Epilepsy is a chronic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification disorder marked by recurrent and unprovoked seizures Unprovoked Seizures Seizures. These seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures can be classified as focal or generalized and idiopathic Idiopathic Dermatomyositis or secondary to another condition. Clinical presentation correlates to the classification of the epileptic disorder. Diagnosis is confirmed with EEG EEG Seizures. While some epileptic disorders resolve over time, many require lifelong antiepileptic medication for management or, in some refractory cases, surgical procedures.
Last updated: Jan 13, 2023
Epilepsy is a chronic brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification disorder marked by recurrent and unprovoked seizures Unprovoked Seizures Seizures.
Several features may be used to classify epilepsy, which is useful in considering management options.
Epilepsy syndromes relate to seizure types and are classified primarily using the clinical history; classification requires input from a family member or witness to the seizure in addition to history from the affected individual.
Diagnosis is based on history, lab results, and EEG EEG Seizures findings.
EEG EEG Seizures is a test to monitor the electrical sensitivity of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.

Types of normal electrical activity on an electroencephalogram
Image by Lecturio.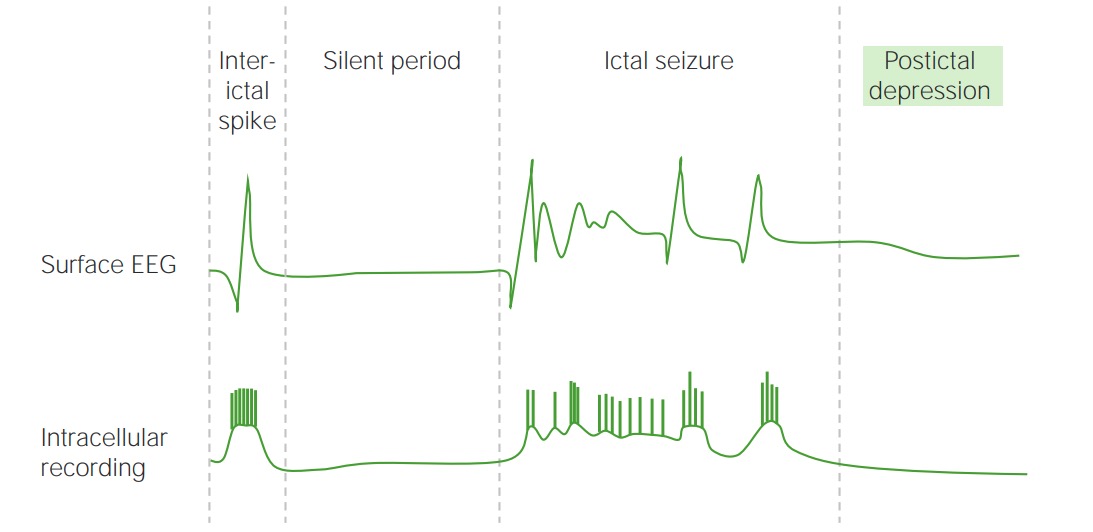
Electrical activity of the brain on an EEG during a seizure
Image by Lecturio.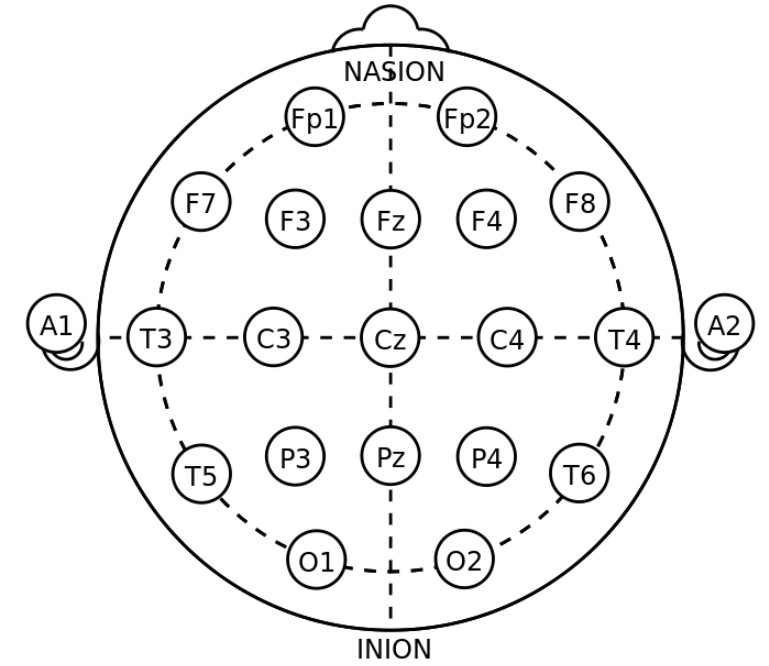
Electrode placements for standard EEG
Image: “21 electrodes of International 10-20 system for EEG” by トマトン124. License: Public DomainThe choice of antiseizure medications is based on the type of epilepsy syndrome. Starting treatment after a single unprovoked seizure remains controversial.
