Staphylococcus is a medically important genera of Gram-positive Gram-Positive Penicillins, aerobic cocci Cocci Bacteriology. These bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology form clusters resembling grapes on culture plates. Staphylococci are ubiquitous for humans, and many strains compose the normal skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions flora. Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess is the most virulent species; S. epidermidis and S. saprophyticus are less virulent but are also clinically significant. Infection can cause a wide array of disease, including cellulitis Cellulitis Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. Cellulitis, abscesses, endocarditis Endocarditis Endocarditis is an inflammatory disease involving the inner lining (endometrium) of the heart, most commonly affecting the cardiac valves. Both infectious and noninfectious etiologies lead to vegetations on the valve leaflets. Patients may present with nonspecific symptoms such as fever and fatigue. Endocarditis, osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis, and medical device infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Toxins formed by S. aureus can cause gastroenteritis Gastroenteritis Gastroenteritis is inflammation of the stomach and intestines, commonly caused by infections from bacteria, viruses, or parasites. Transmission may be foodborne, fecal-oral, or through animal contact. Common clinical features include abdominal pain, diarrhea, vomiting, fever, and dehydration. Gastroenteritis, SSSS SSSS Staphylococcal scalded skin syndrome (SSSS), also known as Ritter disease and staphylococcal epidermal necrolysis, is a toxin-mediated condition caused by Staphylococcus aureus. The