A pyogenic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease is a polymicrobial infection arising from contiguous or hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases spread. Pyogenic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease is the most common type of visceral abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may present with a triad of fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, malaise Malaise Tick-borne Encephalitis Virus, and RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Laboratory analysis can be informative with elevated WBC and abnormal liver function tests Liver function tests Liver function tests, also known as hepatic function panels, are one of the most commonly performed screening blood tests. Such tests are also used to detect, evaluate, and monitor acute and chronic liver diseases. Liver Function Tests, and imaging may reveal solitary or multiple lesions on ultrasound or CT scan. On contrast imaging, the lesions generally appear well-defined with rim enhancement. Diagnosis requires aspiration with Gram stain Gram stain Klebsiella and culture and, in some cases, a drainage catheter may be placed. A combination of drainage and IV antibiotic therapy is the primary method of treatment. Surgical drainage or resection is utilized in specific cases.
Last updated: Jun 29, 2023
Types of liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy abscesses:
Risk factors:
The right lobe is the most common site of infection because of its larger size and blood supply. Multiple pathways exist to infect the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy with bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology:
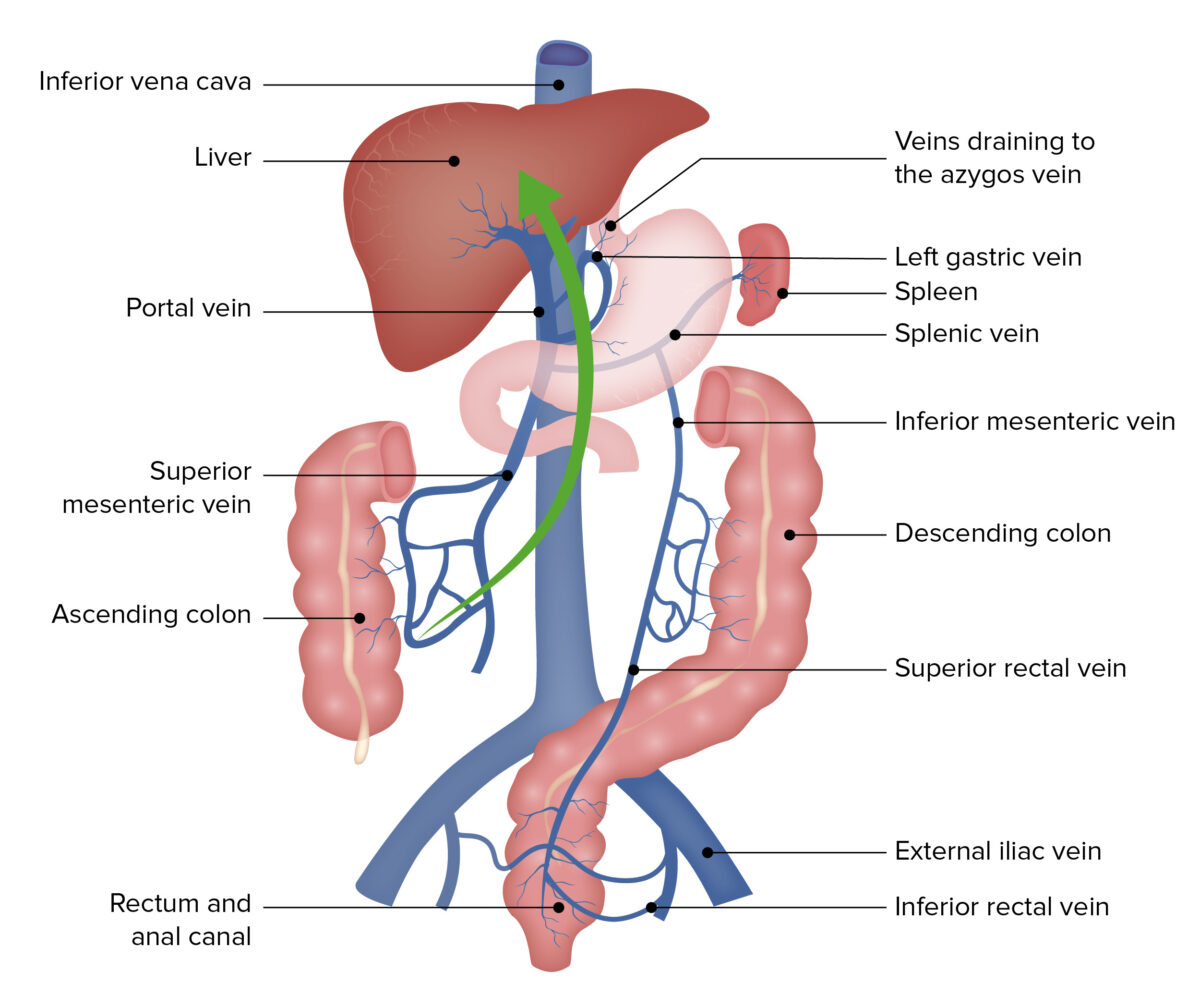
Portal circulation is the primary route: seeding of the liver with bacteria, causing a pyogenic liver abscess.
