Retinal detachment is the separation of the neurosensory retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy from the retinal pigmented epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology and choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy. Rhegmatogenous retinal detachment, the most common type, stems from a break in the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy, allowing fluid to accumulate in the subretinal space. In the setting of an intact retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy, detachment occurs when the vitreous pulls on the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy (traction) or when an underlying condition leads to increased leakage of fluid (exudative). Symptoms of photopsia Photopsia Chorioretinitis, floaters Floaters Chorioretinitis, and visual defects can present over hours or gradually over weeks. Retinal detachment with visual loss is an emergency. Once macular detachment occurs, visual prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is poor. Symptomatic rhegmatogenous retinal detachment with intact central acuity warrants urgent surgery. For non-rhegmatogenous retinal detachments, treatment is directed toward the primary process.
Last updated: May 17, 2024
Retinal detachment is the separation of the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy from the underlying retinal pigment epithelium Retinal Pigment Epithelium The single layer of pigment-containing epithelial cells in the retina, situated closely to the tips (outer segments) of the retinal photoreceptor cells. These epithelial cells are macroglia that perform essential functions for the photoreceptor cells, such as in nutrient transport, phagocytosis of the shed photoreceptor membranes, and ensuring retinal attachment. Hypertensive Retinopathy and choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy.
Retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy:
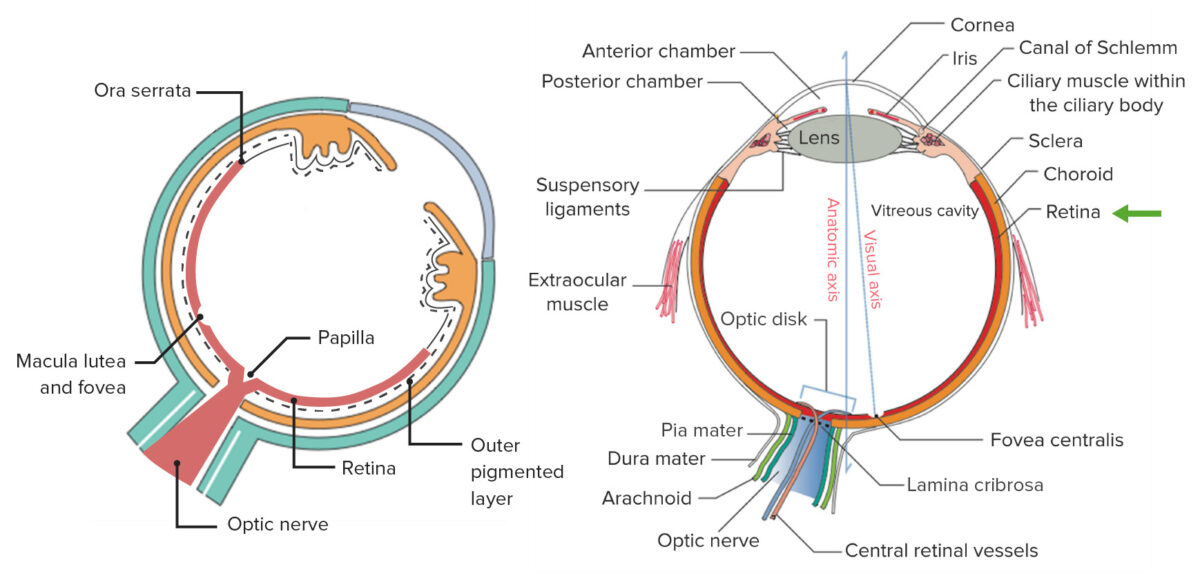
Left: the components of the innermost, neural, and sensory layers of the eye
Right: general structure of the eye
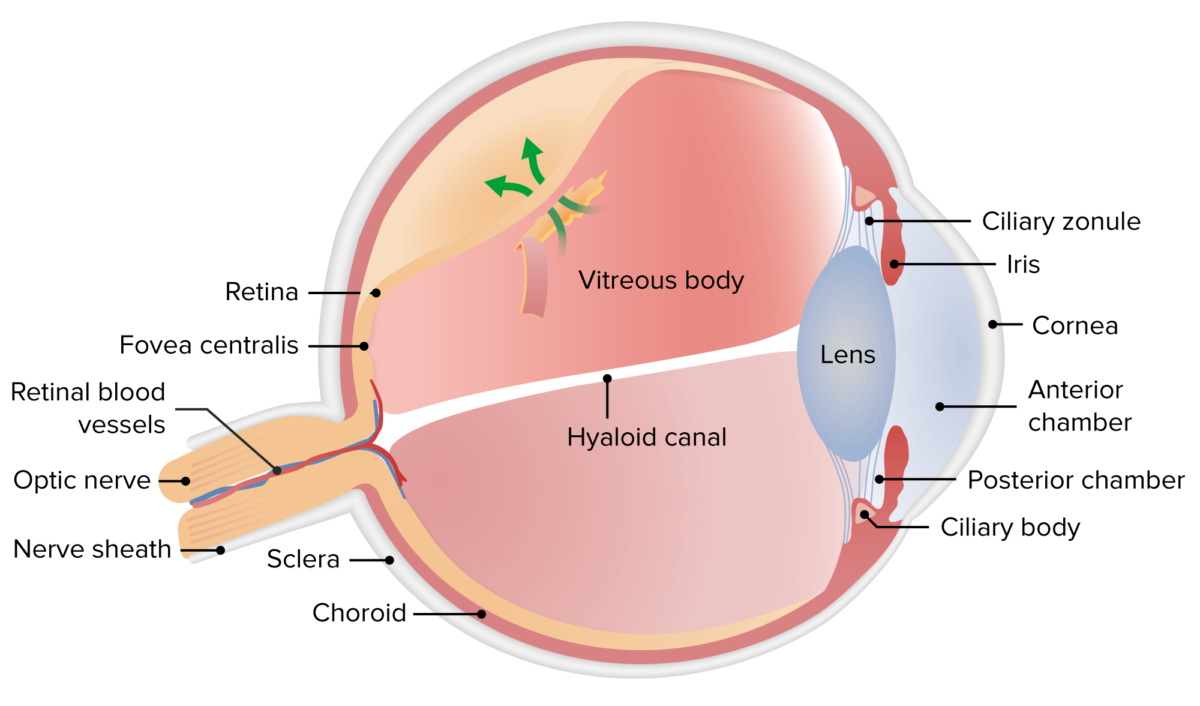
The image shows a retinal break (tear) where fluid can enter the subretinal space.
Image by Lecturio.
The image shows a retinal break, which allows fluid to enter and accumulate in the subretinal space. This predisposes the patient to a rhegmatogenous type of retinal detachment.
Image by Lecturio.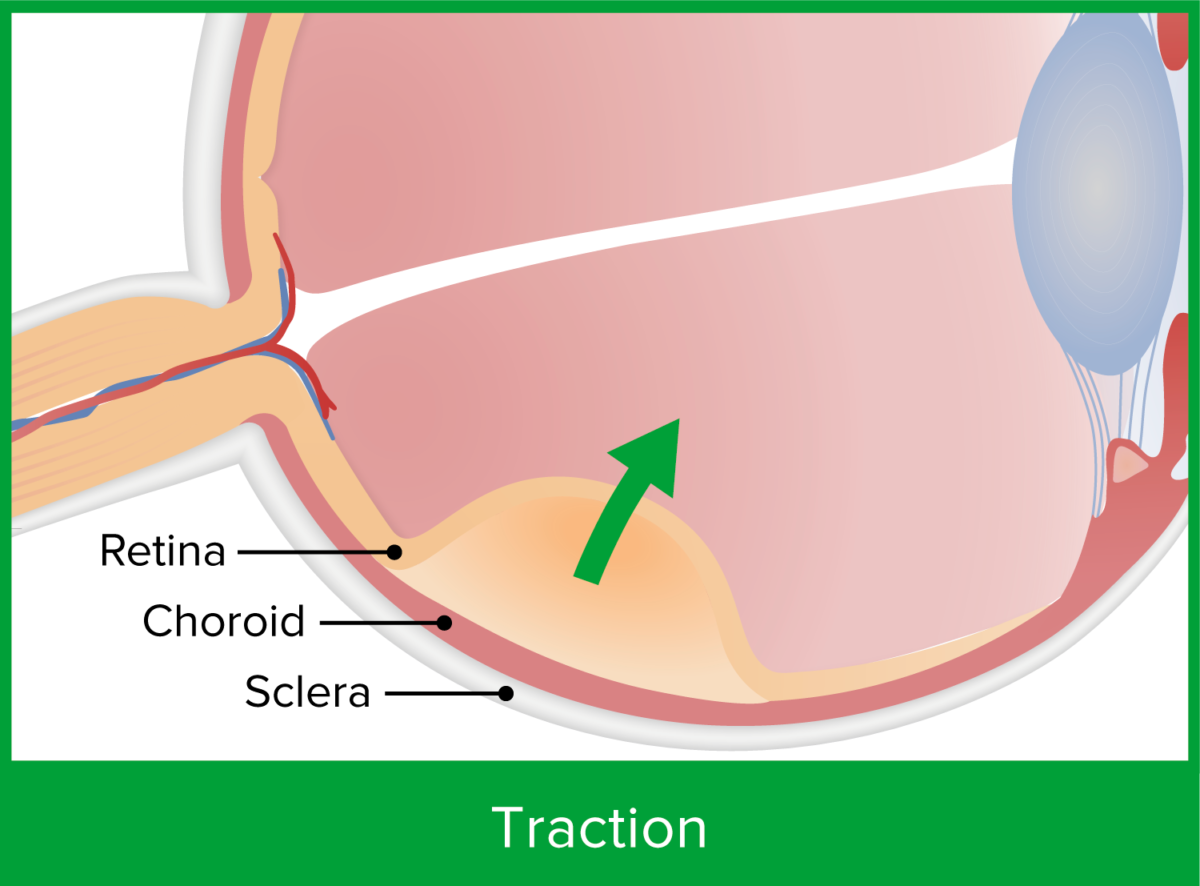
A strongly attached vitreous or a proliferative membrane pulls on the retina, causing traction detachment.
