By refraction, the light that enters the eye is focused onto a particular point of the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy. The main refractive components of the eye are the cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy and the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy. When the corneal curvature, the refractive power of the lens Lens A transparent, biconvex structure of the eye, enclosed in a capsule and situated behind the iris and in front of the vitreous humor (vitreous body). It is slightly overlapped at its margin by the ciliary processes. Adaptation by the ciliary body is crucial for ocular accommodation. Eye: Anatomy, does not match the size of the eye, ametropia or a refractive error Error Refers to any act of commission (doing something wrong) or omission (failing to do something right) that exposes patients to potentially hazardous situations. Disclosure of Information occurs. The types of refractive errors include myopia (nearsightedness), hyperopia (farsightedness), and astigmatism (which can occur in both myopia and hyperopia). The use of a proper refractive device helps correct the visual impairment. Laser in situ keratomileusis (LASIK) is the most common corrective surgical procedure.
Last updated: May 17, 2024
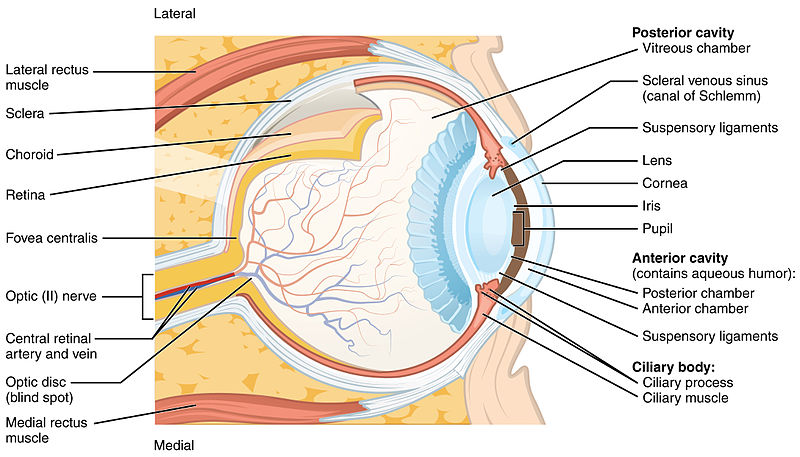
