A neurological exam is a systematic assessment of cognitive, sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology, and motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology responses to identify pathologies of the nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification. A neurological exam allows for the localization of neurologic lesions to narrow the differential diagnosis and focus on subsequent laboratory and imaging examinations. The exam should include assessments of the subject's mental status, speech, cranial nerves Cranial nerves There are 12 pairs of cranial nerves (CNs), which run from the brain to various parts of the head, neck, and trunk. The CNs can be sensory or motor or both. The CNs are named and numbered in Roman numerals according to their location, from the front to the back of the brain. The 12 Cranial Nerves: Overview and Functions, motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology system, deep tendon reflexes, sensation, balance, and coordination Coordination Cerebellar Disorders.
Last updated: Apr 17, 2024
Mental status examination Mental Status Examination Psychiatric Assessment is an assessment of a subject’s current mental capacity based on the following factors:
A basic understanding of the underlying neuroanatomy of the head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess is required before discussing the components of examining the cranial nerves Cranial nerves There are 12 pairs of cranial nerves (CNs), which run from the brain to various parts of the head, neck, and trunk. The CNs can be sensory or motor or both. The CNs are named and numbered in Roman numerals according to their location, from the front to the back of the brain. The 12 Cranial Nerves: Overview and Functions.
| Cranial nerve (CN) | Examination |
|---|---|
| CN I: olfactory nerve Olfactory nerve The 1st cranial nerve. The olfactory nerve conveys the sense of smell. It is formed by the axons of olfactory receptor neurons which project from the olfactory epithelium (in the nasal epithelium) to the olfactory bulb. Nose Anatomy (External & Internal) | Test olfaction Olfaction The sense of smell, or olfaction, begins in a small area on the roof of the nasal cavity, which is covered in specialized mucosa. From there, the olfactory nerve transmits the sensory perception of smell via the olfactory pathway. This pathway is composed of the olfactory cells and bulb, the tractus and striae olfactoriae, and the primary olfactory cortex and amygdala. Olfaction: Anatomy of the subject using non-irritant substances. |
| CN II: optic nerve Optic nerve The 2nd cranial nerve which conveys visual information from the retina to the brain. The nerve carries the axons of the retinal ganglion cells which sort at the optic chiasm and continue via the optic tracts to the brain. The largest projection is to the lateral geniculate nuclei; other targets include the superior colliculi and the suprachiasmatic nuclei. Though known as the second cranial nerve, it is considered part of the central nervous system. The 12 Cranial Nerves: Overview and Functions |
|
| CN III: oculomotor nerve Oculomotor nerve The 3D cranial nerve. The oculomotor nerve sends motor fibers to the levator muscles of the eyelid and to the superior rectus, inferior rectus, and inferior oblique muscles of the eye. It also sends parasympathetic efferents (via the ciliary ganglion) to the muscles controlling pupillary constriction and accommodation. The motor fibers originate in the oculomotor nuclei of the midbrain. The 12 Cranial Nerves: Overview and Functions; CN IV: trochlear nerve Trochlear nerve The 4th cranial nerve. The trochlear nerve carries the motor innervation of the superior oblique muscles of the eye. The 12 Cranial Nerves: Overview and Functions; CN VI: abducens nerve Abducens nerve The 6th cranial nerve which originates in the abducens nucleus of the pons and sends motor fibers to the lateral rectus muscles of the eye. Damage to the nerve or its nucleus disrupts horizontal eye movement control. The 12 Cranial Nerves: Overview and Functions |
|
| CN V: trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions |
|
| CN VII: facial nerve Facial nerve The 7th cranial nerve. The facial nerve has two parts, the larger motor root which may be called the facial nerve proper, and the smaller intermediate or sensory root. Together they provide efferent innervation to the muscles of facial expression and to the lacrimal and salivary glands, and convey afferent information for taste from the anterior two-thirds of the tongue and for touch from the external ear. The 12 Cranial Nerves: Overview and Functions |
|
| CN VIII: vestibulocochlear nerve Vestibulocochlear nerve The 8th cranial nerve. The vestibulocochlear nerve has a cochlear part (cochlear nerve) which is concerned with hearing and a vestibular part (vestibular nerve) which mediates the sense of balance and head position. The fibers of the cochlear nerve originate from neurons of the spiral ganglion and project to the cochlear nuclei (cochlear nucleus). The fibers of the vestibular nerve arise from neurons of scarpa’s ganglion and project to the vestibular nuclei. The 12 Cranial Nerves: Overview and Functions |
|
| CN IX: glossopharyngeal nerve Glossopharyngeal nerve The 9th cranial nerve. The glossopharyngeal nerve is a mixed motor and sensory nerve; it conveys somatic and autonomic efferents as well as general, special, and visceral afferents. Among the connections are motor fibers to the stylopharyngeus muscle, parasympathetic fibers to the parotid glands, general and taste afferents from the posterior third of the tongue, the nasopharynx, and the palate, and afferents from baroreceptors and chemoreceptor cells of the carotid sinus. Pharynx: Anatomy; CN X: vagus nerve Vagus nerve The 10th cranial nerve. The vagus is a mixed nerve which contains somatic afferents (from skin in back of the ear and the external auditory meatus), visceral afferents (from the pharynx, larynx, thorax, and abdomen), parasympathetic efferents (to the thorax and abdomen), and efferents to striated muscle (of the larynx and pharynx). Pharynx: Anatomy |
|
| CN XI: accessory nerve |
|
| CN XII: hypoglossal nerve Hypoglossal nerve The 12th cranial nerve. The hypoglossal nerve originates in the hypoglossal nucleus of the medulla and supplies motor innervation to all of the muscles of the tongue except the palatoglossus (which is supplied by the vagus). This nerve also contains proprioceptive afferents from the tongue muscles. Lips and Tongue: Anatomy |
|

Testing olfaction, cranial nerve I:
Here, an alcohol pad is used.