Image by Lecturio.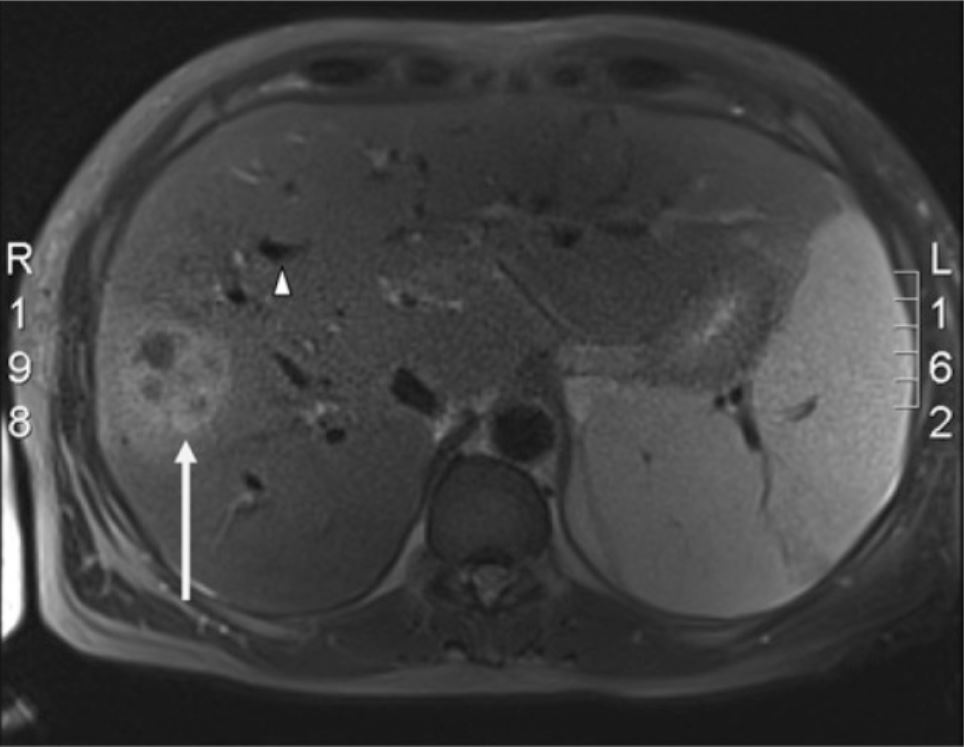
Liver MRCP:
The space-occupying lesion (white arrow) is consistent with a pyogenic liver abscess and seen in the right lobe of the liver. Multiple dilated intrahepatic biliary ducts (white arrowhead) are also present.
