Clostridia species comprise a group of spore-forming, obligate anaerobic, gram-positive Gram-Positive Penicillins bacilli Bacilli Shigella. Major pathogenic species include Clostridium perfringens Clostridium perfringens The most common etiologic agent of gas gangrene. It is differentiable into several distinct types based on the distribution of twelve different toxins. Gas Gangrene ( C. perfringens C. perfringens The most common etiologic agent of gas gangrene. It is differentiable into several distinct types based on the distribution of twelve different toxins. Gas Gangrene), which is associated with gas gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction; Clostridioides difficile, which is associated with pseudomembranous colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis; C. tetani, which causes tetanus Tetanus Tetanus is a bacterial infection caused by Clostridium tetani, a gram-positive obligate anaerobic bacterium commonly found in soil that enters the body through a contaminated wound. C. tetani produces a neurotoxin that blocks the release of inhibitory neurotransmitters and causes prolonged tonic muscle contractions. Tetanus; and C. botulinum, which causes botulism Botulism Botulism is a rare, neuroparalytic syndrome caused by Clostridium botulinum (C. botulinum). A fatal neurotoxin (botulinum toxin) is released causing varying degrees of muscle paralysis and distinct clinical syndromes. The most common types of botulism are foodborne and infant. Botulism. Clostridium perfringens Clostridium perfringens The most common etiologic agent of gas gangrene. It is differentiable into several distinct types based on the distribution of twelve different toxins. Gas Gangrene ( C. perfringens C. perfringens The most common etiologic agent of gas gangrene. It is differentiable into several distinct types based on the distribution of twelve different toxins. Gas Gangrene), Clostridioides difficile, C. tetani, and C. botulinum have broad-spectrum Broad-Spectrum Fluoroquinolones invasiveness and clinical manifestations that are summarized below. Note that Clostridium difficile has been reclassified as Clostridioides difficile. However, exams will likely not have the updated genus for several years.
Last updated: Jan 16, 2024
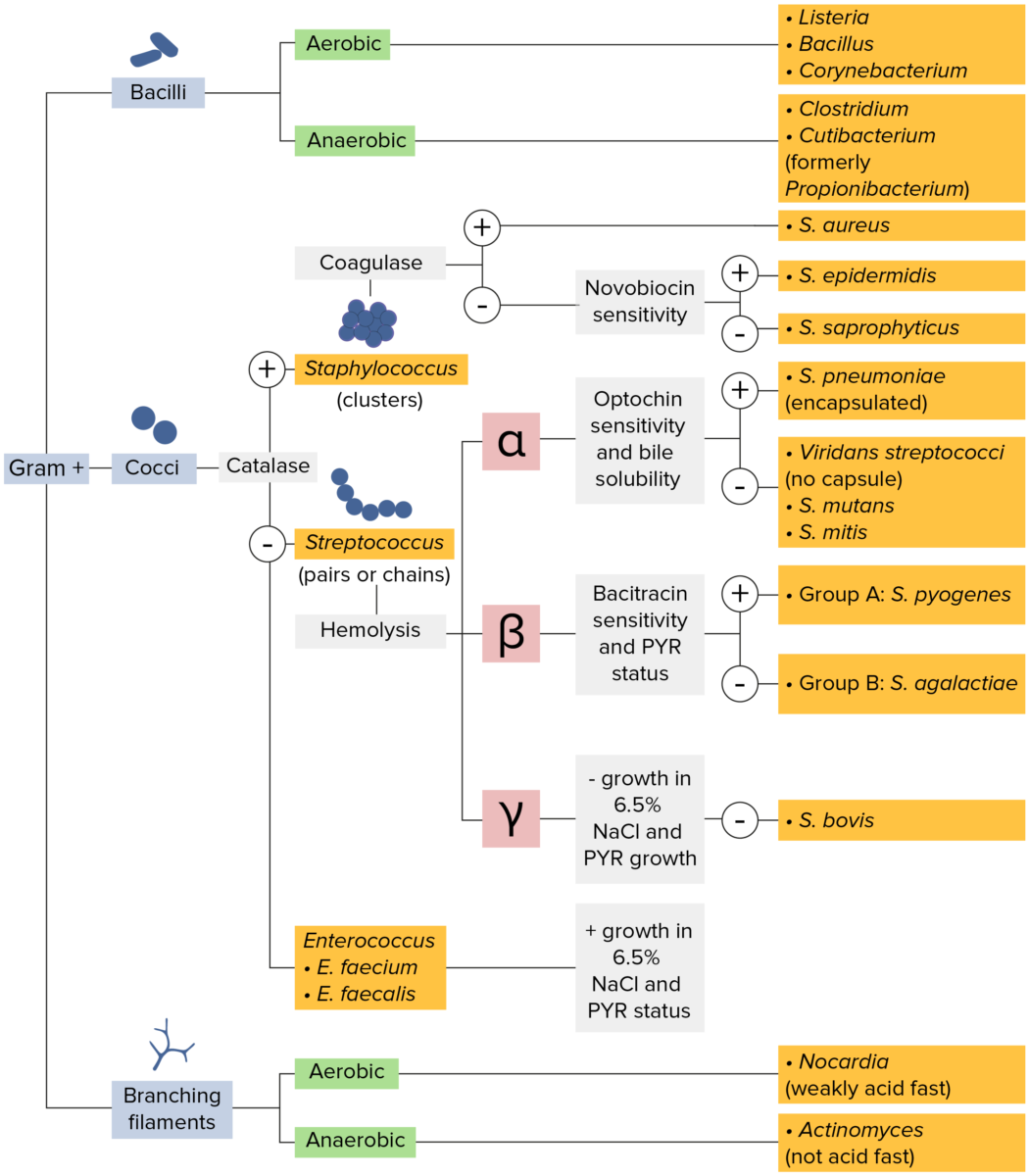
Gram-positive bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thick layer of peptidoglycan retain the crystal violet stain utilized in Gram staining but are not affected by the safranin counterstain. These bacteria appear as purple-blue on the stain, indicating that they are gram positive. The bacteria can be further classified according to morphology (branching filaments, bacilli, and cocci in clusters or chains) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The cocci can also be further identified. Staphylococci can be narrowed down on the basis of the presence of the enzyme coagulase and on their sensitivity to the antibiotic novobiocin. Streptococci are grown on blood agar and classified on the basis of which form of hemolysis they employ (α, β, or γ). Streptococci are further narrowed on the basis of their response to the pyrrolidonyl-β-naphthylamide (PYR) test, their sensitivity to specific antimicrobials (optochin and bacitracin), and their ability to grow on sodium chloride (NaCl) media.
A cartoon showing the general structure of the gram-positive Clostridia bacteria
Image by Lecturio.| C. botulinum | Clostridioides difficile | C. perfringens C. perfringens The most common etiologic agent of gas gangrene. It is differentiable into several distinct types based on the distribution of twelve different toxins. Gas Gangrene | C. tetani | |
|---|---|---|---|---|
| Habitat |
|
|
|
|
| Virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus |
|
|
|
|
| Transmission | Ingestion of: | Via
spores
Spores
The reproductive elements of lower organisms, such as bacteria; fungi; and cryptogamic plants.
Anthrax:
|
Via
spores
Spores
The reproductive elements of lower organisms, such as bacteria; fungi; and cryptogamic plants.
Anthrax:
|
Via
spores
Spores
The reproductive elements of lower organisms, such as bacteria; fungi; and cryptogamic plants.
Anthrax:
|
| Clinical presentation |
|
|
|
|