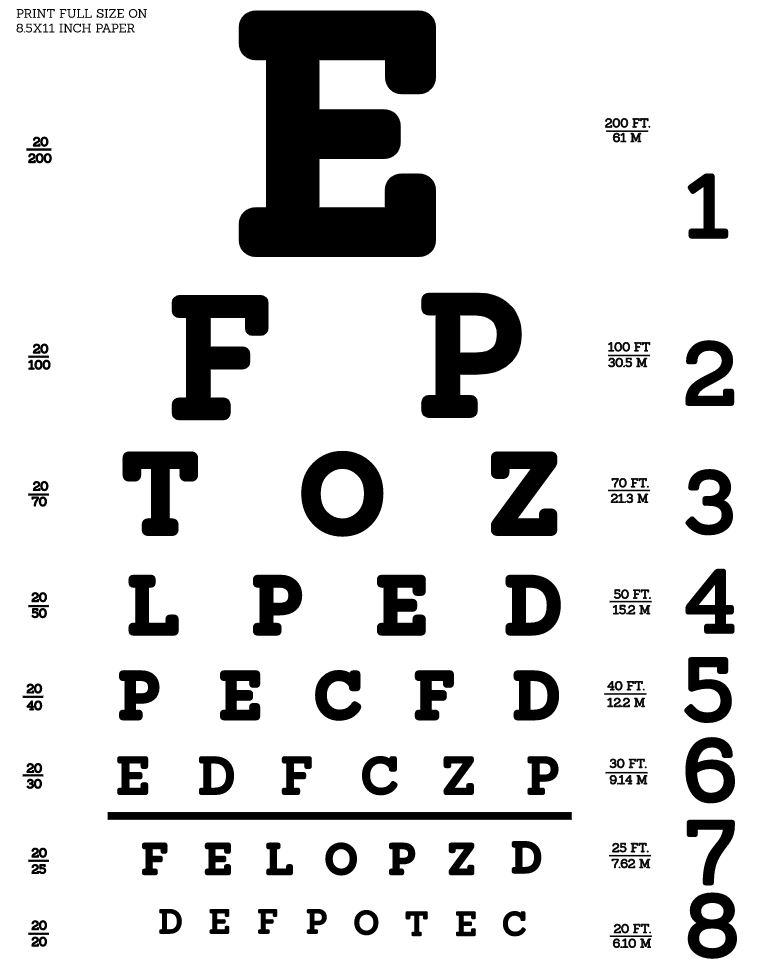
Snellen eye chart to test visual acuity
Image: “Snellen chart by Openclipart” by Openclipart. License: CC0 1.0
Testing visual fields, cranial nerve II:
The subject is asked to cover 1 eye and focus on the examiner’s nose. The examiner then moves their fingers in the upper or lower visual fields.

Testing extraocular movements, cranial nerves III, IV, and VI:
The subject is asked to keep their head still and follow the examiner’s finger with just their eyes.