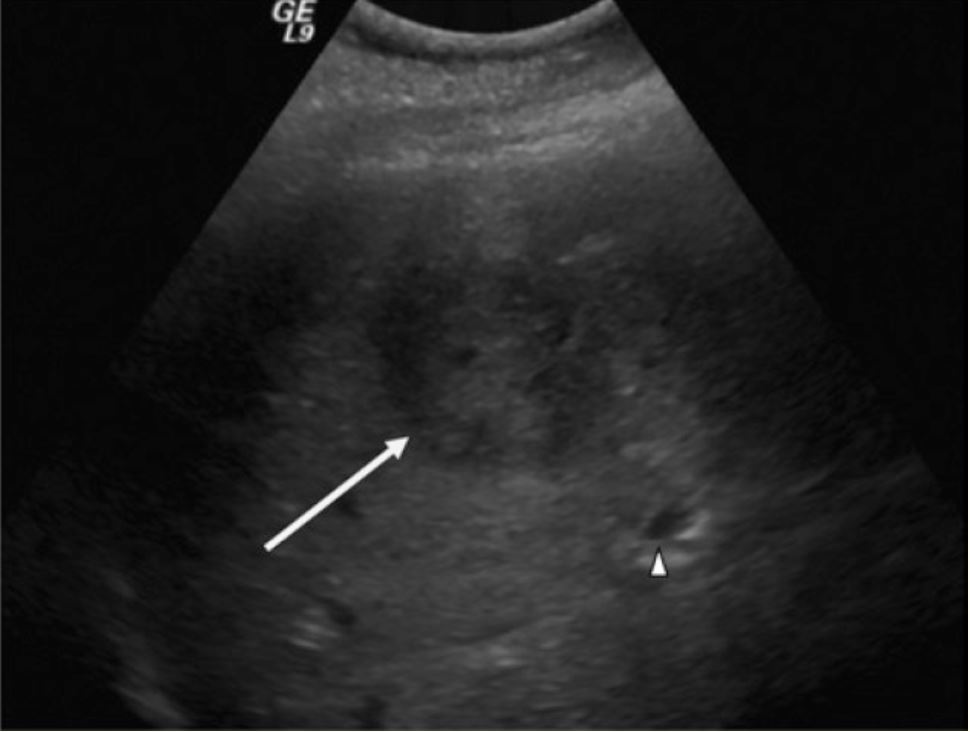
Ultrasound of a suspicious liver mass:
RUQ ultrasound demonstrating a hypodense, well-circumscribed area (arrow) and adjacent dilated intrahepatic biliary duct (arrowhead)
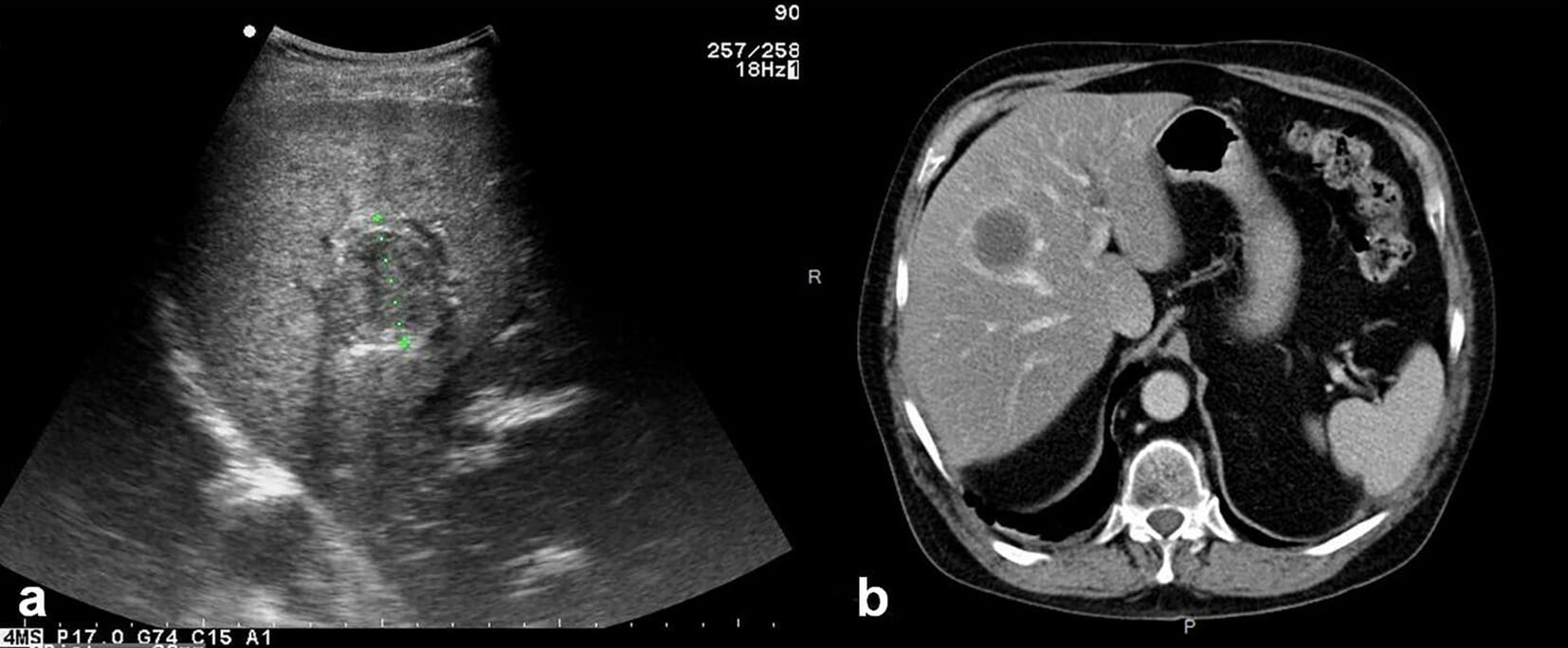
a: ultrasound showing an abscess in the liver b: axial unenhanced CT showing a typical pyogenic liver abscess
Image: “Parasite140075-fig3 Hepatic alveolar echinococcosis imaging” by Liu W, Delabrousse É et al. License: CC BY 4.0Initial broad-spectrum Broad-Spectrum Fluoroquinolones IV antibiotics
