The sulfonamides are a class of antimicrobial drugs inhibiting folic acid synthesis Synthesis Polymerase Chain Reaction (PCR) in pathogens. The prototypical drug in the class is sulfamethoxazole. Although not technically sulfonamides, trimethoprim, dapsone Dapsone A sulfone active against a wide range of bacteria but mainly employed for its actions against Mycobacterium leprae. Its mechanism of action is probably similar to that of the sulfonamides which involves inhibition of folic acid synthesis in susceptible organisms. It is also used with pyrimethamine in the treatment of malaria. Antimycobacterial Drugs, and pyrimethamine Pyrimethamine One of the folic acid antagonists that is used as an antimalarial or with a sulfonamide to treat toxoplasmosis. Antimalarial Drugs are also important antimicrobial agents inhibiting folic acid synthesis Synthesis Polymerase Chain Reaction (PCR). The agents are often combined with sulfonamides, resulting in a synergistic effect. The primary indication for use is treatment of urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infection (although significant resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing has emerged). In addition, the drugs are used to treat and prevent opportunistic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease such as toxoplasmosis Toxoplasmosis Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Felines are the definitive host, but transmission to humans can occur through contact with cat feces or the consumption of contaminated foods. The clinical presentation and complications depend on the host's immune status. Toxoplasma/Toxoplasmosis encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis and pneumocystis pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia in immunosuppressed individuals. The most common adverse events are hypersensitivity reactions, fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, rash Rash Rocky Mountain Spotted Fever, GI upset, and hematologic reactions. The drugs are generally contraindicated in pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, young/ill infants, and individuals with megaloblastic anemia Megaloblastic anemia Megaloblastic anemia is a subset of macrocytic anemias that arises because of impaired nucleic acid synthesis in erythroid precursors. This impairment leads to ineffective RBC production and intramedullary hemolysis that is characterized by large cells with arrested nuclear maturation. The most common causes are vitamin B12 and folic acid deficiencies. Megaloblastic Anemia or severe renal impairment.
Last updated: Oct 6, 2022
Sulfonamide antibiotics are antimicrobial drugs containing a sulfonamide functional group.
Drugs with a mechanism of action similar to sulfonamide antibiotics (but not technically sulfonamides):
Combination drugs (work synergistically):
Sulfonamide antibiotics contain a sulfonamide functional group, which is a sulfur bonded to:
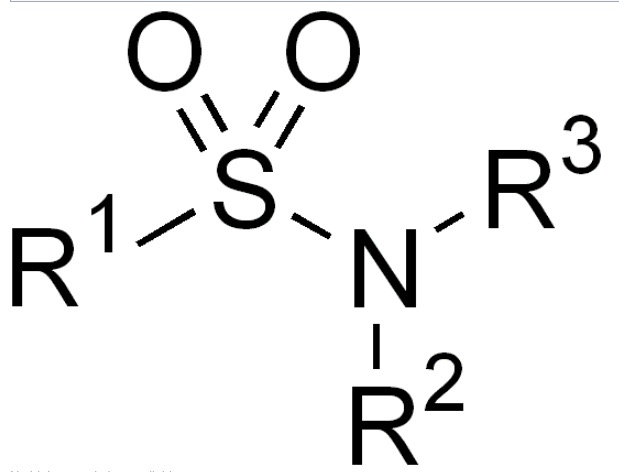
Chemical structure of sulfonamide
Image: “Sulfonamide” by Edgar181. License: Public Domain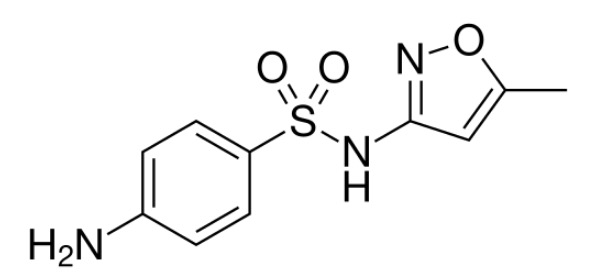
Chemical structure of sulfamethoxazole
Image: “Sulfamethoxazole” by Vaccinationist. License: Public Domain, cropped by Lecturio.
Chemical structure of trimethoprim
Image: “Trimethoprim” by Vaccinationist. License: Public Domain, cropped by Lecturio.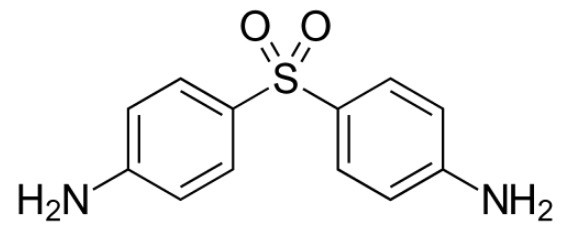
Chemical structure of dapsone
Image: “Dapsone” by Fvasconcellos. License: Public Domain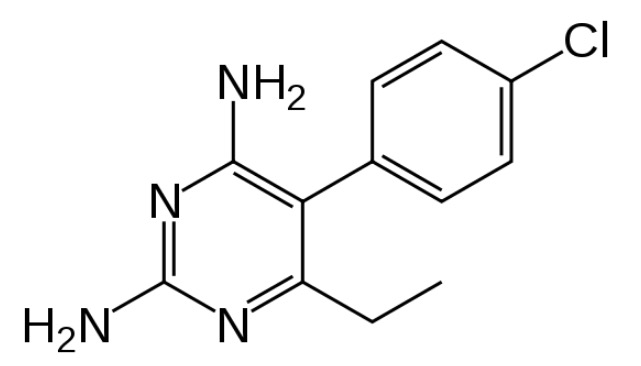
Chemical structure of pyrimethamine
Image: “Pyrimethamine” by Fvasconcellos. License: Public DomainSulfonamides, trimethoprim, dapsone Dapsone A sulfone active against a wide range of bacteria but mainly employed for its actions against Mycobacterium leprae. Its mechanism of action is probably similar to that of the sulfonamides which involves inhibition of folic acid synthesis in susceptible organisms. It is also used with pyrimethamine in the treatment of malaria. Antimycobacterial Drugs, and pyrimethamine Pyrimethamine One of the folic acid antagonists that is used as an antimalarial or with a sulfonamide to treat toxoplasmosis. Antimalarial Drugs disrupt folic acid synthesis Synthesis Polymerase Chain Reaction (PCR) in microbes.
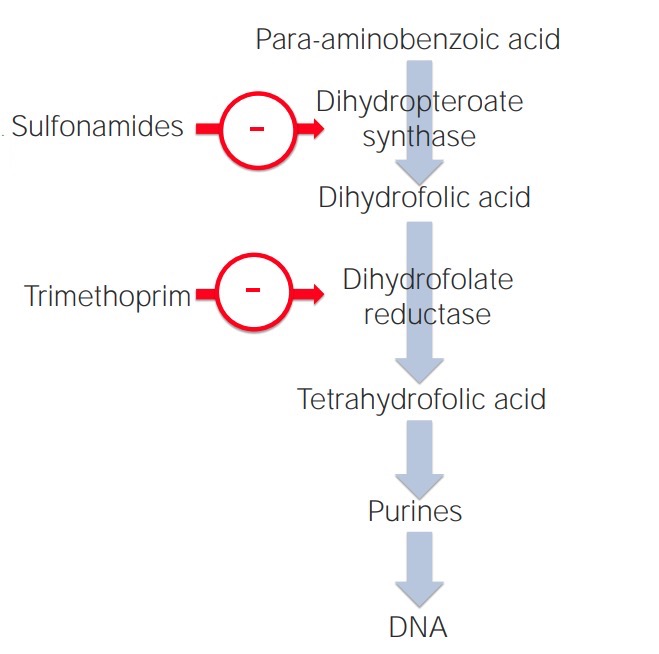
Mechanism of action of sulfonamides and trimethoprim in the folic acid pathway
Image by Lecturio. License: CC BY-NC-SA 4.0Due to significant resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing, especially against TMP-SMX, the agents are best used after antibiotic-susceptibility testing. Activity may be against:
Antibiotics can be classified in several ways. One way is to classify antibiotics by mechanism of action.
| Mechanism | Class of antibiotics |
|---|---|
| Bacterial cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic synthesis Synthesis Polymerase Chain Reaction (PCR) inhibitors |
|
| Bacterial protein synthesis Synthesis Polymerase Chain Reaction (PCR) inhibitors |
|
| Agents acting against DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure and/or folate Folate Folate and vitamin B12 are 2 of the most clinically important water-soluble vitamins. Deficiencies can present with megaloblastic anemia, GI symptoms, neuropsychiatric symptoms, and adverse pregnancy complications, including neural tube defects. Folate and Vitamin B12 |
|
| Antimycobacterial agents Antimycobacterial Agents Antimycobacterial agents represent a diverse group of compounds that have activity against mycobacterial infections, including tuberculosis, leprosy and Mycobacterium avium complex (MAC) disease. The 1st-line agents for tuberculosis are rifampin, isoniazid, pyrazinamide, and ethambutol. Antimycobacterial Drugs |
|
Different antibiotics have varying degrees of activity against different bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology. The table below outlines the antibiotics with activity against 3 important classes of bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology: gram-positive Gram-Positive Penicillins cocci Cocci Bacteriology, gram-negative bacilli Bacilli Shigella, and anaerobes Anaerobes Lincosamides.