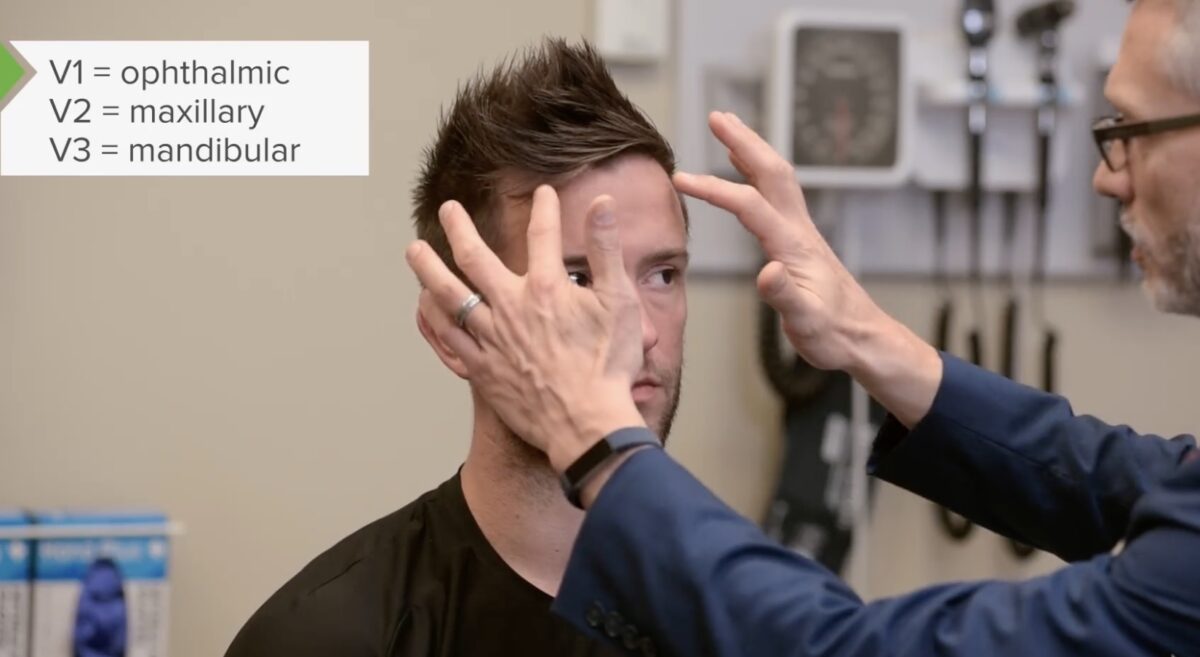
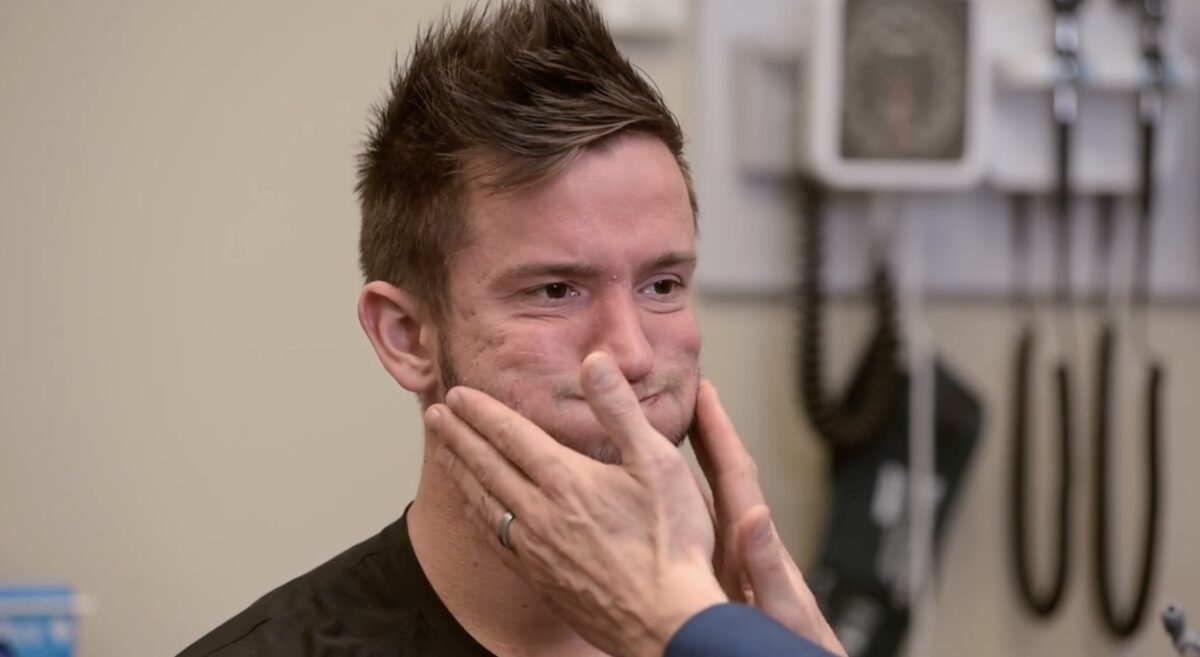
Testing facial sensation, cranial nerve V:
It is important to test sensation to light touch for each branch of the cranial nerve V, including the forehead (V1), maxillary region (V2), and mandibular region (V3).