Pathophysiological mechanism caused by Clostridium botulinum
Introducing the pathogen with its toxin causes hyperexcitation since part of the toxin blocks the motor end-plate from releasing its neurotransmitters into the synapse
Adults:
Infants ( floppy baby syndrome Floppy Baby Syndrome Botulism):

Six-week-old infant with botulism
Marked loss of muscle tone, especially in the region of the head and neck
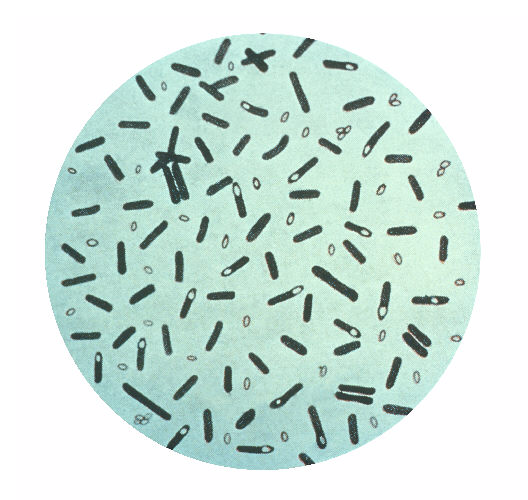
A photomicrograph of Clostridium botulinum bacteria
Image: “Clostridium botulinum” by the CDC. License: Public domain.Pseudomembranous colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis:

Pathologic specimen showing pseudomembranous colitis
Image: “Pseudomembranous colitis” by the pathologist at work. License: Public domain.Myonecrosis (gas gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction):
Food poisoning:

Gas gangrene of the right leg and pelvis
Image: “Gas gangrene” by Engelbert Schröpfer, Stephan Rauthe, and Thomas Meyer. License: CC BY 2.0.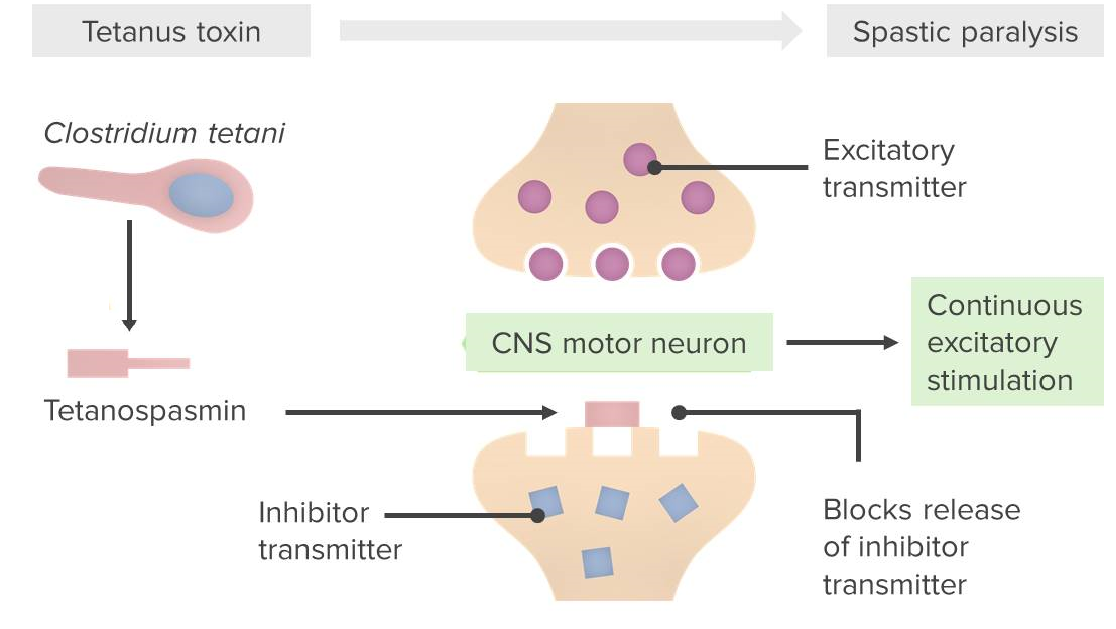
Pathophysiological mechanism caused by Clostridium tetani
Tetanospasmin blocks the binding of neurotransmitters (GABA/glycine) to their receptors on the postsynaptic membrane; thus, inhibitory neurotransmission

Risus sardonicus in a patient with generalized tetanus
Image: “PMC4946959_cureus-0008-000000000644-i01” by Zunga PM, Tarfarosh SF, Farooq O, Dar IH, Rashid S, & Yaseen U. License: CC BY 3.0.