Structure of the eye
Image: “Structure of the Eye” by OpenStax College. License: CC BY 3.0| Myopia | Hyperopia | Astigmatism | |
|---|---|---|---|
| Focal point | In front of retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy | Behind retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy | Multiple sites |
| Causes | Eye too long, cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy with too much curvature | Eye too short, cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy with too little curvature | Uneven curvature of the cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy |
| Result | Cannot focus distant objects | Cannot focus near objects | Blurry vision Vision Ophthalmic Exam |
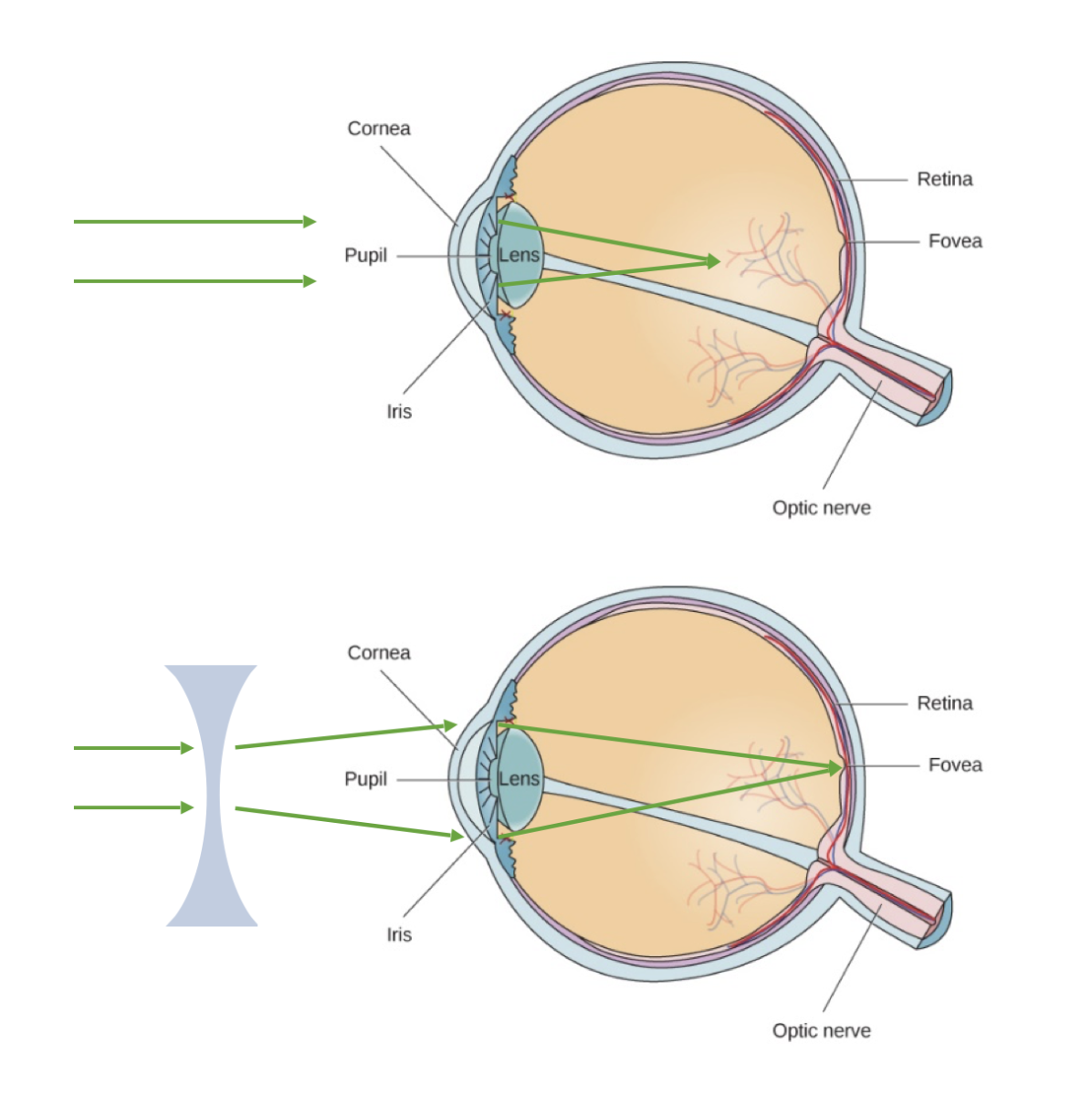
This figure illustrates myopia (nearsightedness). The top image shows light as it is refracted too sharply by the cornea, resulting in a focal point in front of the retina.
With corrective negative lenses (bottom image), the light can be dispersed through the concave lens and focus appropriately onto the retina for clear vision.
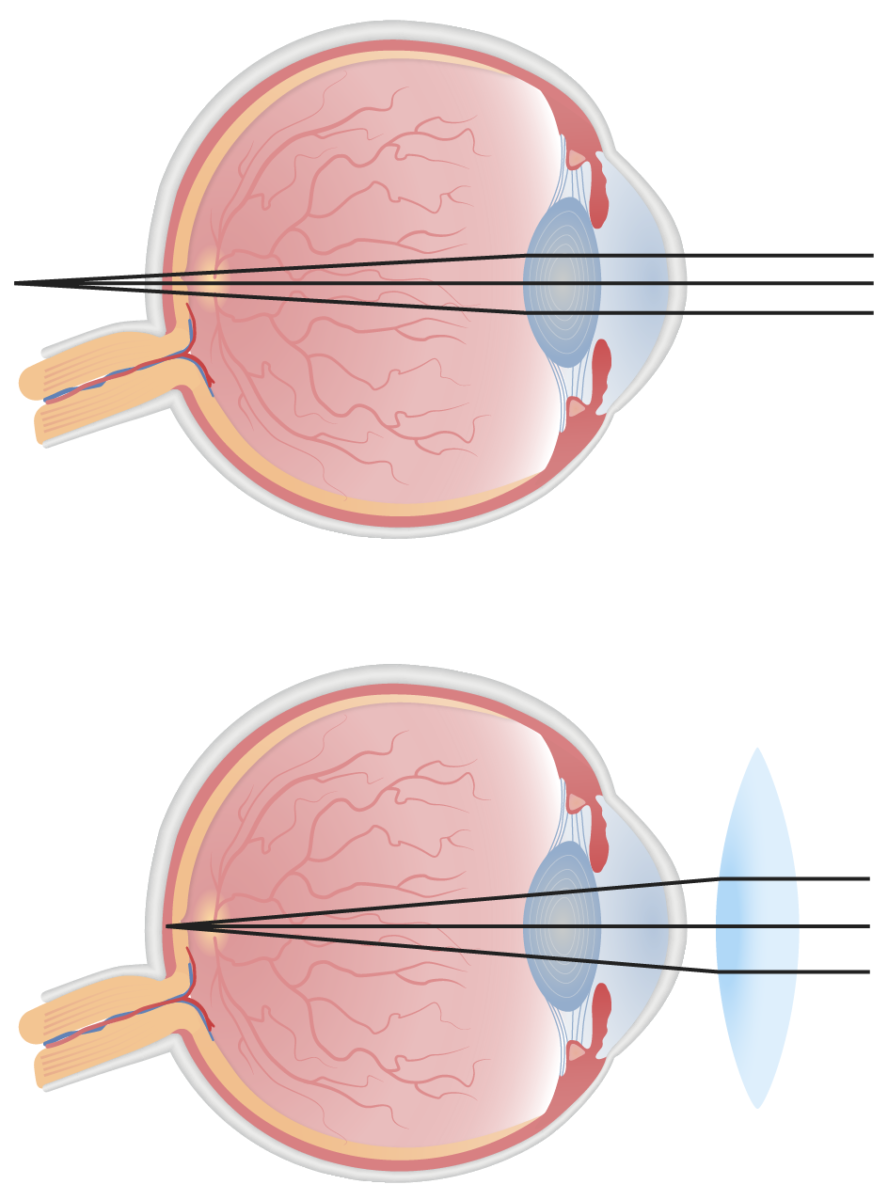
This figure illustrates hyperopia (farsightedness). The top image illustrates uncorrected refraction, where the light is not refracted sharply enough, resulting in a focal point behind the retina.