Testing the facial musculature, cranial nerve VII:
The subject is asked to puff out their cheeks to demonstrate strength in the facial muscles. Other tasks can include raising their eyebrows, closing their eyes tightly, and smiling.

Testing cochlear function, cranial nerve VIII:
For the Weber test, a vibrating tuning fork is placed on the subject’s forehead (midline). A positive test for conductive hearing loss would result in the subject noting a louder sound on the affected side. For sensorineural hearing loss, the sound would be louder on the unaffected side.

Weber and Rinne tests
Image by Lecturio.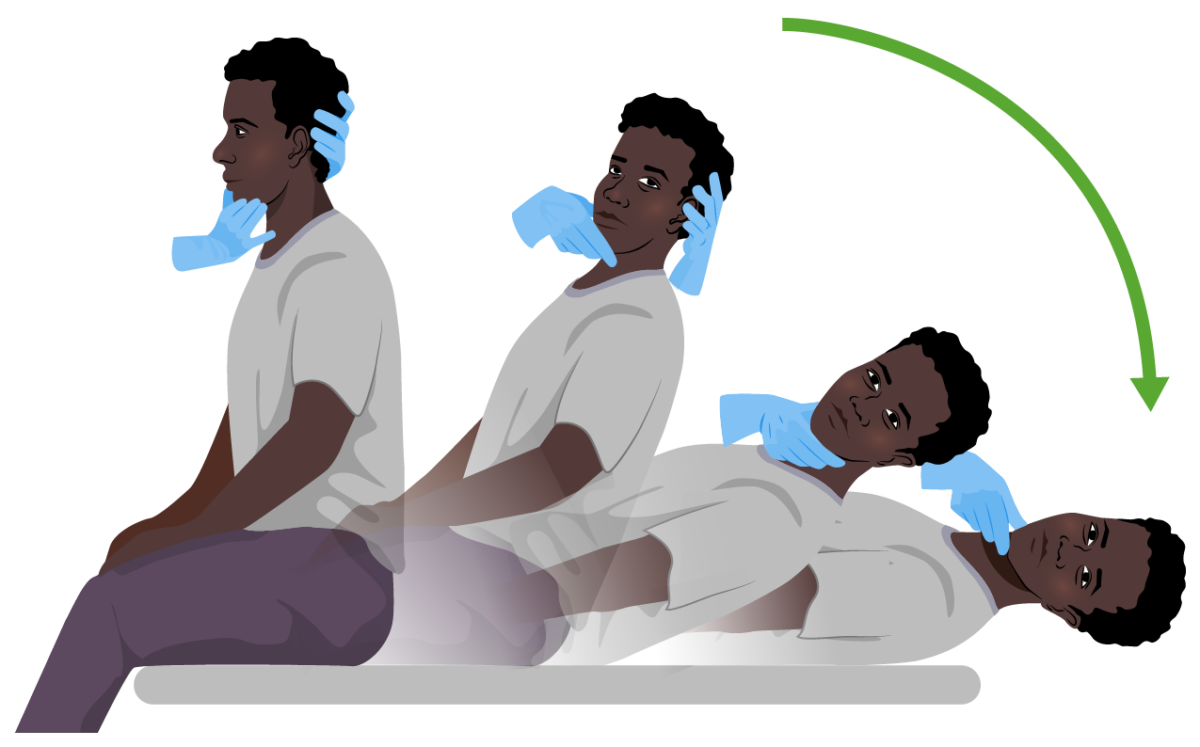
Dix-Hallpike maneuver:
Both diagnostic and curative in benign paroxysmal positional vertigo (BPPV). The subject sits on an examination table and quickly adopts a supine position while the examiner supports their head (to the right or to the left) at a 20º angle below the edge of the bed. The position is held for 30 seconds. In individuals with BPPV, symptoms of vertigo with or without nystagmus become evident.

Testing elevation of the soft palate and uvula, cranial nerves IX and X:
It is important to evaluate for symmetry of the soft palate. The uvula should be midline.

Testing sternocleidomastoid function, cranial nerve XI:
For this test, have the subject turn their head against resistance.

Testing tongue movements, cranial nerve (CN) XII:
For this test, have the subject stick out their tongue and move it from side to side. In CN XII palsy, the tongue will deviate toward the affected side.
Motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology system examination includes the following:

Strength testing the C5 myotome: deltoid and biceps
Image by Lecturio.
Strength testing the C6 myotome: triceps and wrist extensors
Image by Lecturio.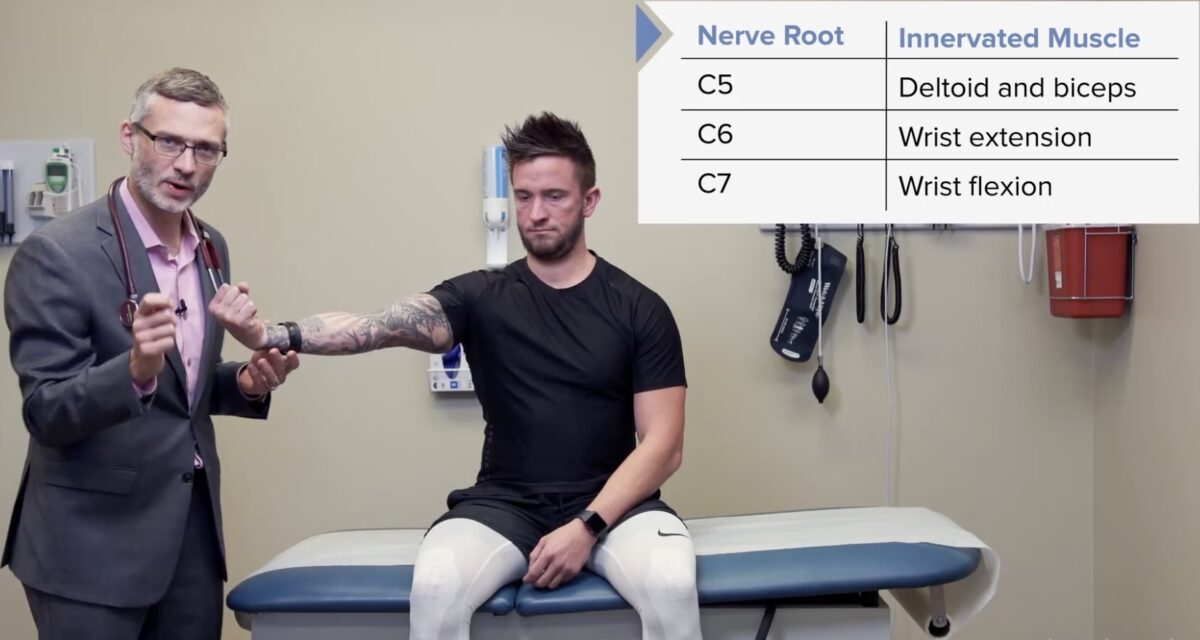
Strength testing the C7 myotome: wrist flexors
Image by Lecturio.
Strength testing the C8 and T1 myotomes: interosseous muscles:
For this test, the subject squeezes the examiner’s fingers.

Strength testing the L2 myotome: hip flexors
Image by Lecturio.
Strength testing the L3 myotome: knee extensors
Image by Lecturio.
Strength testing the L4 myotome: ankle dorsiflexors
Image by Lecturio.
Strength testing the L5 and S1 myotomes: ankle plantar flexors
Image by Lecturio.
Distracting the subject using the Jendrassik maneuver may lead to more reliable reflex testing.
Image by Lecturio.
Reflex testing of the C5 nerve root, biceps tendon reflex
Image by Lecturio.
Reflex testing of the C6 nerve root, brachioradialis tendon reflex
Image by Lecturio.
Reflex testing of the C7 nerve root, triceps tendon reflex
Image by Lecturio.
Reflex testing of the L3 and L4 nerve roots, patellar tendon reflex
Image by Lecturio.
Reflex testing of the L5 and S1 nerve roots, Achilles tendon reflex
Image by Lecturio.Evidence of upper versus lower motor neuron Lower Motor Neuron Motor Neuron Lesions lesions may become evident during motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology examination of the subject due to abnormalities in:
| Upper motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology neuron | Lower motor neuron Lower Motor Neuron Motor Neuron Lesions | |
|---|---|---|
| Site of lesion | Brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy | Anterior horn Anterior horn One of three central columns of the spinal cord. It is composed of gray matter spinal laminae VIII and ix. Brown-Séquard Syndrome, nerve root, peripheral nerve |
| Muscle strength | Weakness | Weakness |
| Muscle tone Muscle tone The state of activity or tension of a muscle beyond that related to its physical properties, that is, its active resistance to stretch. In skeletal muscle, tonus is dependent upon efferent innervation. Skeletal Muscle Contraction | Hypertonic Hypertonic Solutions that have a greater osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation | Flaccid |
| Fasciculations Fasciculations Involuntary contraction of the muscle fibers innervated by a motor unit. Fasciculations may be visualized as a muscle twitch or dimpling under the skin, but usually do not generate sufficient force to move a limb. They may represent a benign condition or occur as a manifestation of motor neuron disease or peripheral nervous system diseases. Polyneuropathy | Absent | Present |
| Deep tendon reflexes | Hyperreflexia | Hyporeflexia Hyporeflexia Duchenne Muscular Dystrophy |

Testing for the Babinski (extensor/plantar) reflex:
The sole of the foot is stroked in a “hockey stick” shape. In a normal (negative) response, the toes will exhibit plantar flexion.
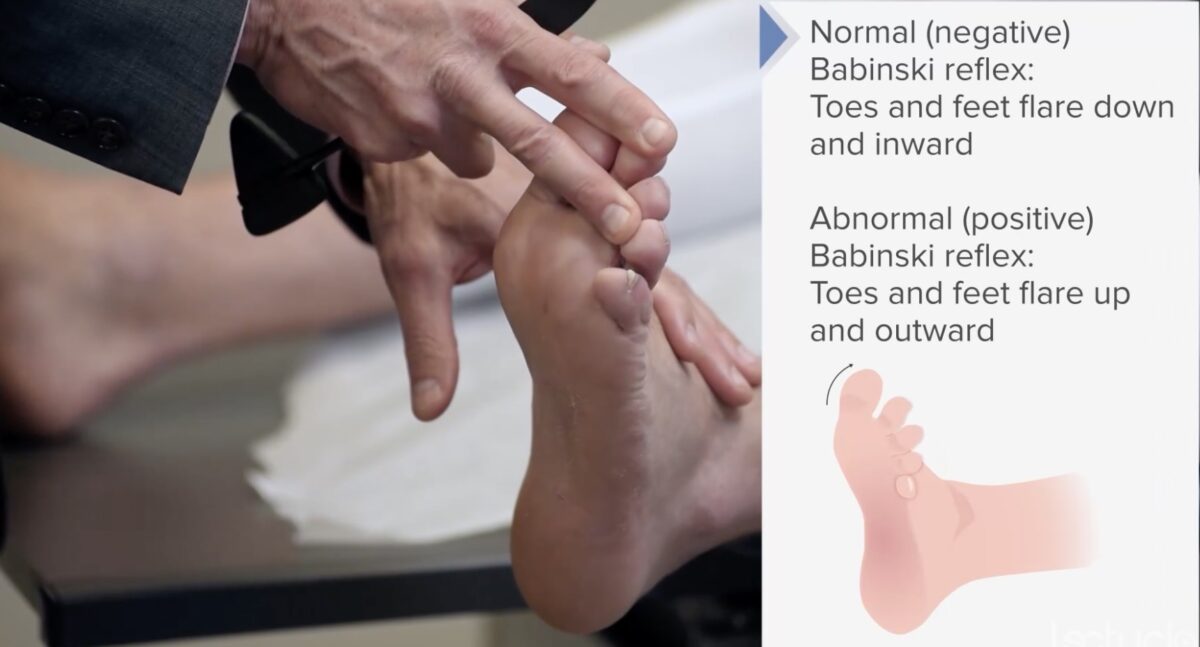
An abnormal (positive) Babinski reflex is a sign of an upper motor neuron lesion.
In an abnormal (positive) response, the great toe will dorsiflex as the other toes fan out.