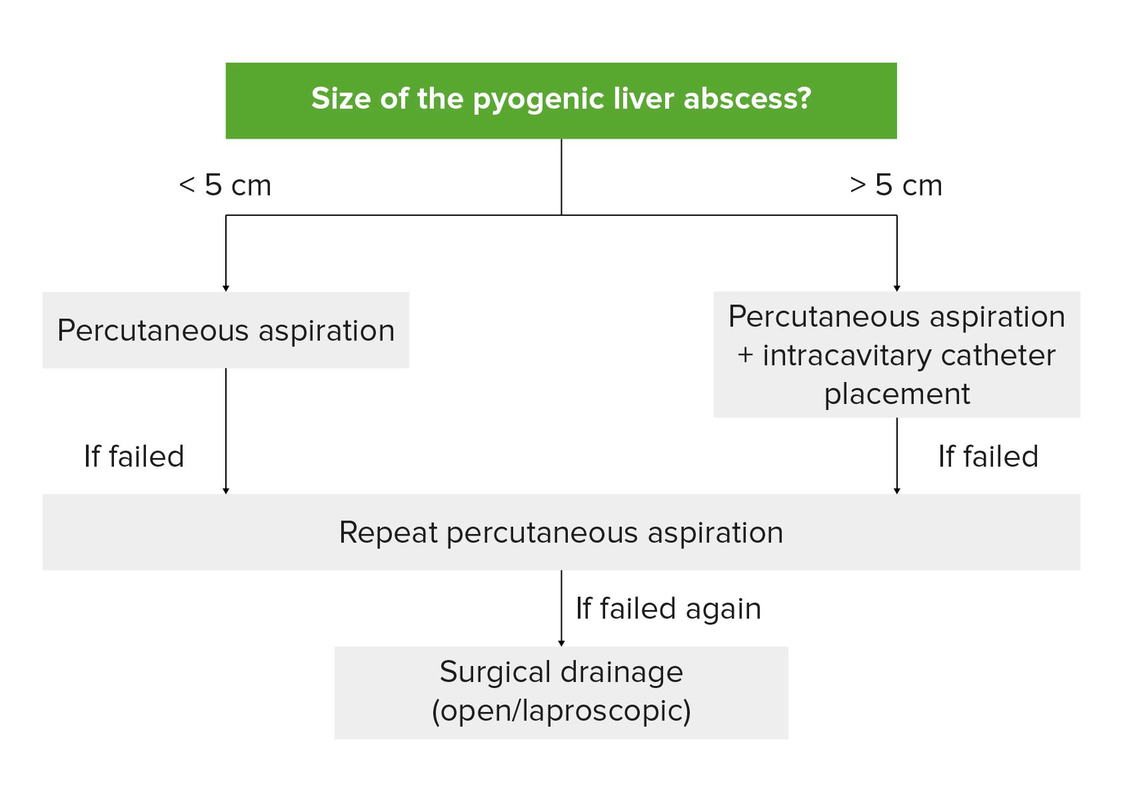
Drainage of unilocular pyogenic abscess:
With abscess ≤ 5 cm, percutaneous drainage is recommended (needle aspiration or catheter placement). Repeated needle aspiration attempts may be necessary. Drainage catheters remain in place until there is minimal drainage. For an abscess > 5 cm, percutaneous aspiration with catheter placement is recommended. Surgical drainage is done when repeated percutaneous drainage fails.
