Gas gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction, also known as clostridial myonecrosis Myonecrosis A severe condition resulting from bacteria invading healthy muscle from adjacent traumatized muscle or soft tissue. The infection originates in a wound contaminated with bacteria of the genus Clostridium. C. perfringens accounts for the majority of cases (over eighty percent), while C. novyi, C. septicum, and C. histolyticum cause most of the other cases. Clostridia, is a life-threatening muscle and soft tissue Soft Tissue Soft Tissue Abscess infection that usually develops after traumatic inoculation with Clostridium perfringens (C. perfringens), but can also develop spontaneously in association with other Clostridium species. Sudden, severe muscle pain Muscle Pain Ion Channel Myopathy classically develops shortly after the injury. Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions color changes (red/purple to black), tenderness, bullae Bullae Erythema Multiforme formation, and crepitus Crepitus Osteoarthritis are also present and progress rapidly. Most of the time, diagnosis is established clinically. Once the diagnosis is suspected, intravenous (IV) antibiotic therapy should be started and emergent surgical debridement Debridement The removal of foreign material and devitalized or contaminated tissue from or adjacent to a traumatic or infected lesion until surrounding healthy tissue is exposed. Stevens-Johnson Syndrome should be performed.
Last updated: Feb 14, 2023
Gas gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction (clostridial myonecrosis Myonecrosis A severe condition resulting from bacteria invading healthy muscle from adjacent traumatized muscle or soft tissue. The infection originates in a wound contaminated with bacteria of the genus Clostridium. C. perfringens accounts for the majority of cases (over eighty percent), while C. novyi, C. septicum, and C. histolyticum cause most of the other cases. Clostridia) is a rapidly progressing infection of muscle and soft tissue Soft Tissue Soft Tissue Abscess most commonly caused by Clostridium species.
Localized signs and symptoms:

Gas gangrene:
Erythema of the right shoulder with an area of necrosis can be seen.

Gas gangrene of the right leg and pelvis, showing swelling and discoloration of the right thigh, bullae, and palpable crepitus:
The patient, in shock at the time this photograph was taken, underwent a hemipelvectomy and died less than 8 hours later.
Systemic symptoms:
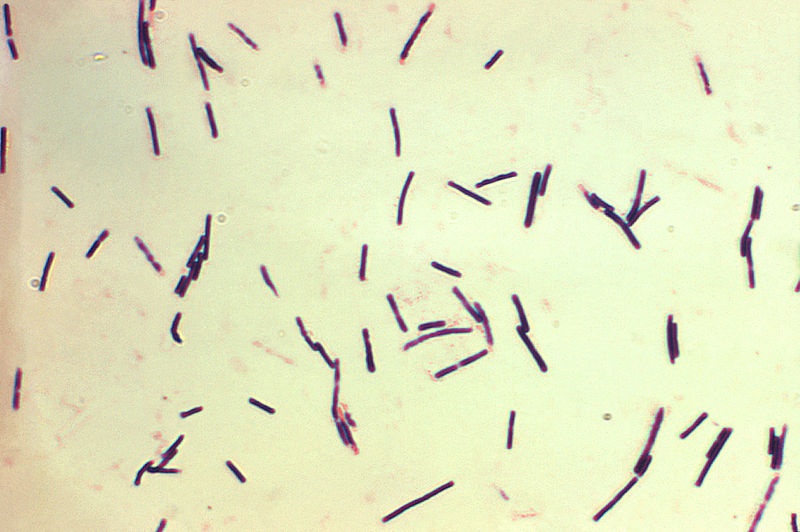
A photomicrograph showing gram-positive bacilli representing C. perfringens
Image: “Clostridium perfringens” by CDC/Don Stalons. License: Public Domain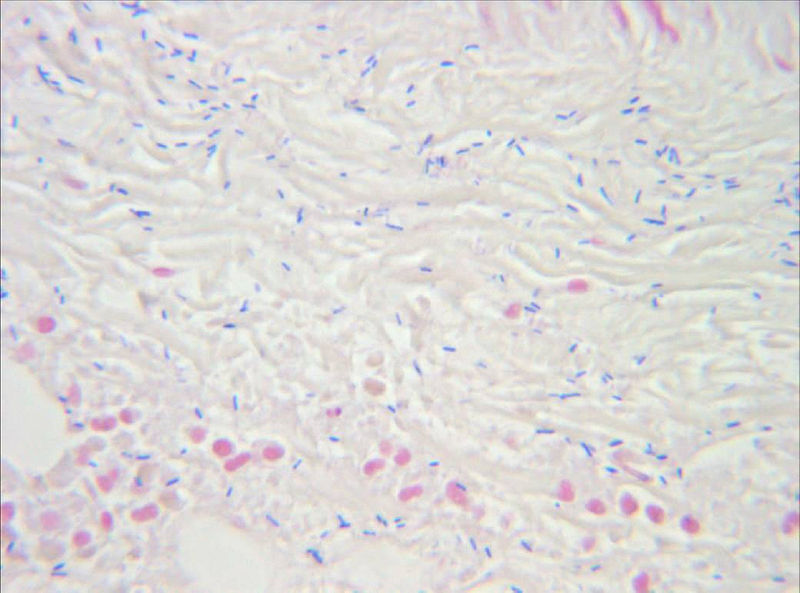
Identification of gram-positive, rod-shaped, anaerobic, spore-forming bacteria (C. perfringens) in the infected muscle tissue (gas gangrene)
Image: “Clostridium perfringens” by Engelbert Schröpfer, Stephan Rauthe and Thomas Meyer. License: CC BY 2.0
X-ray reveals soft-tissue gas consistent with gas gangrene.
Image: “Figure 3” by Cooney and Cooney. License: CC BY 2.0