| Sensation | Pathway | Examination | Abnormal findings |
|---|---|---|---|
| Light touch | Spinothalamic tract | Touch the subject’s body at different locations bilaterally. |
|
| Vibration | Dorsal columns Dorsal Columns Posterior Cord Syndrome | Bony projections tested with a tuning fork | Decreased sensation of vibration indicates peripheral nerve damage. |
| Proprioception | Dorsal columns Dorsal Columns Posterior Cord Syndrome | Identify the positional change of the big toe while moving it up and down. | Abnormal proprioception indicates peripheral nerve damage. |
| Pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and temperature | Spinothalamic tract |
|
Abnormal perception Perception The process by which the nature and meaning of sensory stimuli are recognized and interpreted. Psychiatric Assessment of pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and temperature indicates peripheral nerve damage. |
| Stereognosis | Cerebral cortex Cerebral cortex The cerebral cortex is the largest and most developed part of the human brain and CNS. Occupying the upper part of the cranial cavity, the cerebral cortex has 4 lobes and is divided into 2 hemispheres that are joined centrally by the corpus callosum. Cerebral Cortex: Anatomy | Ask the subject to identify a familiar object with their eyes closed. | Inability to identify a familiar object |
| Graphesthesia | Cerebral cortex Cerebral cortex The cerebral cortex is the largest and most developed part of the human brain and CNS. Occupying the upper part of the cranial cavity, the cerebral cortex has 4 lobes and is divided into 2 hemispheres that are joined centrally by the corpus callosum. Cerebral Cortex: Anatomy | Trace a familiar symbol on the subject’s palm while their eyes are closed. | Inability to identify the symbol |
| Tactile extinction Extinction The procedure of presenting the conditioned stimulus without reinforcement to an organism previously conditioned. It refers also to the diminution of a conditioned response resulting from this procedure. Psychotherapy | Cerebral cortex Cerebral cortex The cerebral cortex is the largest and most developed part of the human brain and CNS. Occupying the upper part of the cranial cavity, the cerebral cortex has 4 lobes and is divided into 2 hemispheres that are joined centrally by the corpus callosum. Cerebral Cortex: Anatomy | Apply a tactile stimulus on each side of body and then bilaterally, and compare perception Perception The process by which the nature and meaning of sensory stimuli are recognized and interpreted. Psychiatric Assessment. | Asymmetry Asymmetry Examination of the Upper Limbs of perception Perception The process by which the nature and meaning of sensory stimuli are recognized and interpreted. Psychiatric Assessment or inability to perceive stimulus on 1 side of the body |

Testing for light touch is often performed using the Semmes-Weinstein monofilament, a useful tool in screening for diabetic polyneuropathy. Here, the examiner is seen testing light touch in the feet.
Image by Lecturio.
Vibratory sense is often assessed using a 120-Hz tuning fork. Here, the examiner is testing the vibratory sensation of the distal lower limb.
Image by Lecturio.
Position sense (proprioception) is tested by asking the subject to detect motion in the digits with their eyes closed. Here, the examiner is testing proprioception of the distal upper limb.
Image by Lecturio.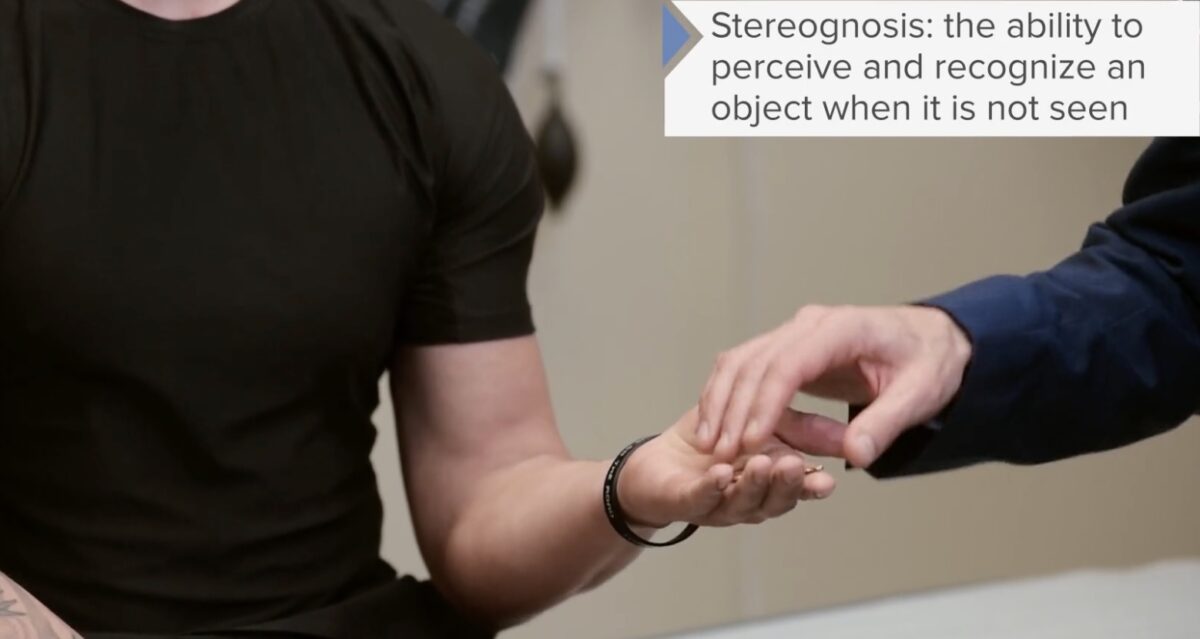
Test for stereognosis (tactile identification of objects with the eyes closed) is often performed by asking the subject to identify a random but familiar object with their eyes closed. Here, the examiner is testing stereognosis with a key.