exfoliative toxin produced disseminates and cleaves desmoglein 1 in the epidermis, causing separation and detachment of the skin. Staphylococcal Scalded Skin Syndrome (SSSS), and toxic shock syndrome Toxic Shock Syndrome Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing. Toxic Shock Syndrome ( TSS TSS Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing. Toxic Shock Syndrome). Antibiotic management varies based on the type of infection, severity, and sensitivity data.
Last updated: Dec 29, 2023
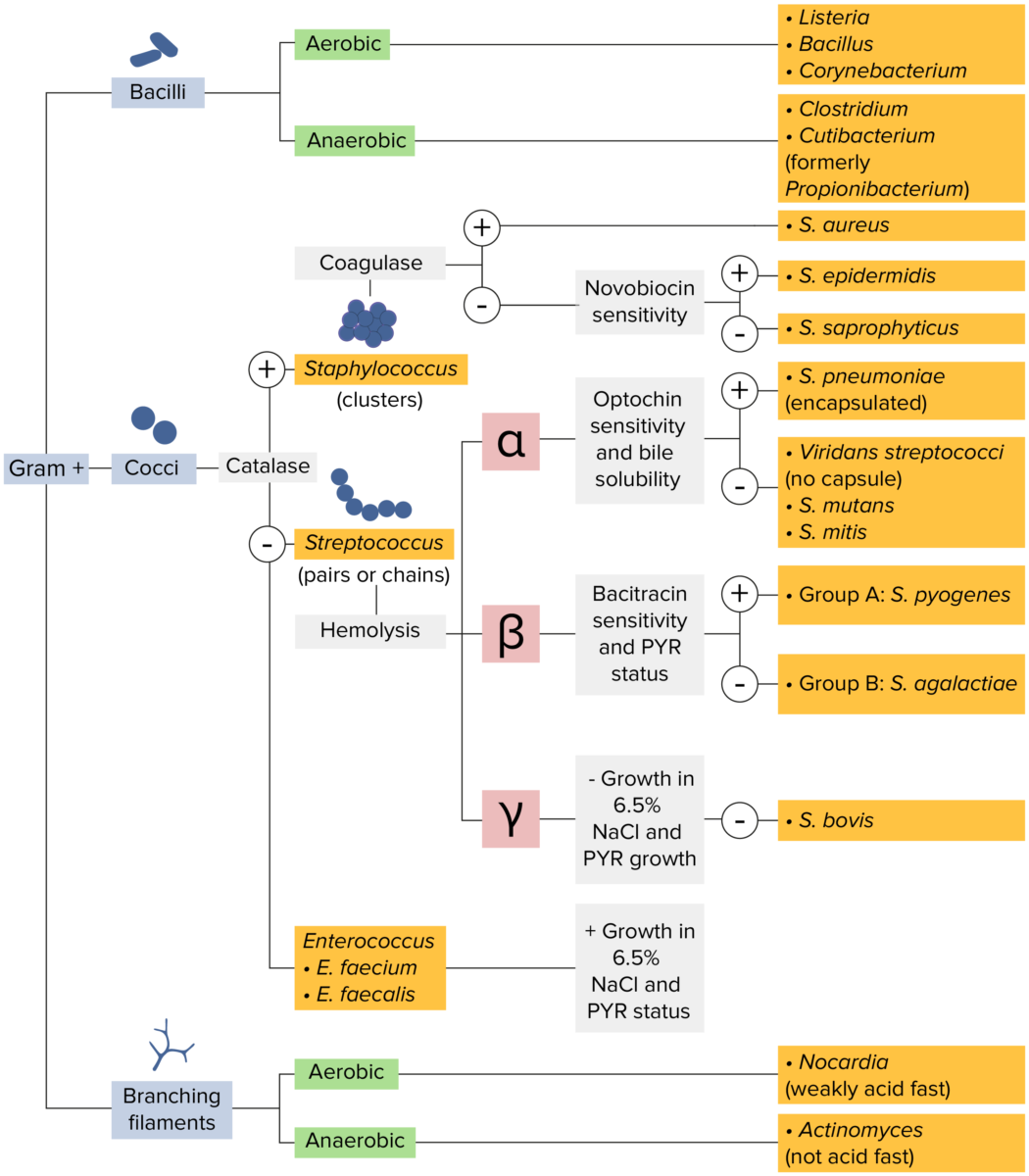
Gram-positive bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thick layer of peptidoglycan retain the crystal violet stain utilized in Gram staining but are not affected by the safranin counterstain. These bacteria appear as purple-blue on the stain, indicating that they are gram positive. The bacteria can be further classified according to morphology (branching filaments, bacilli, and cocci in clusters or chains) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The cocci can also be further identified. Staphylococci can be narrowed down on the basis of the presence of the enzyme coagulase and on their sensitivity to the antibiotic novobiocin. Streptococci are grown on blood agar and classified on the basis of which form of hemolysis they employ (α, β, or γ). Streptococci are further narrowed on the basis of their response to the pyrrolidonyl-β-naphthylamide (PYR) test, their sensitivity to specific antimicrobials (optochin and bacitracin), and their ability to grow on sodium chloride (NaCl) media.
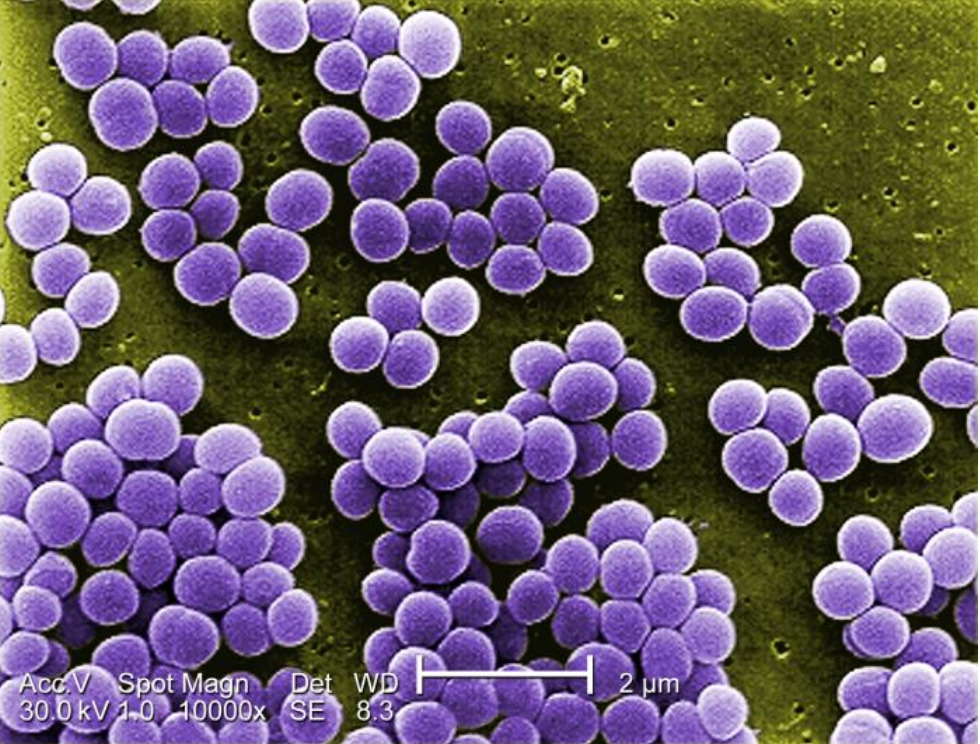
Digitally-colorized scanning electron microscopic image under 10,000X magnification of Staphylococcus aureus:
Notice these cocci resemble a “cluster of grapes.”
The clinically relevant species can be classified based on the presence (or absence) of coagulase:
| Species | Coagulase | Blood agar Blood agar Nocardia/Nocardiosis | Mannitol Mannitol A diuretic and renal diagnostic aid related to sorbitol. It has little significant energy value as it is largely eliminated from the body before any metabolism can take place. It can be used to treat oliguria associated with kidney failure or other manifestations of inadequate renal function and has been used for determination of glomerular filtration rate. Mannitol is also commonly used as a research tool in cell biological studies, usually to control osmolarity. Osmotic Diuretics salt agar | Novobiocin* sensitivity |
|---|---|---|---|---|
| S. aureus | Positive | Beta-hemolysis | Yellow colonies | Sensitive |
| S. epidermidis | Negative | Nonhemolytic | Pink or red colonies | Sensitive |
| S. saprophyticus | Negative | Nonhemolytic | Yellow or red colonies (depending on the strain) | Resistant |

Methicillin-resistant Staphylococcus aureus (MRSA):
Coagulase-positive S. aureus ferments mannitol (red), producing yellow colonies on mannitol salt agar plates.
Staphylococcus species are part of the normal human flora:
Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess can be transmitted via aerosols Aerosols Colloids with a gaseous dispersing phase and either liquid (fog) or solid (smoke) dispersed phase; used in fumigation or in inhalation therapy; may contain propellant agents. Coxiella/Q Fever and contact with:
Risk factors for severe Staphylococcus infection include:
Common to most staphylococci:
Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess:
CoNS:
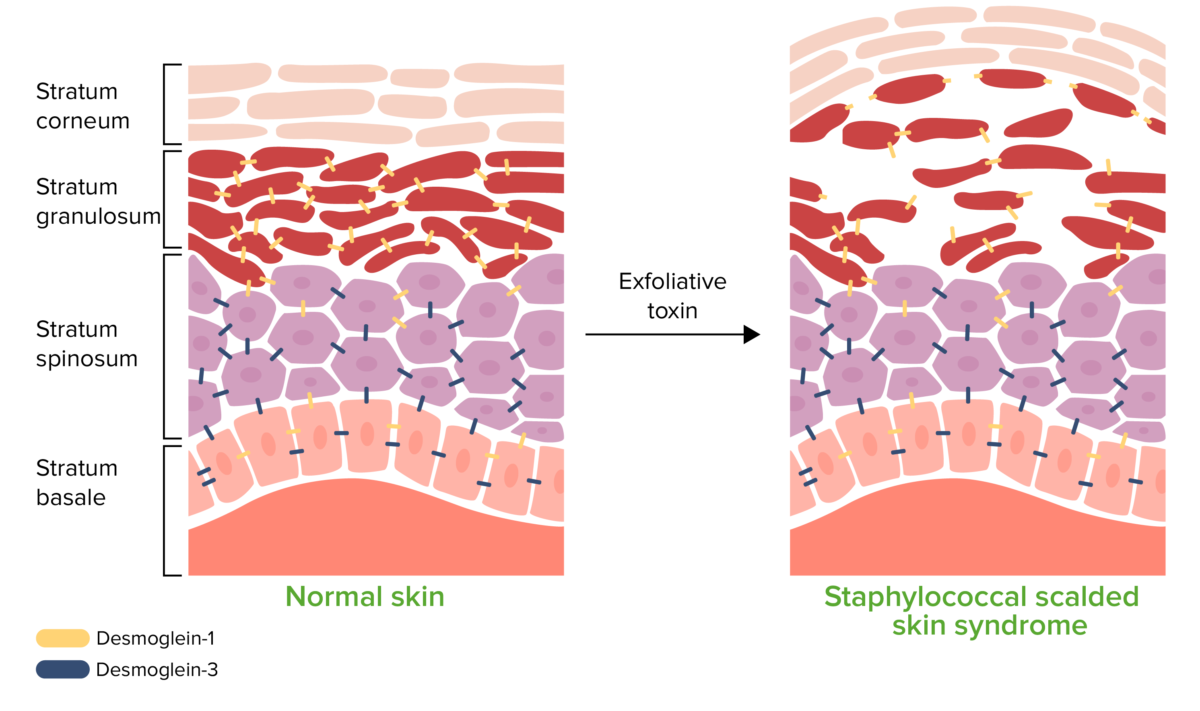
Pathophysiology of staphylococcal scalded skin syndrome:
Exfoliative toxin cleaves desmoglein (Dsg) 1, disrupting the cell-to-cell adhesion of the stratum granulosum. This detachment of the superficial epidermis causes bullae formation and desquamation.
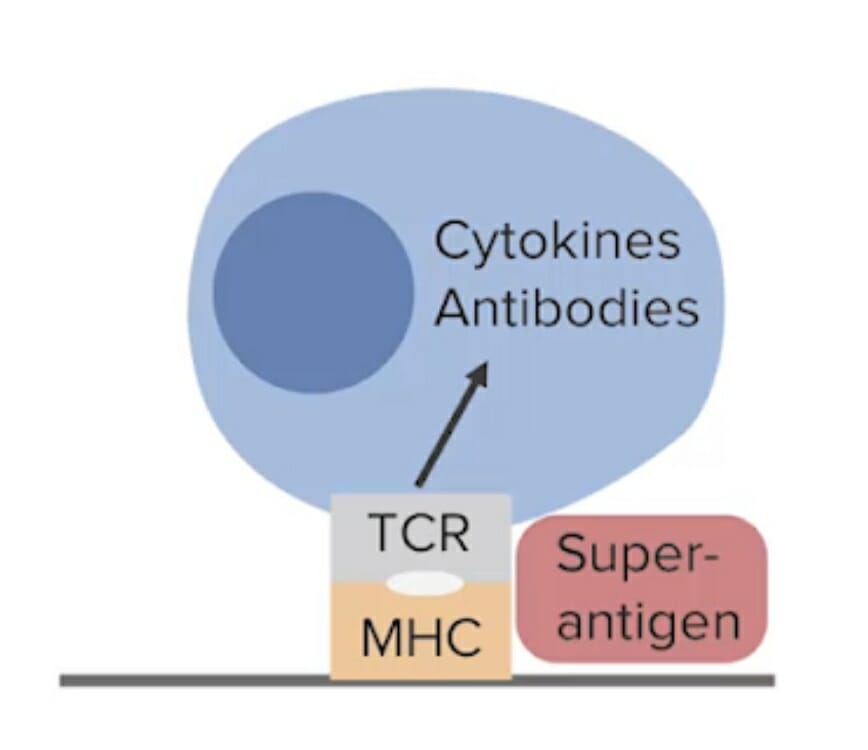
Superantigens bind to major histocompatibility complex (MHC) class II T cell receptors (TCR), which stimulate an exaggerated cytokine release and inflammatory response. This includes toxic shock syndrome toxin type-1, which can be produced by Staphylococcus aureus.
Image by Lecturio.Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess can cause a wide range of infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, including (but not limited to):

Crusted, nonbullous impetigo on the upper extremity of a pediatric patient
Image: “Diagnosis of Atopic Dermatitis: Mimics, Overlaps, and Complications” by Siegfried EC, Hebert AA. License: CC BY 4.0
Cutaneous abscess caused by MRSA
Image: “Cutaneous abscess MRSA” by CDC/Bruno Coignard, M.D. License: Public Domain
Lower extremity with areas of necrosis, erythema, and bullous changes, commonly seen in necrotizing fasciitis.
Image: “Necrotizing fasciitis left leg” by Piotr Smuszkiewicz, Iwona Trojanowska and Hanna Tomczak. License: CC BY 2.0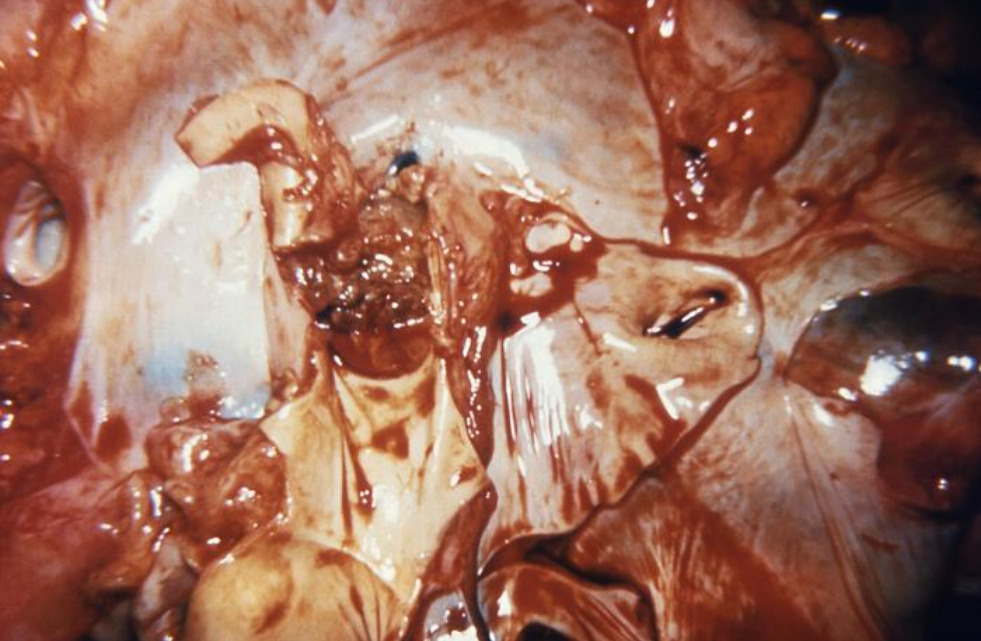
Bacterial endocarditis: obstruction of the pulmonic valve of a heart by a bacterial vegetation, seen here during autopsy
Image: “Bacterial endocarditis” by CDC/ Dr. Sellers. License: Public Domain| Disease | Exotoxin | Clinical presentation |
|---|---|---|
| SSSS SSSS Staphylococcal scalded skin syndrome (SSSS), also known as Ritter disease and staphylococcal epidermal necrolysis, is a toxin-mediated condition caused by Staphylococcus aureus. The exfoliative toxin produced disseminates and cleaves desmoglein 1 in the epidermis, causing separation and detachment of the skin. Staphylococcal Scalded Skin Syndrome (SSSS) | Exfoliative toxins A and B |
|
| Toxic shock syndrome Toxic Shock Syndrome Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing. Toxic Shock Syndrome ( TSS TSS Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing. Toxic Shock Syndrome) |
Toxic shock syndrome
Toxic Shock Syndrome
Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing.
Toxic Shock Syndrome toxin type-1 (
TSST-1
TSST-1
Toxic Shock Syndrome) Enterotoxin Enterotoxin Substances that are toxic to the intestinal tract causing vomiting, diarrhea, etc. ; most common enterotoxins are produced by bacteria. Diarrhea B |
|
| Gastroenteritis Gastroenteritis Gastroenteritis is inflammation of the stomach and intestines, commonly caused by infections from bacteria, viruses, or parasites. Transmission may be foodborne, fecal-oral, or through animal contact. Common clinical features include abdominal pain, diarrhea, vomiting, fever, and dehydration. Gastroenteritis | Enterotoxins |
|

Staphylococcal scalded skin syndrome in a newborn:
This image shows diffuse erythema, bullae formation, and skin peeling.

Morbilliform rash from toxic shock syndrome (TSS)
Image: “Morbilliform rash (resembling measles) resulting from toxic shock syndrome” by Centers for Disease Control and Prevention. License: Public DomainCoagulase-negative staphylococci can cause many of the same conditions as S. aureus. Notable infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease include:
Staphylococcus species can develop antibiotic resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing, and identification Identification Defense Mechanisms of susceptibility is necessary for adequate treatment. Species are often designated as:

Penicillin-binding protein (PBP) forms cross-linked bridges between adjacent peptidoglycan chains during bacterial cell wall synthesis. A beta-lactam antibiotic irreversibly binds to and inhibits the PBP, preventing it from forming new cross-links. This effectively inhibits further cell wall synthesis, which ultimately leads to cell death. Alterations in PBP are what confer staphylococcal resistance to penicillin antibiotics, such as methicillin.
Image by Lecturio. License: CC BY-NC-SA 4.0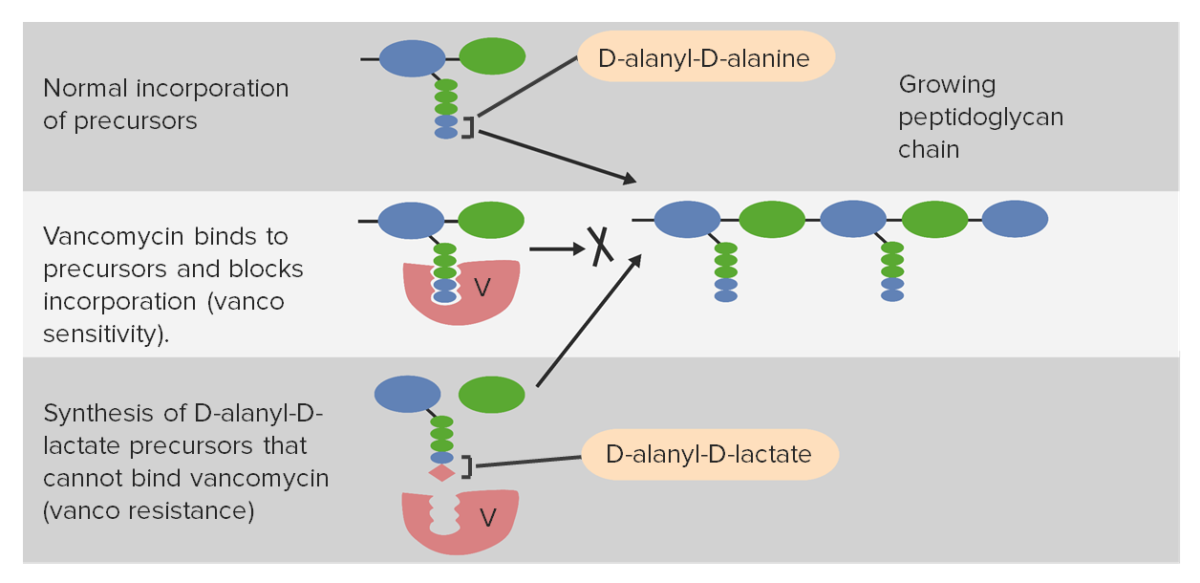
Vancomycin resistance:
Synthesis of D-alanyl-D-lactate on peptidoglycan precursors in the cell wall causes poor binding with vancomycin, thus reducing the effectiveness of the antibiotic.
The agent of choice and duration of treatment for Staphylococcus infection depends on the body area affected, the severity of infection, and the antibiotic sensitivity of the strain.
| Strain | Antibiotic |
|---|---|
| MSSA and CoNS |
|
| MRSA |
|
| VRSA |
|