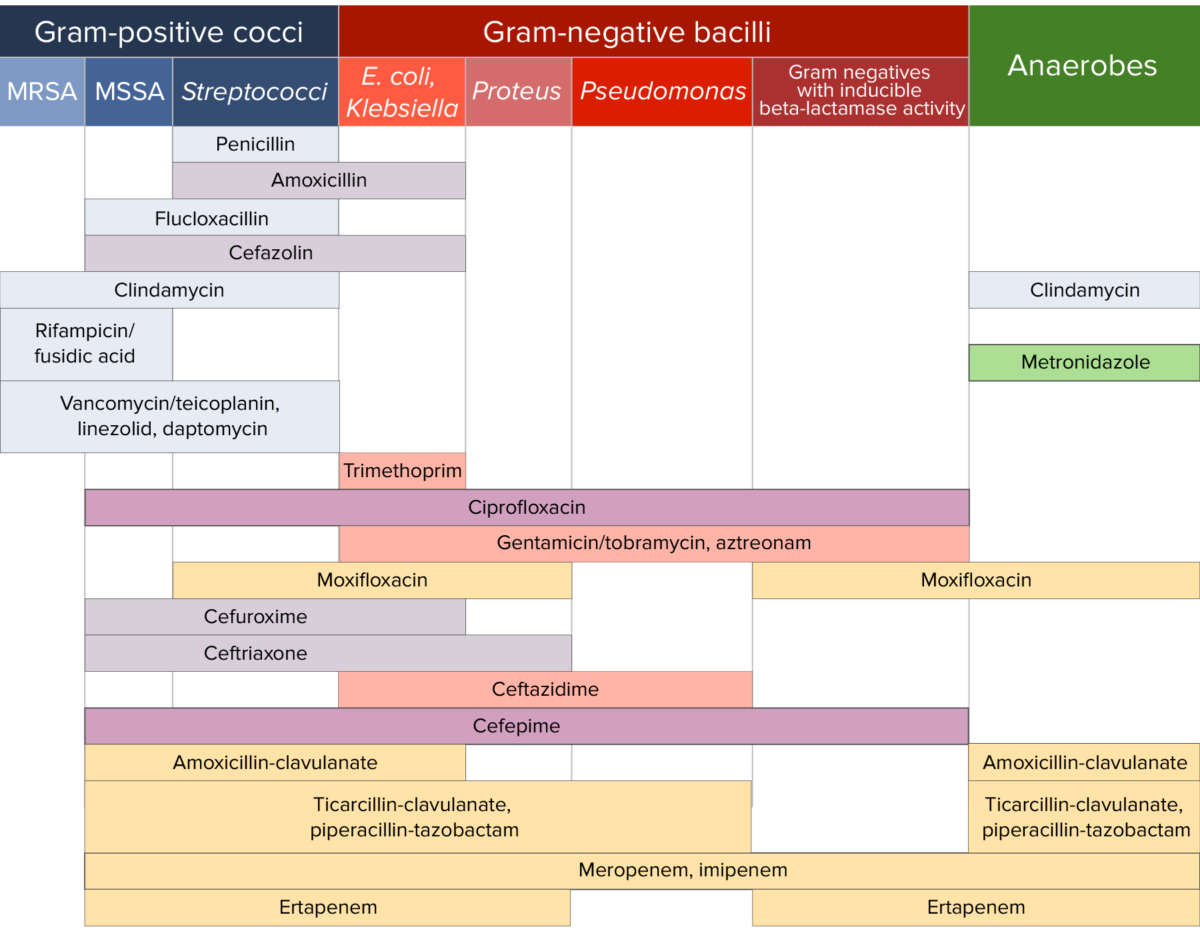
Antibiotic sensitivity:
Chart comparing the microbial coverage of different antibiotics for gram-positive cocci, gram-negative bacilli, and anaerobes.