| Amebic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease | Pyogenic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease | Echinococcal cyst | |
|---|---|---|---|
| Number | Single | Single/multiple | Single/multiple |
| Associated symptoms | Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea | RUQ pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | Perianal pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema) |
| Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever | +/- | + | – |
| Imaging (CT) | Solitary lesion in the right lobe of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy | Peripheral rim enhancement is seen with IV contrast administration | Peripheral enhancement even without IV contrast administration (due to eggshell calcification) along with internal septations |
| CBC | ↑ Lymphocytes Lymphocytes Lymphocytes are heterogeneous WBCs involved in immune response. Lymphocytes develop from the bone marrow, starting from hematopoietic stem cells (HSCs) and progressing to common lymphoid progenitors (CLPs). B and T lymphocytes and natural killer (NK) cells arise from the lineage. Lymphocytes: Histology | ↑ Neutrophils Neutrophils Granular leukocytes having a nucleus with three to five lobes connected by slender threads of chromatin, and cytoplasm containing fine inconspicuous granules and stainable by neutral dyes. Innate Immunity: Phagocytes and Antigen Presentation | ↑ Eosinophils Eosinophils Granular leukocytes with a nucleus that usually has two lobes connected by a slender thread of chromatin, and cytoplasm containing coarse, round granules that are uniform in size and stainable by eosin. Innate Immunity: Phagocytes and Antigen Presentation |
| Diagnosis | Amebic serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus | Imaging + aspiration | Imaging + serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus |
| Management |
|
IV antibiotics and surgical/ percutaneous drainage Percutaneous Drainage Echinococcus/Echinococcosis of the abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease | Dependent on classification (surgical resection, albendazole Albendazole A benzimidazole broad-spectrum anthelmintic structurally related to mebendazole that is effective against many diseases. Anthelmintic Drugs, percutaneous treatment) |
| Hepatic hemangioma Hemangioma A vascular anomaly due to proliferation of blood vessels that forms a tumor-like mass. The common types involve capillaries and veins. It can occur anywhere in the body but is most frequently noticed in the skin and subcutaneous tissue. Imaging of the Liver and Biliary Tract | Focal nodular hyperplasia Focal nodular hyperplasia Solitary or multiple benign hepatic vascular tumors, usually occurring in women of 20-50 years of age. The nodule, poorly encapsulated, consists of a central stellate fibrous scar and normal liver elements such as hepatocytes, small bile ducts, and kupffer cells among the intervening fibrous septa. The pale colored central scar represents large blood vessels with hyperplastic fibromuscular layer and narrowing lumen. Benign Liver Tumors | Hepatocellular adenoma Hepatocellular adenoma A benign epithelial tumor of the liver. Benign Liver Tumors | |
|---|---|---|---|
| Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma | Cavernous vascular spaces lined by flat endothelial cells | Localized hepatocyte nodules with large malformed arterial branches and centralized fibrous Fibrous Fibrocystic Change tissue | Enlarged hepatocytes Hepatocytes The main structural component of the liver. They are specialized epithelial cells that are organized into interconnected plates called lobules. Liver: Anatomy with small and regular Regular Insulin nuclei (no anaplasia); normal hepatic lobular architecture is absent |
| CT scan findings | Well-demarcated, hypodense mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast with peripheral enhancement on arterial phase and centripetal filling on delayed phases | Central stellate scar Scar Dermatologic Examination | Well-demarcated mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast with heterogeneous enhancement Heterogeneous Enhancement Imaging of the Spleen on arterial phase and isodense on venous phase (without washout of contrast) |
| Simple cyst Simple Cyst Imaging of the Breast | Polycystic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease | Choledochal cyst | Cystadenoma/cystadenocarcinoma | |
|---|---|---|---|---|
| Description | Most common hepatic cyst, contains clear fluid, lacks communication Communication The exchange or transmission of ideas, attitudes, or beliefs between individuals or groups. Decision-making Capacity and Legal Competence with the intrahepatic biliary tree Biliary tree The bile ducts and the gallbladder. Gallbladder and Biliary Tract: Anatomy | Several cysts Cysts Any fluid-filled closed cavity or sac that is lined by an epithelium. Cysts can be of normal, abnormal, non-neoplastic, or neoplastic tissues. Fibrocystic Change replace large portion of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy | Congenital Congenital Chorioretinitis malformations of the pancreaticobiliary tree, multiple types based on location in biliary system |
|
| Clinical Presentation | Usually asymptomatic |
|
|
|
| Diagnosis |
|
Ultrasound: replacement of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy parenchyma by cysts Cysts Any fluid-filled closed cavity or sac that is lined by an epithelium. Cysts can be of normal, abnormal, non-neoplastic, or neoplastic tissues. Fibrocystic Change of varying sizes | Ultrasound, CT, transhepatic cholangiography, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy function test |
|
| Management | Treat with excision (only if symptomatic) | Partial liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy resection or, in rare cases, transplantation (only if symptomatic) |
|
All complex, multiloculated cysts Cysts Any fluid-filled closed cavity or sac that is lined by an epithelium. Cysts can be of normal, abnormal, non-neoplastic, or neoplastic tissues. Fibrocystic Change (except chinococcal) should be excised because of the risk of malignancy Malignancy Hemothorax. |