Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Felines are the definitive host, but transmission to humans can occur through contact with cat feces or the consumption of contaminated foods. The clinical presentation and complications depend on the host’s immune status. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are immunocompetent usually have no symptoms, whereas those who are immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis may develop CNS toxoplasmosis CNS toxoplasmosis Infections of the brain caused by the protozoan toxoplasma gondii that primarily arise in individuals with immunologic deficiency syndromes. The infection may involve the brain diffusely or form discrete abscesses. Clinical manifestations include seizures, altered mentation, headache, focal neurologic deficits, and intracranial hypertension. AIDS-defining Conditions or chorioretinitis Chorioretinitis Chorioretinitis is the inflammation of the posterior segment of the eye, including the choroid and the retina. The condition is usually caused by infections, the most common of which is toxoplasmosis. Some of these infections can affect the fetus in utero and present as congenital abnormalities. Chorioretinitis. The diagnosis is often made based on serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus or PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are immunocompetent may not need any treatment. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis or those with severe disease may require combination therapy with pyrimethamine Pyrimethamine One of the folic acid antagonists that is used as an antimalarial or with a sulfonamide to treat toxoplasmosis. Antimalarial Drugs, sulfadiazine Sulfadiazine One of the short-acting sulfonamides used in combination with pyrimethamine to treat toxoplasmosis in patients with acquired immunodeficiency syndrome and in newborns with congenital infections. Sulfonamides and Trimethoprim, and leucovorin.
Last updated: Feb 28, 2025
General characteristics:
Morphologic forms:
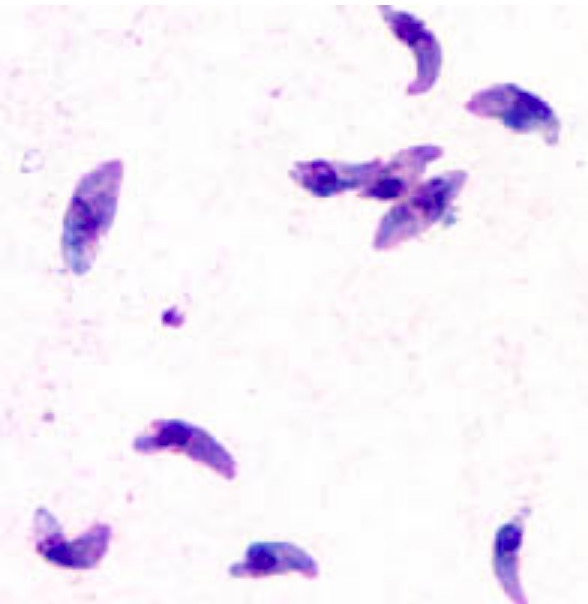
Toxoplasma gondii tachyzoites stained with Giemsa:
Tachyzoites are typically crescent shaped with a prominent, centrally placed nucleus.
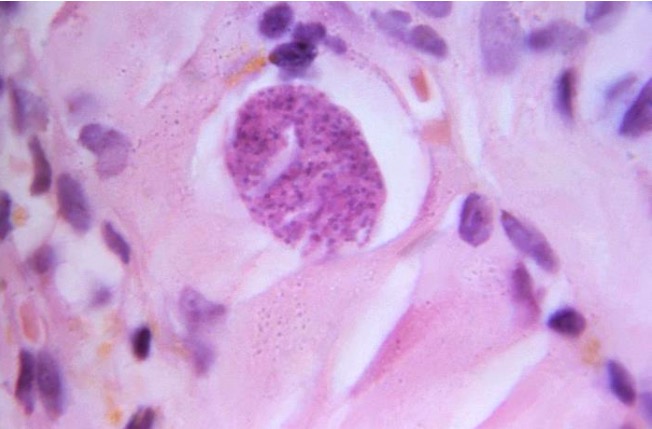
A hematoxylin and eosin-stained (H&E) photomicrograph of a Toxoplasma gondii tissue cyst containing developing bradyzoites in human muscle tissue
Image: “16547” by CDC/Dr. Martin Hicklin. License: Public DomainToxoplasmosis is caused by Toxoplasma gondii.
Life cycle:
Life cycle and pathophysiology in humans:
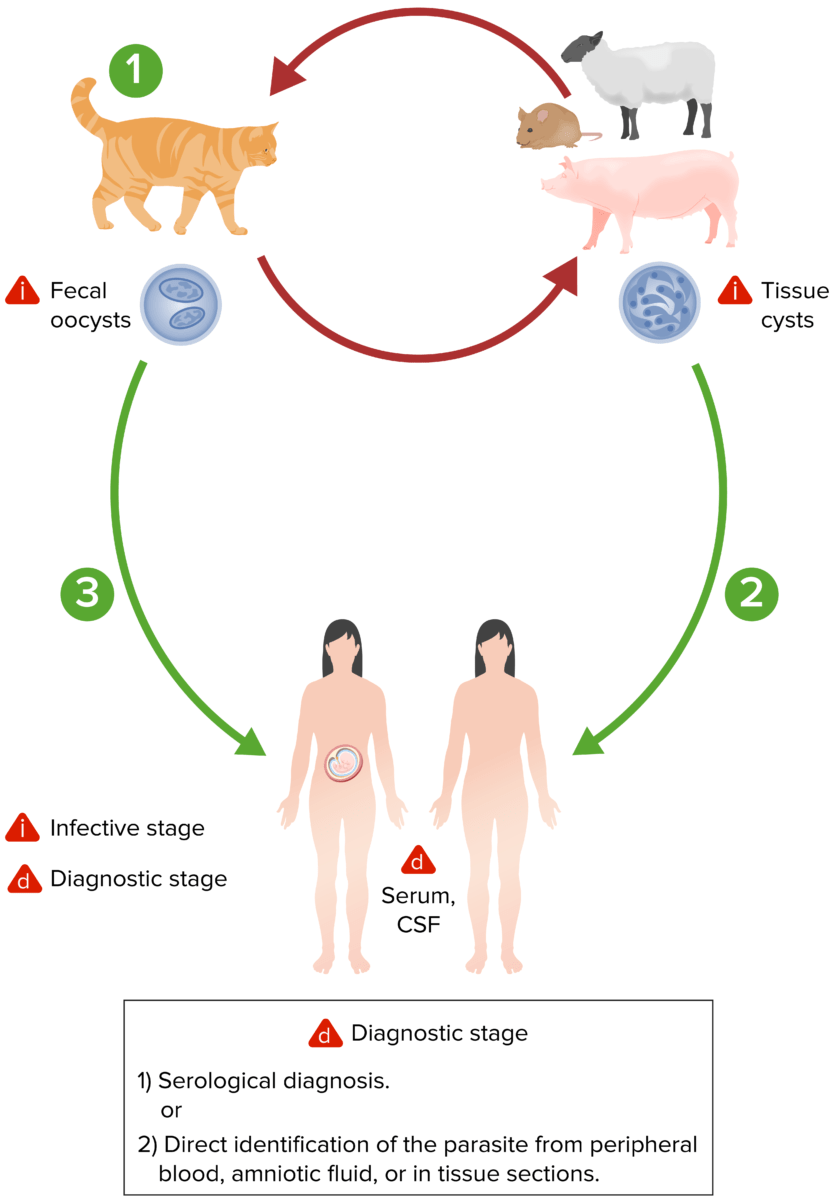
The lifecycle of Toxoplasma gondii. Both oocysts and tissue cysts transform into tachyzoites shortly after ingestion. Tachyzoites localize in neural and muscle tissue and develop into tissue-cyst bradyzoites. If a pregnant woman becomes infected, tachyzoites can infect the fetus via the bloodstream.
Image by Lecturio.The clinical presentation of toxoplasmosis can vary depending on the host’s immune function and organs involved. The following table summarizes the various diseases:
| Host | Disease | Presentation |
|---|---|---|
| Immunocompetent host | Subclinical infection (approximately 90% of cases) | Asymptomatic |
| Acute systemic disease | Common signs and symptoms:
|
|
| Immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis host (e.g., AIDS) | CNS toxoplasmosis CNS toxoplasmosis Infections of the brain caused by the protozoan toxoplasma gondii that primarily arise in individuals with immunologic deficiency syndromes. The infection may involve the brain diffusely or form discrete abscesses. Clinical manifestations include seizures, altered mentation, headache, focal neurologic deficits, and intracranial hypertension. AIDS-defining Conditions (AIDS-defining illness, CD4 count < 100 cells/µL) |
|
| Chorioretinitis Chorioretinitis Chorioretinitis is the inflammation of the posterior segment of the eye, including the choroid and the retina. The condition is usually caused by infections, the most common of which is toxoplasmosis. Some of these infections can affect the fetus in utero and present as congenital abnormalities. Chorioretinitis | Symptoms:
|
|
| Pneumonitis Pneumonitis Human Herpesvirus 6 and 7 |
|
|
| Fetus, newborn Newborn An infant during the first 28 days after birth. Physical Examination of the Newborn, or infant | Congenital toxoplasmosis | Classic triad:
|
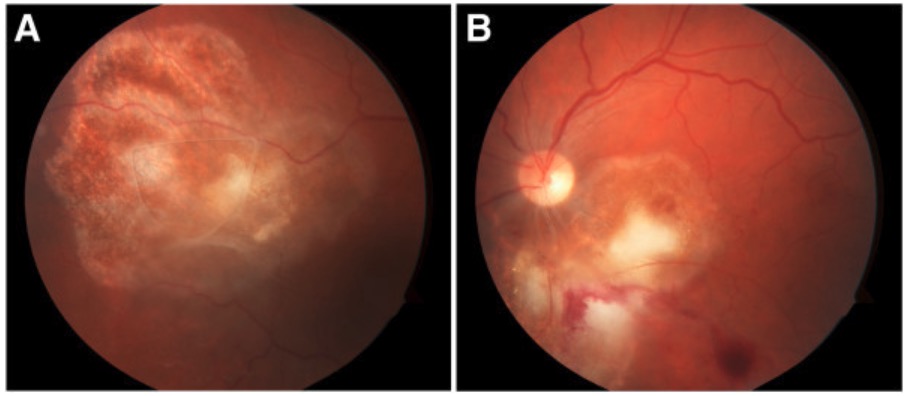
Fundoscopy of Toxoplasma chorioretinitis:
Note the yellow-white cotton lesions in both the right eye (A) and left eye (B).
The diagnostic workup will be guided by the patient’s clinical presentation.
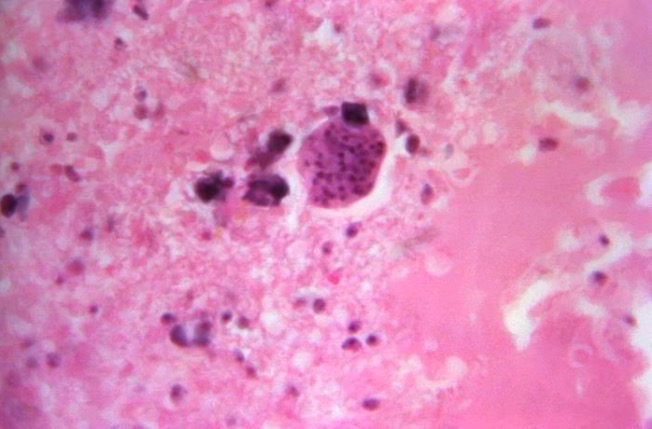
Photomicrograph of a Toxoplasma gondii tissue cyst in a brain tissue specimen
Image: “16543” by CDC/Dr. Martin Hicklin. License: Public DomainBrain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification imaging may be performed if CNS or congenital toxoplasmosis is suspected.
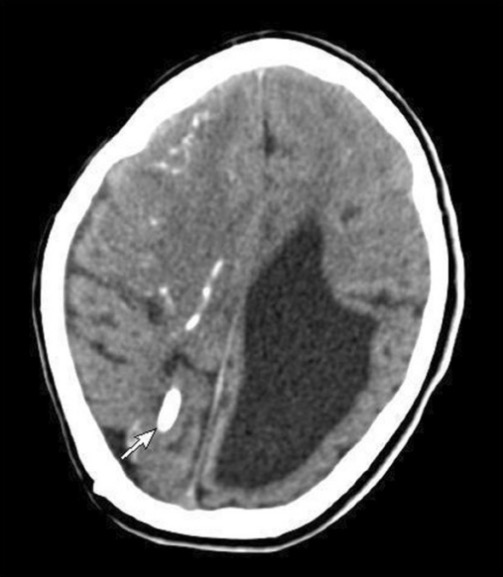
A CT image showing parenchymal calcification (arrow), multiple subependymal calcifications, and dilated ventricles due to congenital toxoplasmosis
Image: “Computerized tomography of brain” by Department of Pediatrics (39), College of Medicine, King Saud University, PO Box 2925, 11461 Riyadh, Saudi Arabia. License: CC BY 2.0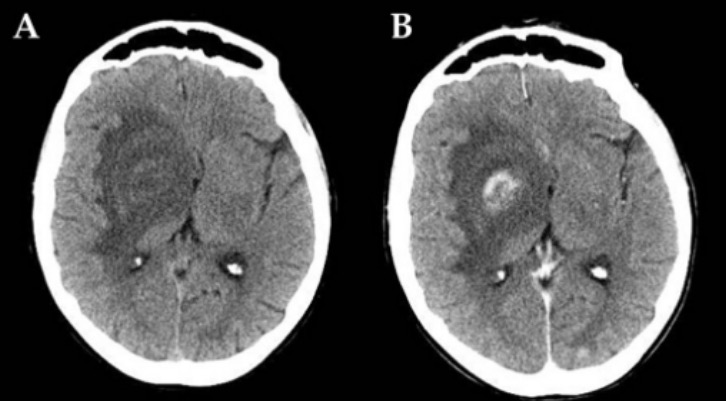
Case of AIDS-related CNS toxoplasmosis:
A CT scan of toxoplasmic localization in the right capsulonuclear region with wide perilesional edema before (A) and after (B) contrast injection
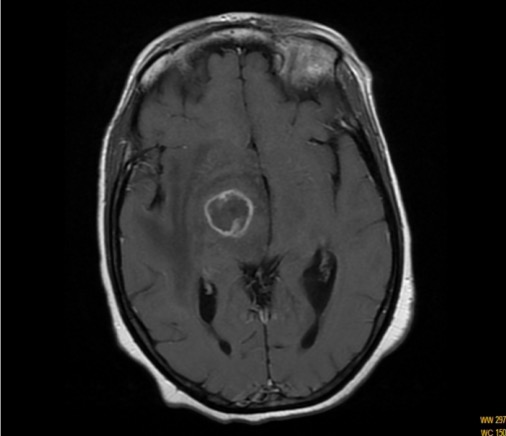
An MRI image of CNS toxoplasmosis in a patient with AIDS: T1-weighted MRI scan showing a ring-enhancing lesion
Image: “T1-weighted magnetic resonance imaging scan” by Department of Internal Medicine, Hassan II University Hospital, Faculty of Medicine and Pharmacy, University Sidi Mohammed Ben Abdellah, Morocco. License: CC BY 2.0Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are immunocompetent typically do not require treatment. However, treatment is needed for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis, pregnant, or with severe or prolonged symptoms.