| Name | Mechanism of action | Indication | Side effects |
|---|---|---|---|
| Phenobarbital Phenobarbital A barbituric acid derivative that acts as a nonselective central nervous system depressant. It potentiates gamma-aminobutyric acid action on gaba-a receptors, and modulates chloride currents through receptor channels. It also inhibits glutamate induced depolarizations. First-Generation Anticonvulsant Drugs | Enhances GABA-mediated inhibition of synaptic transmission Synaptic transmission The communication from a neuron to a target (neuron, muscle, or secretory cell) across a synapse. In chemical synaptic transmission, the presynaptic neuron releases a neurotransmitter that diffuses across the synaptic cleft and binds to specific synaptic receptors, activating them. The activated receptors modulate specific ion channels and/or second-messenger systems in the postsynaptic cell. In electrical synaptic transmission, electrical signals are communicated as an ionic current flow across electrical synapses. Synapses and Neurotransmission | All types of epilepsy except absence |
|
| Phenytoin Phenytoin An anticonvulsant that is used to treat a wide variety of seizures. The mechanism of therapeutic action is not clear, although several cellular actions have been described including effects on ion channels, active transport, and general membrane stabilization. Phenytoin has been proposed for several other therapeutic uses, but its use has been limited by its many adverse effects and interactions with other drugs. First-Generation Anticonvulsant Drugs | Inhibits Na channel activation to inhibit neurotransmission Neurotransmission The communication from a neuron to a target (neuron, muscle, or secretory cell) across a synapse. In chemical synaptic transmission, the presynaptic neuron releases a neurotransmitter that diffuses across the synaptic cleft and binds to specific synaptic receptors, activating them. The activated receptors modulate specific ion channels and/or second-messenger systems in the postsynaptic cell. In electrical synaptic transmission, electrical signals are communicated as an ionic current flow across electrical synapses. Synapses and Neurotransmission | Focal seizures Focal Seizures Seizures in Children and generalized tonic-clonic seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures |
|
| Fosphenytoin Fosphenytoin First-Generation Anticonvulsant Drugs | Same as phenytoin Phenytoin An anticonvulsant that is used to treat a wide variety of seizures. The mechanism of therapeutic action is not clear, although several cellular actions have been described including effects on ion channels, active transport, and general membrane stabilization. Phenytoin has been proposed for several other therapeutic uses, but its use has been limited by its many adverse effects and interactions with other drugs. First-Generation Anticonvulsant Drugs | Same as phenytoin Phenytoin An anticonvulsant that is used to treat a wide variety of seizures. The mechanism of therapeutic action is not clear, although several cellular actions have been described including effects on ion channels, active transport, and general membrane stabilization. Phenytoin has been proposed for several other therapeutic uses, but its use has been limited by its many adverse effects and interactions with other drugs. First-Generation Anticonvulsant Drugs | Less risk of hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension and cardiac dysfunction then with phenytoin Phenytoin An anticonvulsant that is used to treat a wide variety of seizures. The mechanism of therapeutic action is not clear, although several cellular actions have been described including effects on ion channels, active transport, and general membrane stabilization. Phenytoin has been proposed for several other therapeutic uses, but its use has been limited by its many adverse effects and interactions with other drugs. First-Generation Anticonvulsant Drugs |