Image by Lecturio.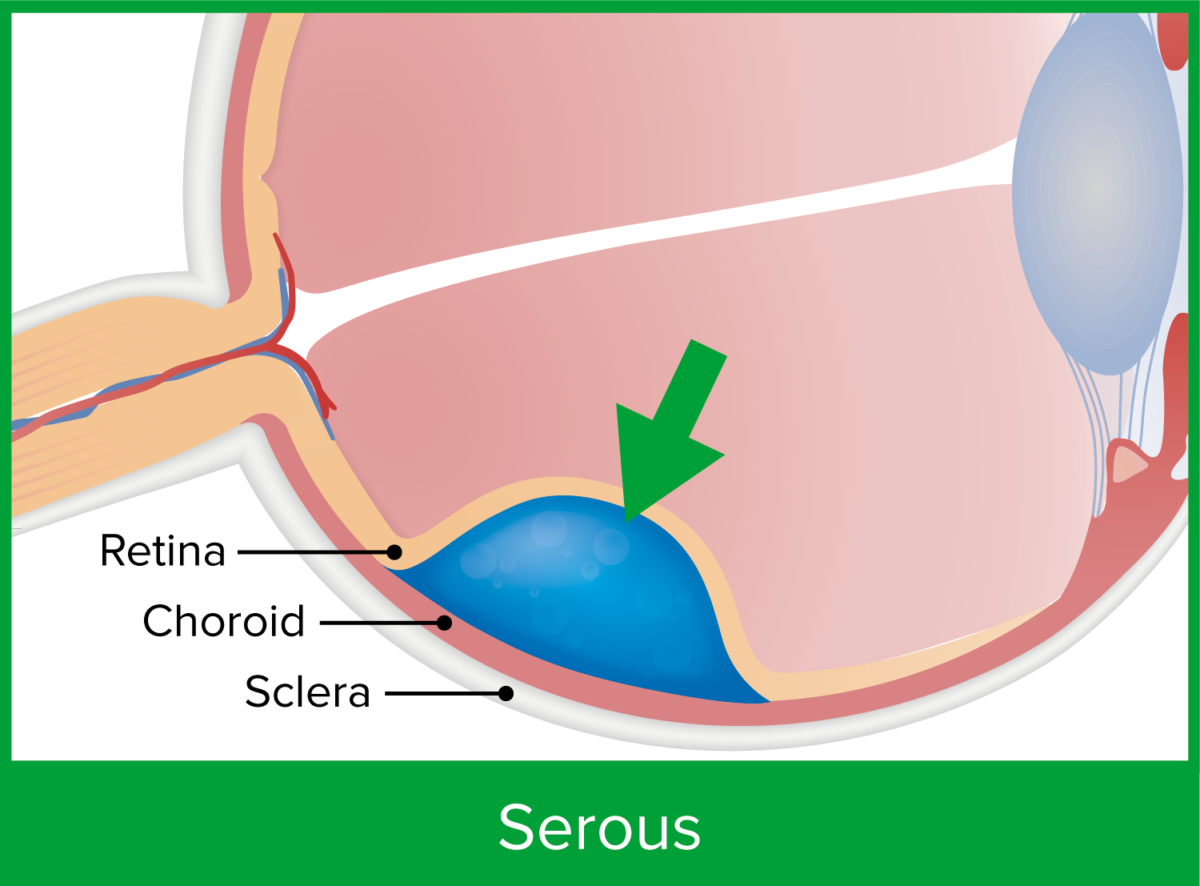
Exudative or serous retinal detachment results from impaired fluid outflow or increased vascular permeability due to an underlying condition or disease.
Image by Lecturio.| Symptom | Cause |
|---|---|
| Photopsia Photopsia Chorioretinitis | Vitreoretinal traction |
| Floaters Floaters Chorioretinitis | Vitreous cells, blood |
| Visual field Visual Field The Visual Pathway and Related Disorders loss or defect | Peripheral detachment |
| Blurred vision Vision Ophthalmic Exam or loss of central vision Vision Ophthalmic Exam | Macular detachment |
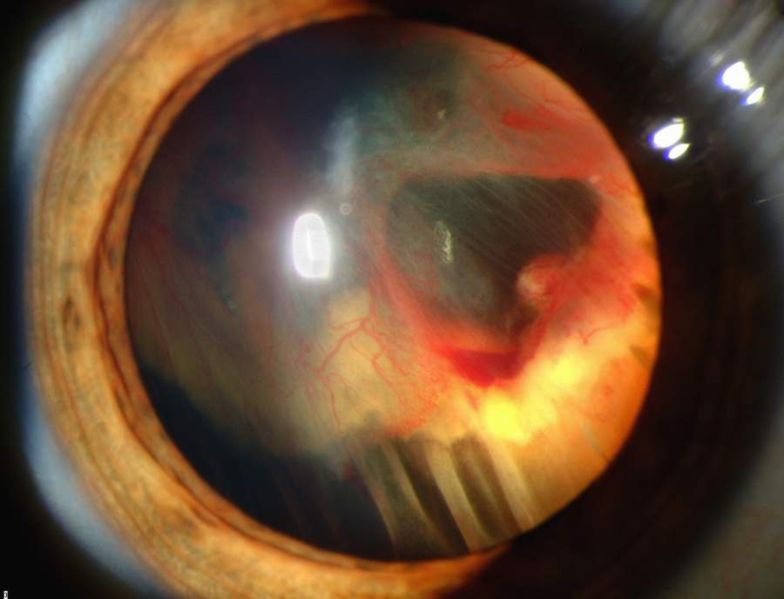
Slit-lamp photograph showing retinal detachment with vitreous hemorrhage
Image: “Slit lamp photograph showing retinal detachment” by National Eye Institute/National Institutes of Health. License: Public Domain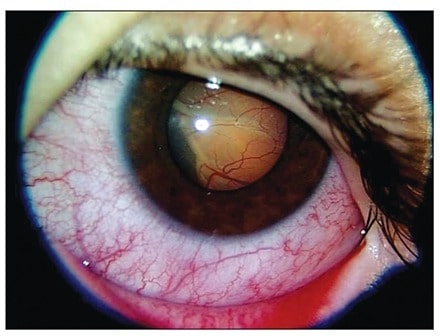
Slit-lamp photograph of the left eye showing exudative retinal detachment in the lower nasal area. Retinal detachment is secondary to acute lymphoblastic leukemia.
Image: “Slit-lamp photograph of the left eye at presentation” by Diskapi Children’s Hospital, Department of Pediatric Hematology, Ankara, Turkey. License: CC BY 2.5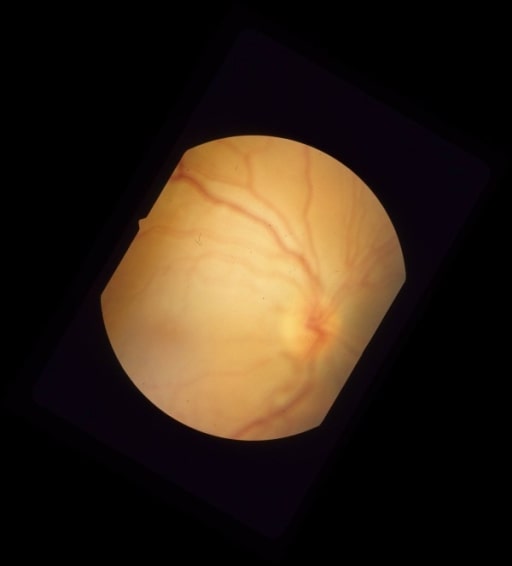
Color fundus photograph of the eye showing macula-off rhegmatogenous retinal detachment due to a necrotic retinal hole from a flat choroidal lesion inferior to the inferotemporal arcade
Image: “Pre-operative color fundus photograph of the right eye” by University of Southern California and Doheny Eye Institute, Los Angeles, California 90033, USA. License: CC BY 2.0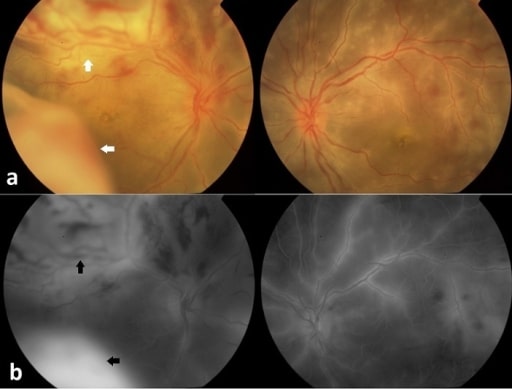
Unilateral bullous exudative retinal detachment in Behçet’s disease. Funduscopy and fluorescein angiography:
(a) Extensive perivascular sheathing with scattered yellowish retinal infiltrates and hemorrhages in both eyes, with a bullous exudative retinal detachment involving the superior and inferior quadrants of the temporal retina in the right eye (white arrows)
(b) Fluorescein angiography showing late staining of the retinal vasculature with diffuse dye leakage in both eyes and fluorescein pooling in the subretinal space in the right eye (black arrows)
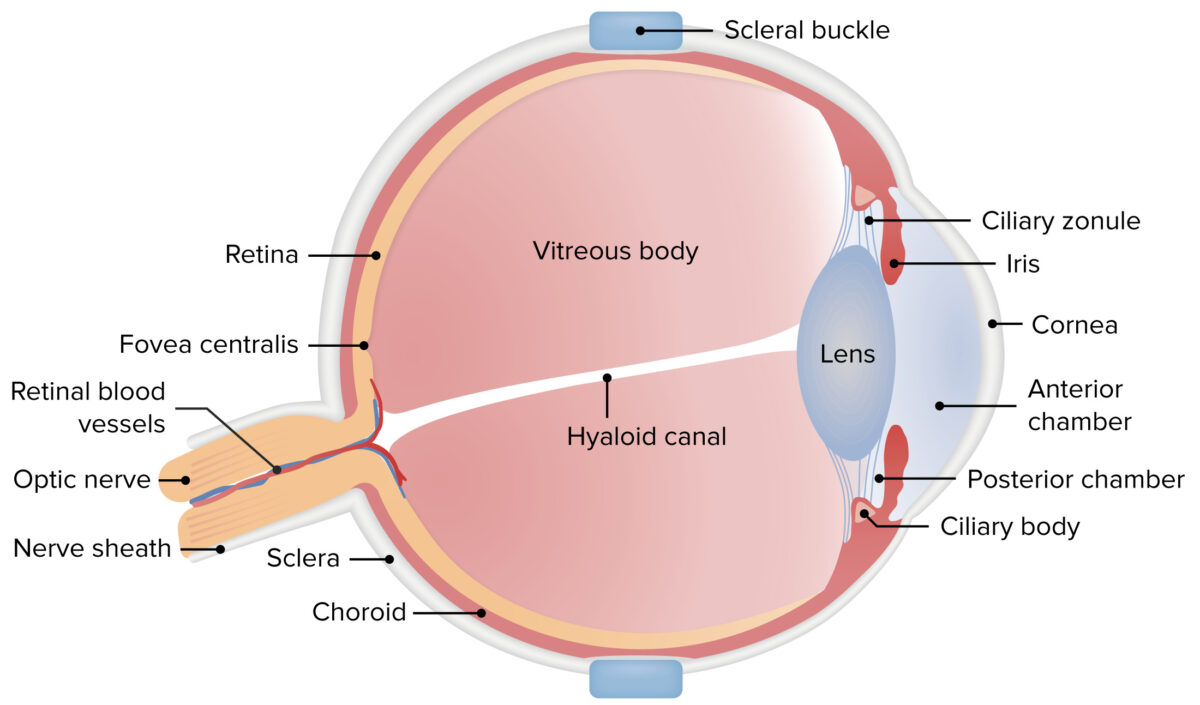
The image illustrates scleral buckling, the placement of a pliable silicone sutured to the sclera. Scleral buckling pushes the sclera inward, thereby keeping the separated structures closer and allowing the retina to reattach.
Image by Lecturio.