With corrective positive lenses (bottom image), the light can be dispersed through the convex lens and focus appropriately onto the retina for clear vision.
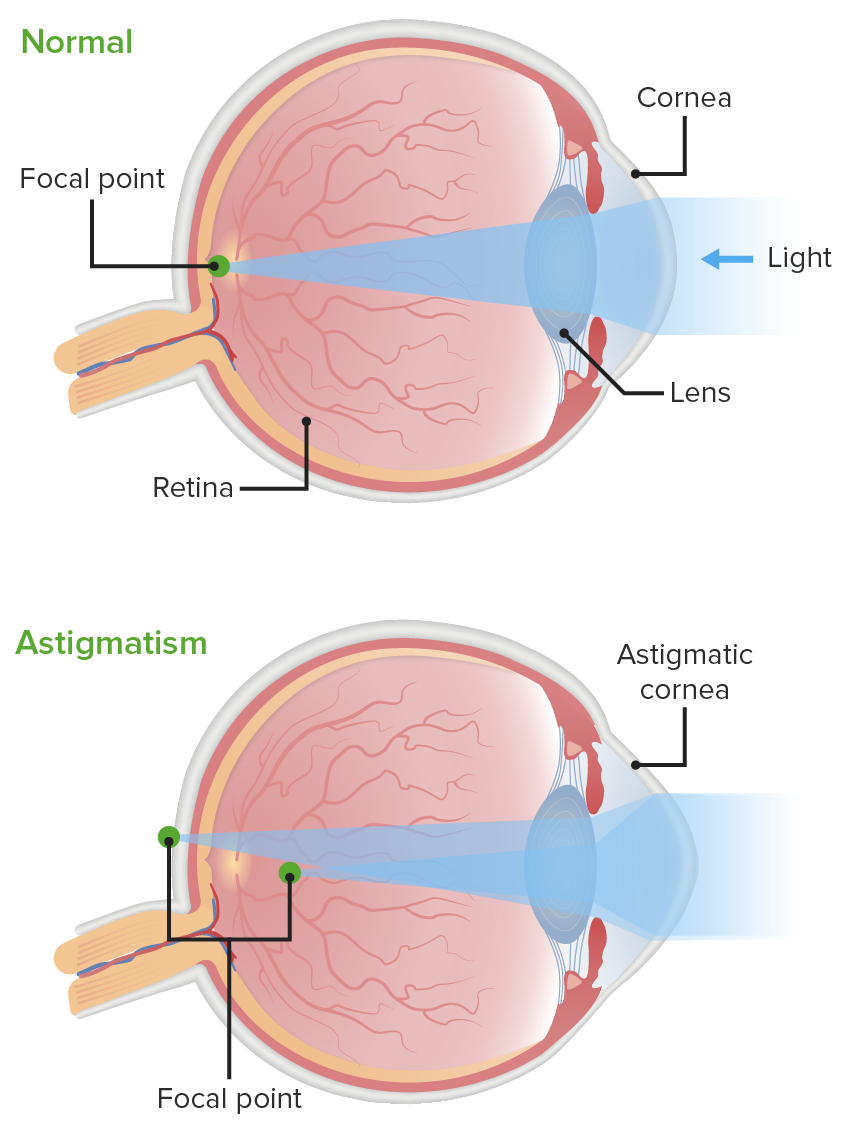
This figure contrasts the normal corneal curvature with that of an astigmatic cornea. The cornea with astigmatism distorts the focus point of light in front of and/or behind the retina.
Image by Lecturio.Myopia
Hyperopia
Astigmatism
Presbyopia
Example:
A patient with hyperopia, more on the left, also with astigmatism in both eyes, would be given the following prescription:
The differential diagnosis of refractive errors includes the following conditions: