Chloramphenicol, the only clinically relevant drug in the amphenicol class, is a potent inhibitor of bacterial protein synthesis by binding to the 50S ribosomal subunit and preventing peptide bond formation. Chloramphenicol is a broad-spectrum Broad-Spectrum Fluoroquinolones antibiotic with wide distribution; however, due to its toxicity Toxicity Dosage Calculation, its use is limited to severe infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease where another alternative antibiotic is not available (usually due to resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing issues). Adverse effects include optic neuritis Optic neuritis Inflammation of the optic nerve. Commonly associated conditions include autoimmune disorders such as multiple sclerosis, infections, and granulomatous diseases. Clinical features include retro-orbital pain that is aggravated by eye movement, loss of color vision, and contrast sensitivity that may progress to severe visual loss, an afferent pupillary defect (Marcus-Gunn pupil), and in some instances optic disc hyperemia and swelling. Inflammation may occur in the portion of the nerve within the globe (neuropapillitis or anterior optic neuritis) or the portion behind the globe (retrobulbar neuritis or posterior optic neuritis). Cranial Nerve Palsies, aplastic anemia Aplastic Anemia Aplastic anemia (AA) is a rare, life-threatening condition characterized by pancytopenia and hypocellularity of the bone marrow (in the absence of any abnormal cells) reflecting damage to hematopoietic stem cells. Aplastic anemia can be acquired or inherited, however, most cases of AA are acquired and caused by autoimmune damage to hematopoietic stem cells. Aplastic Anemia, and gray baby syndrome.
Last updated: Feb 13, 2025
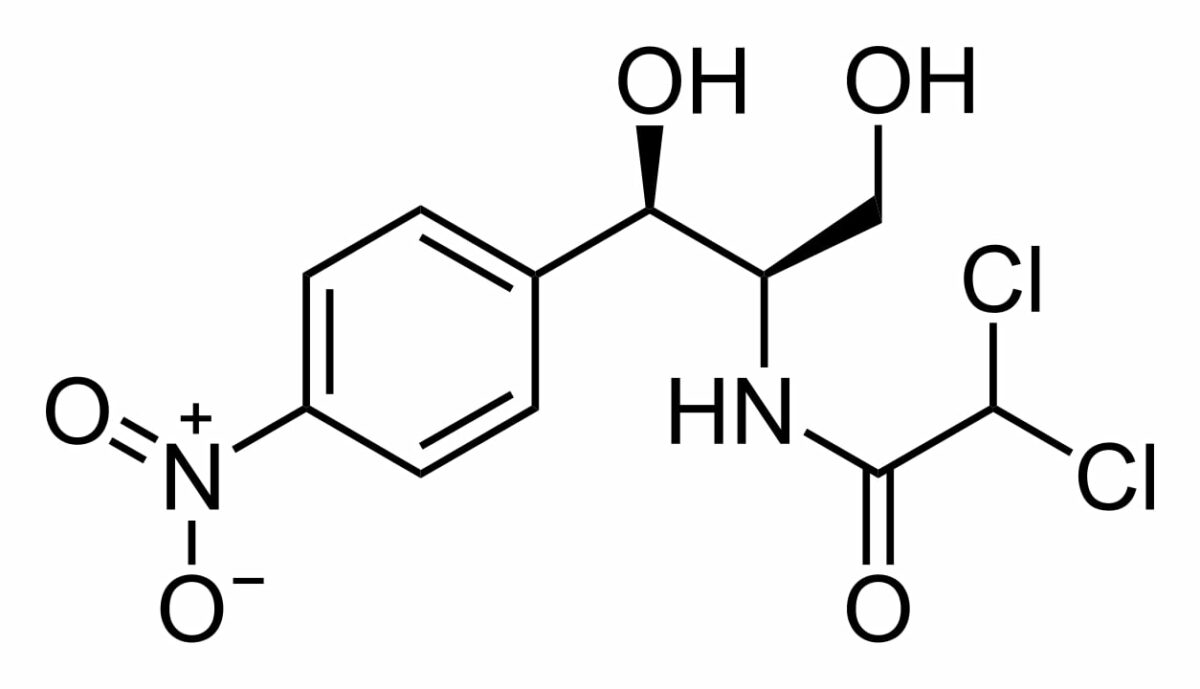
Chemical structure of chloramphenicol
Image: “Chemical structure of chloramphenicol” by Calvero. License: Public Domain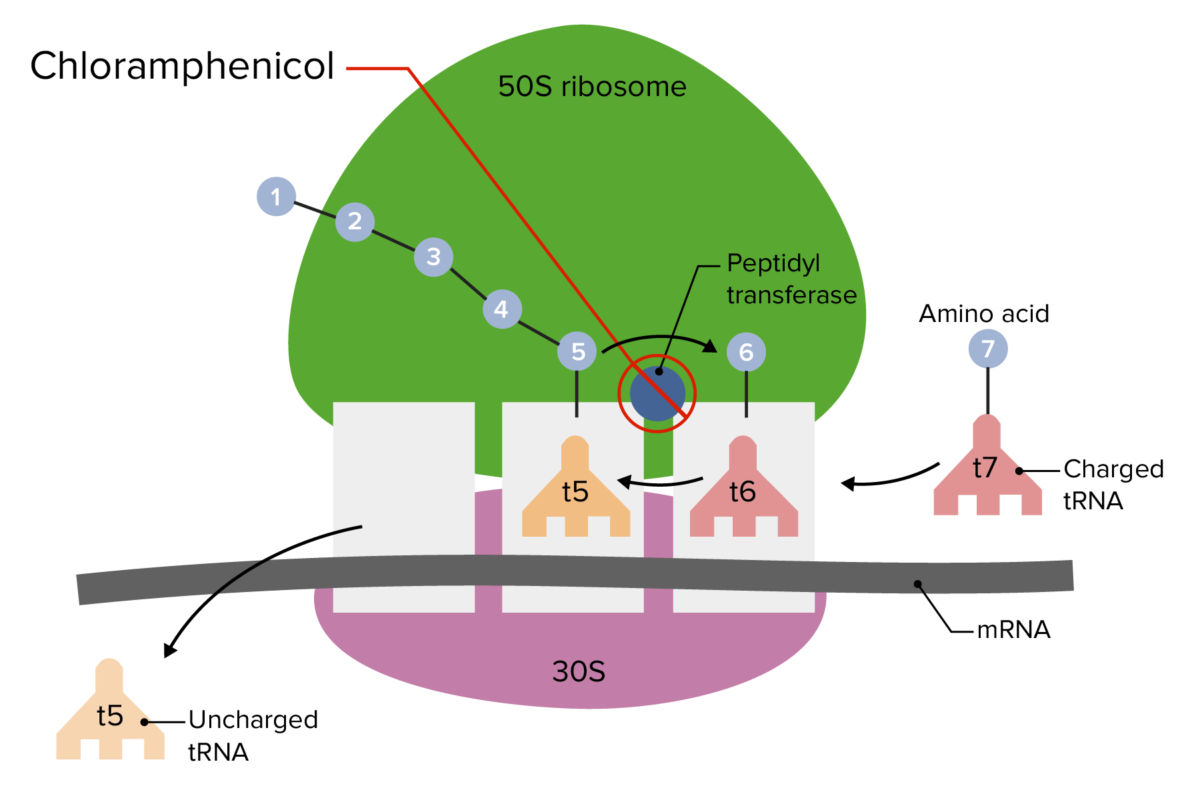
Site of action for chloramphenicol on the 50S ribosomal subunit:
This prevents linkage of amino acids to the peptide chain, resulting in inhibition of protein synthesis.
tRNA: transfer RNA
Because of chloramphenicol’s side effects, use is generally limited to severe infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease where resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing has developed against alternative agents:
Resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing mechanisms to chloramphenicol in bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology include:
| Drug class | Mechanism of action | Coverage | Adverse effects |
|---|---|---|---|
| Amphenicols |
|
|
|
| Lincosamides Lincosamides The lincosamides, lincomycin and clindamycin, are inhibitors of bacterial protein synthesis. Drugs in this class share the same binding site as that of macrolides and amphenicols; however, they differ in chemical structure. Lincosamides target the 50S ribosomal subunit and interfere with transpeptidation. Lincosamides |
|
|
|
| Macrolides Macrolides Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit and blocking transpeptidation. These antibiotics have a broad spectrum of antimicrobial activity but are best known for their coverage of atypical microorganisms. Macrolides and Ketolides |
|
|
|
| Oxazolidinones Oxazolidinones The oxazolidinones (linezolid and tedizolid) are bacterial protein synthesis inhibitors. Their unique binding site on the 23S ribosomal RNA of the 50S ribosome gives them zero cross-resistance with other antibiotics. Oxazolidinones |
|
Gram-positive
Gram-Positive
Penicillins
cocci
Cocci
Bacteriology:
|
|
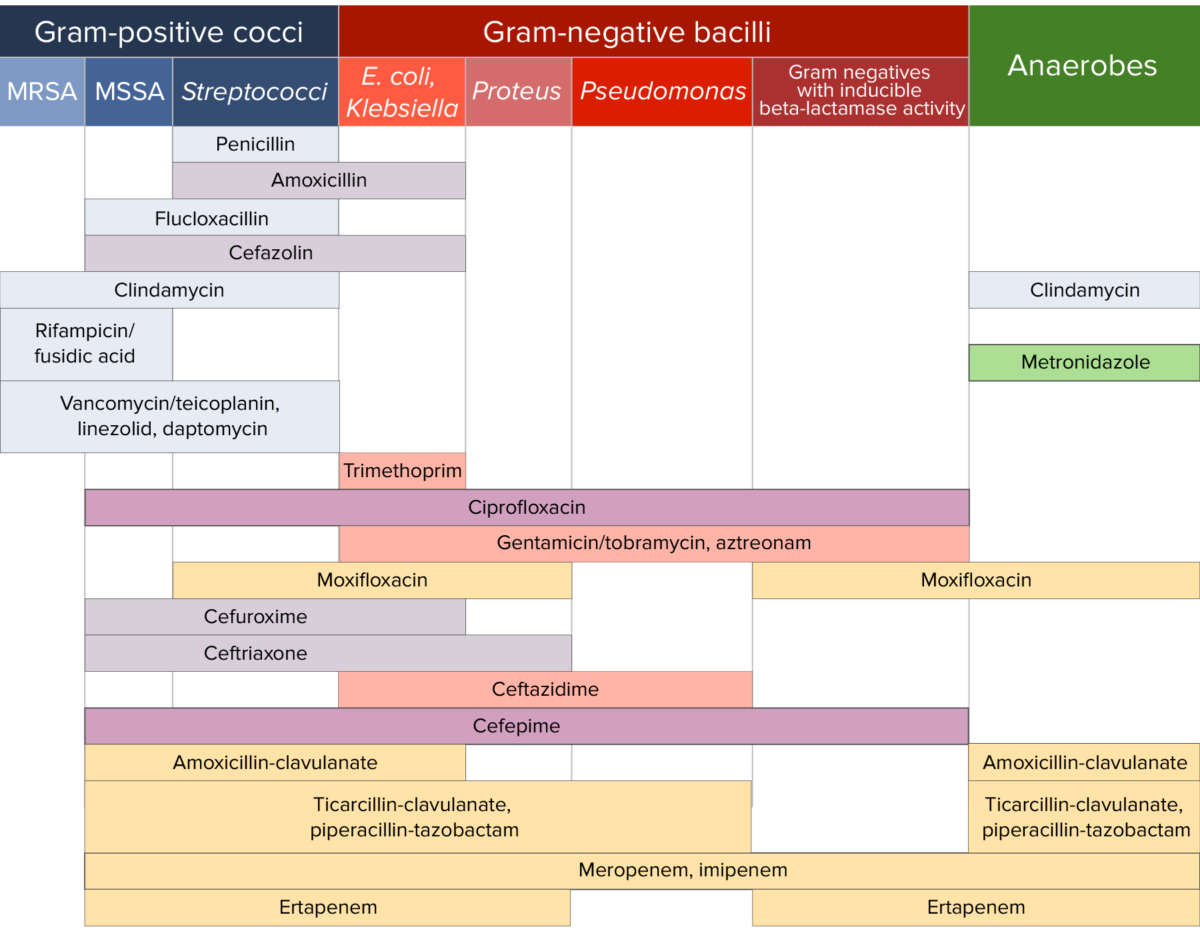
Antibiotic sensitivity:
Chart comparing the microbial coverage of different antibiotics for gram-positive cocci, gram-negative bacilli, and anaerobes.