Image by Lecturio.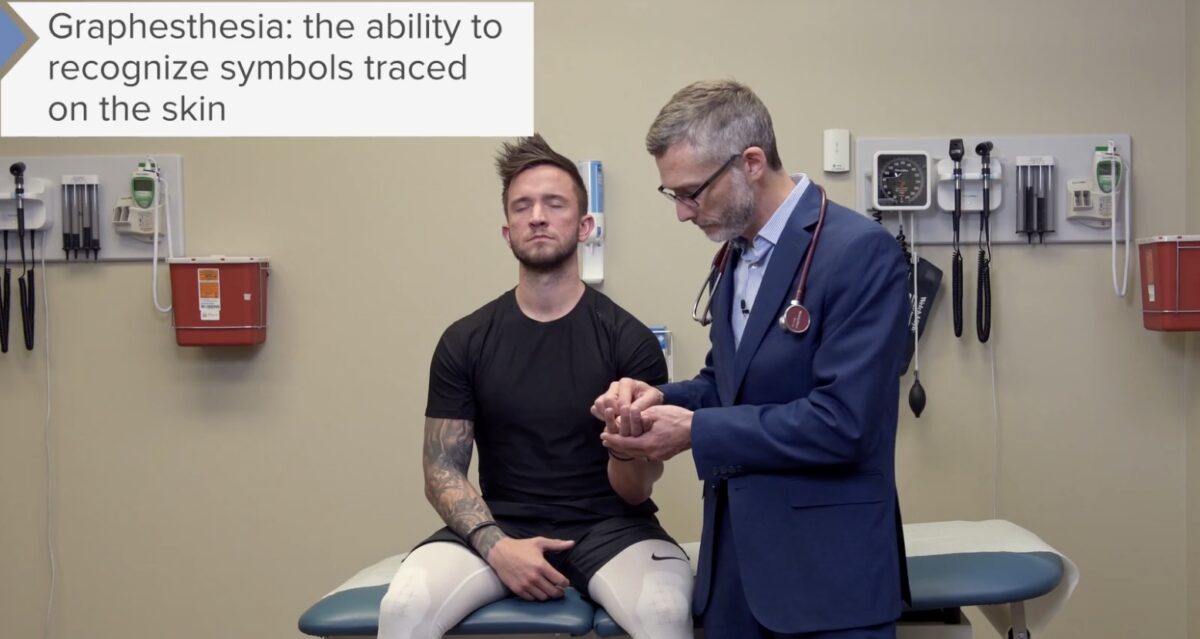
Test for graphesthesia (ability to recognize symbols traced on the skin) is often performed by asking the subject to identify a random but familiar figure drawn on their skin while their eyes are closed. Here, the examiner is testing graphesthesia by drawing an imaginary letter on the subject’s palm.
Image by Lecturio.
Test for tactile extinction (inability to perceive stimuli) is often performed by asking the subject to identify a stimulus on 1 side, then the other, then both simultaneously while their eyes are closed. Here, the examiner is testing extinction by applying a light, stroking motion to the upper limbs.
Image by Lecturio.A cerebellar examination should be performed in any subject exhibiting signs or symptoms of cerebellar pathology including:
There are many causes of cerebellar dysfunction, including:
Cerebellar examination includes the following:
Coordination Coordination Cerebellar Disorders:

Limb ataxia is assessed by having the subject perform the finger-to-nose test.
Image by Lecturio.
Limb ataxia is assessed by having the subject perform the heel-to-shin test.
Image by Lecturio.
Dysdiadochokinesia is assessed by having the subject perform rapid alternating movements.
Image by Lecturio.
The Romberg test helps distinguish ataxia due to peripheral sensory disorders from cerebellar causes of ataxia.
A subject with sensory ataxia will sway during the test, whereas a subject with a cerebellar disorder may not sway until their equilibrium is perturbed. Here, the examiner has introduced a gentle “push” to the subject exhibiting an otherwise negative Romberg test.
Gait assessment:

Testing for gait ataxia is often performed by simply having the subject ambulate across the room.
Image by Lecturio.Many cerebellar syndromes can manifest with gait abnormalities.
| Gait | Description | Associated signs | Causes |
|---|---|---|---|
| Cerebellar |
|
|
|
| Sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology |
|
|
|
| Vestibular |
|
|
|
| Parkinsonian |
|
|
|
| Steppage gait |
|
|
|
| Trendelenburg gait Trendelenburg Gait Legg-Calvé-Perthes Disease/sign |
|
|
|
| Spastic |
|
|
|
The following conditions might be found during neurological examination: