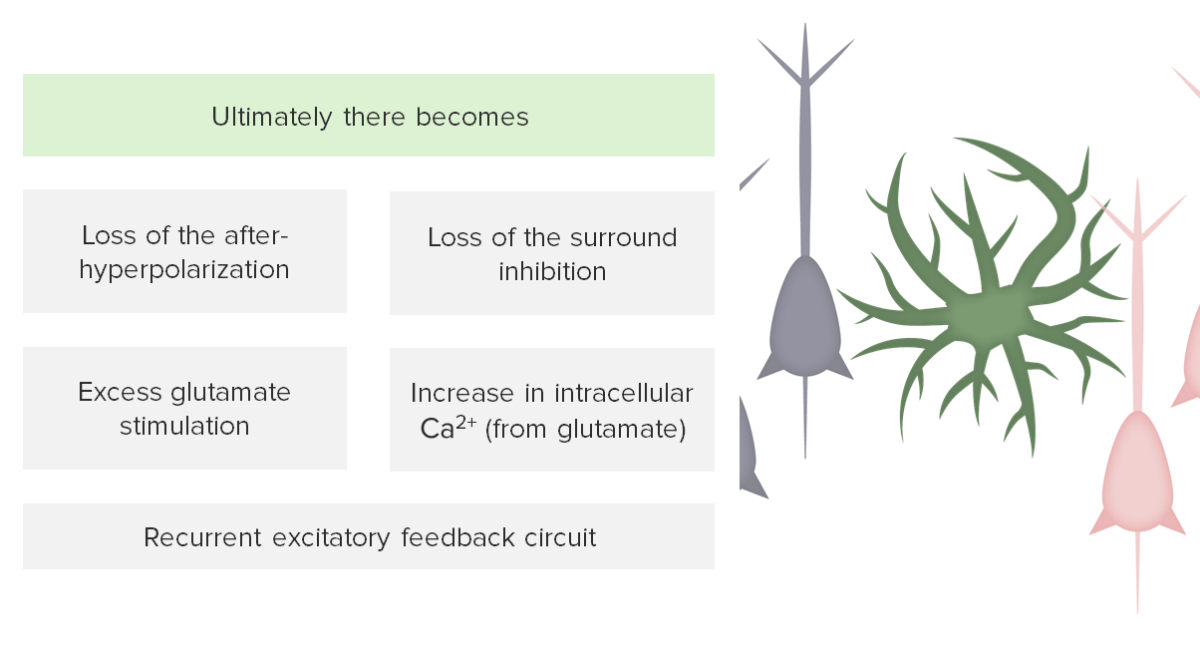
Step 3: failure of inhibition in pathophysiology of seizures
Image by Lecturio.| Simple | Complex | Secondary generalized |
|---|---|---|
|
|
|
| Absence | First-degree generalized brief staring spells, often confused with daydreaming, with 3-Hz spike-and-wave EEG |
|---|---|
| Myoclonic | Typically focal myoclonic jerks Myoclonic Jerks Neonatal Abstinence Syndrome with brief loss of consciousness but no convulsions and little postictal confusion |
| Tonic | Focal, isolated rigidity Rigidity Continuous involuntary sustained muscle contraction which is often a manifestation of basal ganglia diseases. When an affected muscle is passively stretched, the degree of resistance remains constant regardless of the rate at which the muscle is stretched. This feature helps to distinguish rigidity from muscle spasticity. Megacolon |
| Generalized tonic-clonic | Most often convulsive (but may be nonconvulsive) with first-degree generalization without aura Aura Reversible neurological phenomena that often precede or coincide with headache onset. Migraine Headache |
| Atonic | Drop attacks Drop Attacks Seizures in Children are most common in children. |
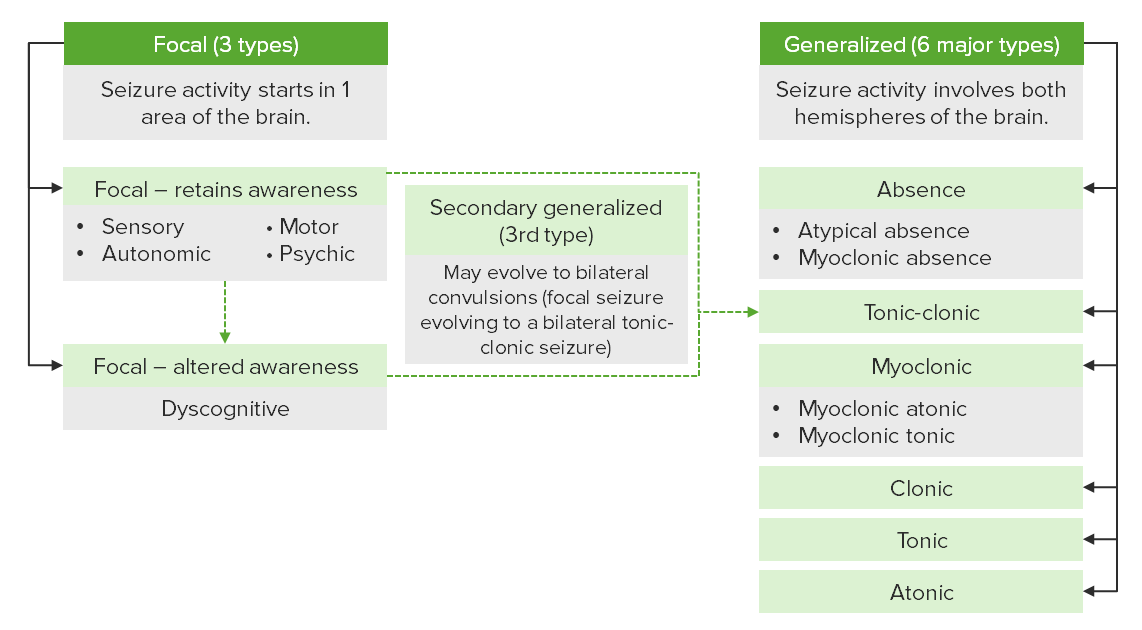
Types of seizures and classifications
Image by Lecturio.Initial evaluation and stabilization centers around screening Screening Preoperative Care for hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia, hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage, and hemodynamic instability.
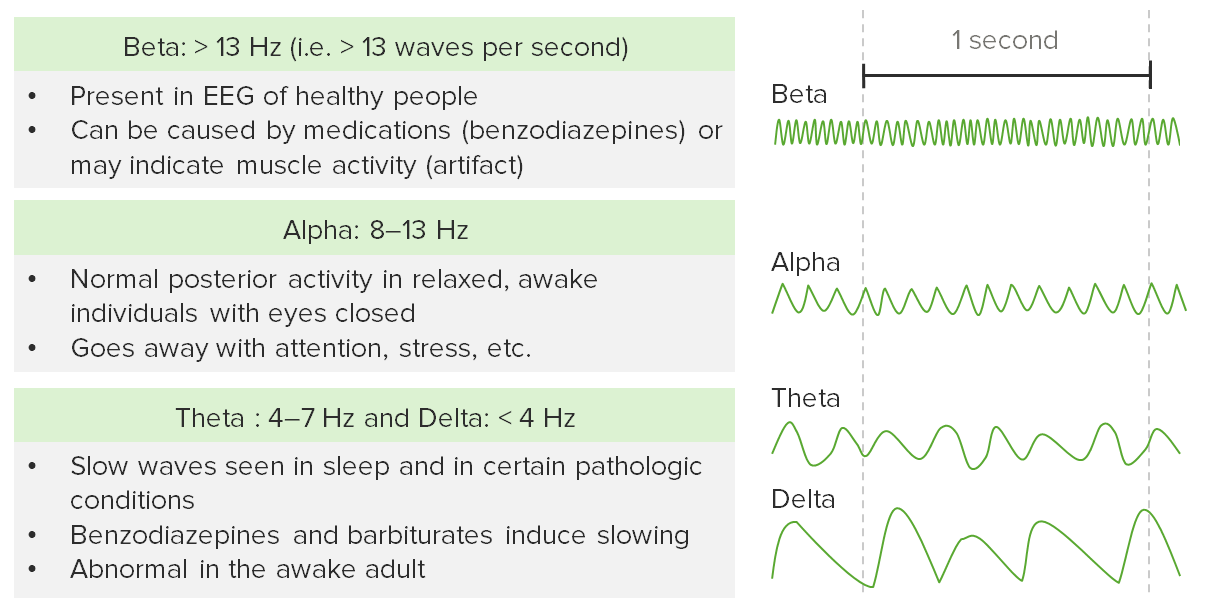
Types of normal electrical activity on an electroencephalogram
Image by Lecturio.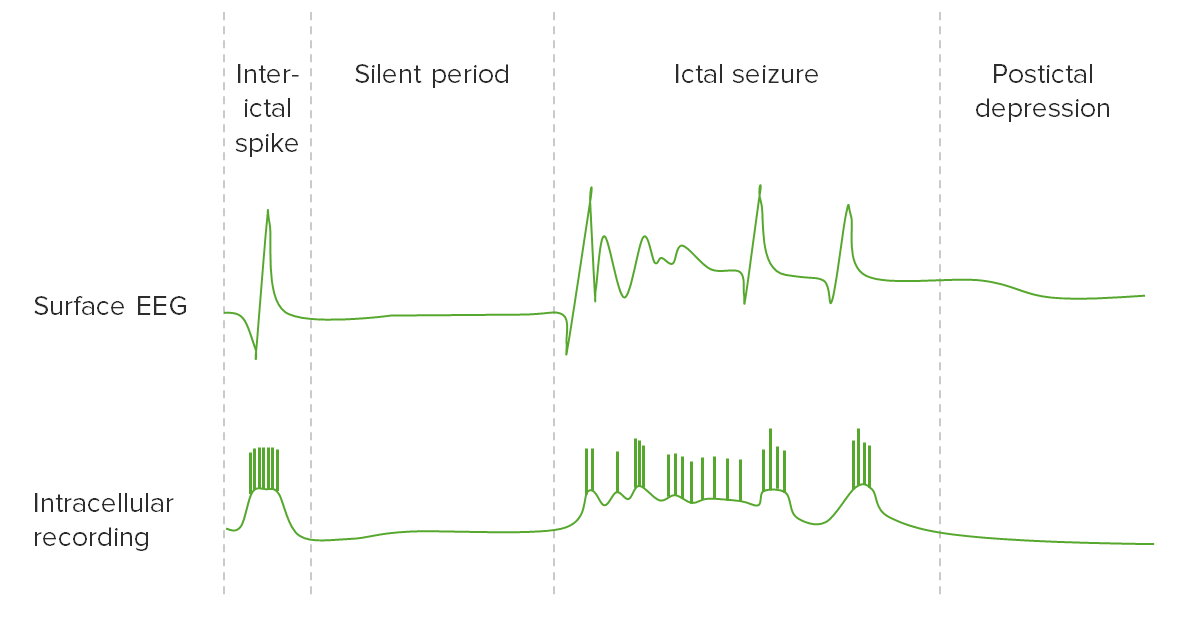
Electrical activity of the brain on an EEG during a seizure
Image by Lecturio.| Spell | Seizure | Syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope | PNES | |
|---|---|---|---|---|
| Laboratories |
|
|
|
|
| Imaging |
|
|
|
None needed |
| Other testing |
|
|
|
|
| Seizure | Syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope | Transient ischemic attack Transient ischemic attack Transient ischemic attack (TIA) is a temporary episode of neurologic dysfunction caused by ischemia without infarction that resolves completely when blood supply is restored. Transient ischemic attack is a neurologic emergency that warrants urgent medical attention. Transient Ischemic Attack (TIA) | |
|---|---|---|---|
| Aura Aura Reversible neurological phenomena that often precede or coincide with headache onset. Migraine Headache | Yes or none | None, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome) | None |
| Posture | None | Erect | None |
| Onset | Acute | Acute/ variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Acute |
| Duration | 1–2 minutes | Seconds to minutes | Minutes to hours |
| Movements | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables/tonic-clonic | Lost-tone myoclonus Myoclonus Involuntary shock-like contractions, irregular in rhythm and amplitude, followed by relaxation, of a muscle or a group of muscles. This condition may be a feature of some central nervous system diseases; (e.g., epilepsy-myoclonic). Nocturnal myoclonus is the principal feature of the nocturnal myoclonus syndrome. Neurological Examination | Deficits |
| Incontinence | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Very rare | None |
| EEG | Epileptiform | General slow | Focal slowing or generalized slowing with posterior circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment event |
| Trauma | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables | Usually none |
| Offset | Slow/confused | Rapid/alert | Alert |
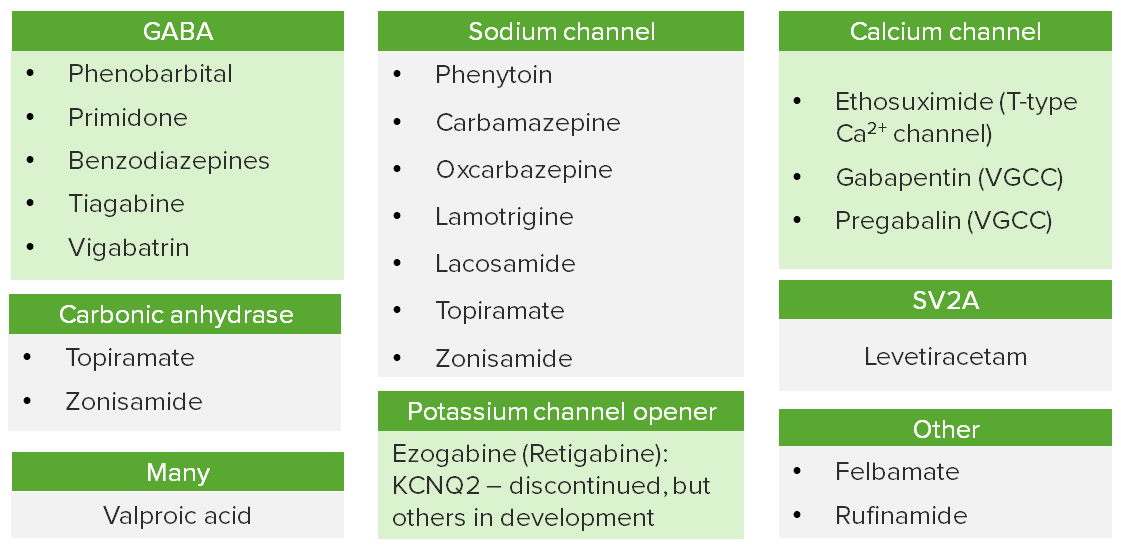
Mechanisms of action of anticonvulsants
VGCC: voltage-gated calcium channels