| Carbamazepine Carbamazepine A dibenzazepine that acts as a sodium channel blocker. It is used as an anticonvulsant for the treatment of grand mal and psychomotor or focal seizures. It may also be used in the management of bipolar disorder, and has analgesic properties. First-Generation Anticonvulsant Drugs | Works on voltage-gated Na channels Channels The Cell: Cell Membrane to inhibit synaptic transmission Synaptic transmission The communication from a neuron to a target (neuron, muscle, or secretory cell) across a synapse. In chemical synaptic transmission, the presynaptic neuron releases a neurotransmitter that diffuses across the synaptic cleft and binds to specific synaptic receptors, activating them. The activated receptors modulate specific ion channels and/or second-messenger systems in the postsynaptic cell. In electrical synaptic transmission, electrical signals are communicated as an ionic current flow across electrical synapses. Synapses and Neurotransmission | Focal and secondary generalized seizures Generalized Seizures Seizures |
|
| Lamotrigine Lamotrigine A phenyltriazine compound, sodium and calcium channel blocker that is used for the treatment of seizures and bipolar disorder. Second-Generation Anticonvulsant Drugs | Blocks excitatory Na ion channels Channels The Cell: Cell Membrane | Focal and generalized epilepsy; safest antiepileptic drug during pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care |
|
| Ethosuximide Ethosuximide An anticonvulsant especially useful in the treatment of absence seizures unaccompanied by other types of seizures. First-Generation Anticonvulsant Drugs | Works on T-type Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts) channel to decrease burst firing of thalamocortical neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology | Absence seizures Absence seizures Brief period of unresponsiveness thats lasts about 4–30 seconds and can occur multiple times per day Seizures in Children |
|
| Gabapentin Gabapentin A cyclohexane-gamma-aminobutyric acid derivative that is used for the treatment of partial seizures; neuralgia; and restless legs syndrome. Second-Generation Anticonvulsant Drugs | Acts on voltage-gated Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts) channels Channels The Cell: Cell Membrane, which increase inhibitory tone | Focal seizures Focal Seizures Seizures in Children |
|
| Levetiracetam Levetiracetam A pyrrolidinone and acetamide derivative that is used primarily for the treatment of seizures and some movement disorders, and as a nootropic agent. Second-Generation Anticonvulsant Drugs | Modifies synaptic protein SV2A | Focal and generalized epilepsy; often used as 1st-line therapy; well tolerated |
|
| Topiramate Topiramate A sulfamate-substituted fructose analog that was originally identified as a hypoglycemic agent. It is used for the treatment of epilepsy and migraine disorders, and may also promote weight loss. Second-Generation Anticonvulsant Drugs | Blocks voltage-gated Na channels Channels The Cell: Cell Membrane; also inhibits carbonic anhydrase Carbonic anhydrase A family of zinc-containing enzymes that catalyze the reversible hydration of carbon dioxide. They play an important role in the transport of carbon dioxide from the tissues to the lung. Carbonic Anhydrase Inhibitors, causing acidosis Acidosis A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. Respiratory Acidosis in the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification → partial protection against seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures | Primary generalized onset tonic-clonic seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures |
|
| Valproic acid Valproic acid A fatty acid with anticonvulsant and anti-manic properties that is used in the treatment of epilepsy and bipolar disorder. The mechanisms of its therapeutic actions are not well understood. It may act by increasing gamma-aminobutyric acid levels in the brain or by altering the properties of voltage-gated sodium channels. First-Generation Anticonvulsant Drugs | Multiple | Focal seizures Focal Seizures Seizures in Children with impaired awareness, generalized and absence seizures Absence seizures Brief period of unresponsiveness thats lasts about 4–30 seconds and can occur multiple times per day Seizures in Children |
|