The hepatobiliary system is composed of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy, and bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy ducts (within the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and external to the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy). The liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy produces bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy, which is a fluid made of cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism, phospholipids Phospholipids Lipids containing one or more phosphate groups, particularly those derived from either glycerol (phosphoglycerides) or sphingosine (sphingolipids). They are polar lipids that are of great importance for the structure and function of cell membranes and are the most abundant of membrane lipids, although not stored in large amounts in the system. Lipid Metabolism, conjugated bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism, bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy salts, electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes, and water. Bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy, which assists in digestion Digestion Digestion refers to the process of the mechanical and chemical breakdown of food into smaller particles, which can then be absorbed and utilized by the body. Digestion and Absorption and helps eliminate waste products, is stored in the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy. The hepatobiliary system can be affected by infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, cysts Cysts Any fluid-filled closed cavity or sac that is lined by an epithelium. Cysts can be of normal, abnormal, non-neoplastic, or neoplastic tissues. Fibrocystic Change, solid masses, ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, and mechanical flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure obstruction, which mandate the presence of reliable imaging tests to determine the etiology. The methods that evaluate structural changes in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and biliary tract Biliary tract Bile is secreted by hepatocytes into thin channels called canaliculi. These canaliculi lead into slightly larger interlobular bile ductules, which are part of the portal triads at the "corners" of hepatic lobules. The bile leaves the liver via the right and left hepatic ducts, which join together to form the common hepatic duct. Gallbladder and Biliary Tract: Anatomy include ultrasonography, CT scan, and MRI (including magnetic resonance cholangiopancreatography Magnetic resonance cholangiopancreatography Non-invasive diagnostic technique for visualizing the pancreatic ducts and bile ducts without the use of injected contrast media or x-ray. Mri scans provide excellent sensitivity for duct dilatation, biliary stricture, and intraductal abnormalities. Primary Sclerosing Cholangitis). Additionally, cholescintigraphy Cholescintigraphy Nuclear Imaging, a functional imaging study, helps identify gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy pathology by tracking the biliary pathway.
Last updated: May 17, 2024
Prior to interpretation of any image, the physician should take certain preparatory steps. The same systematic approach should be followed every time.
Report includes:
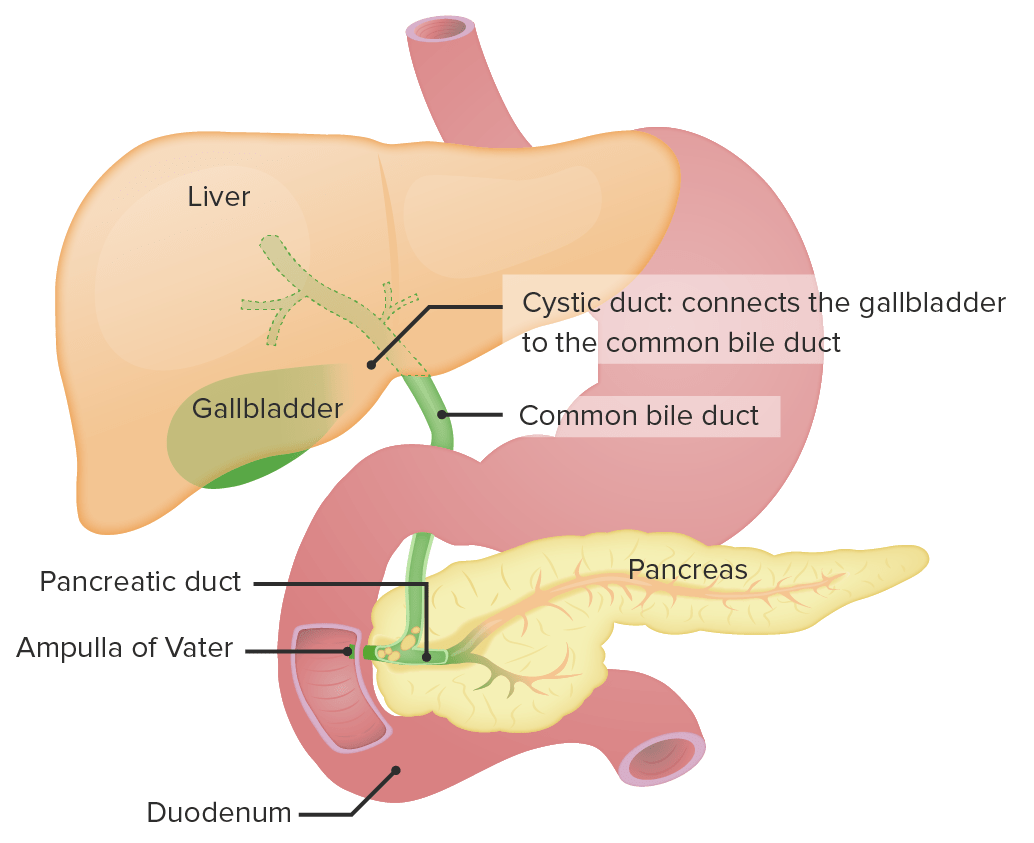
Anatomy of the liver and the biliary system
Image by Lecturio.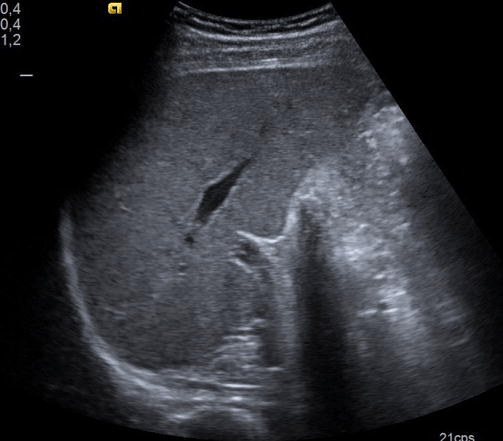
Normal liver ultrasound showing a homogeneous parenchyma
Image: “Normal liver” by Fuster, D. et al. License: CC BY 3.0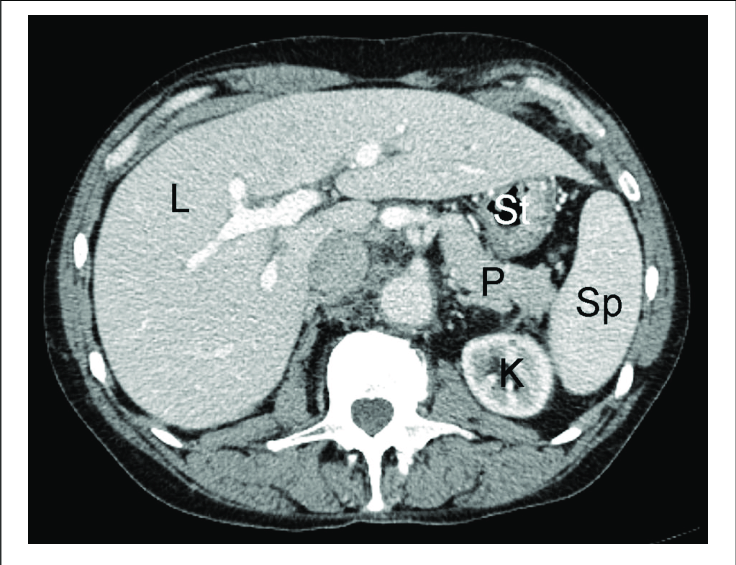
A normal contrast-enhanced CT scan of the liver:
K: kidney
L: liver
P: pancreas
St: stomach
Sp: spleen
| Tissue | T1-weighted images T1-Weighted Images Imaging of the Head and Brain | T2-weighted images T2-Weighted Images Imaging of the Head and Brain |
|---|---|---|
| Fluid (e.g., CSF) | Dark | Bright |
| Fat | Bright | Bright |
| Inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation | Dark | Bright |
Nuclear medicine Nuclear medicine A specialty field of radiology concerned with diagnostic, therapeutic, and investigative use of radioactive compounds. Nuclear Imaging differs from the rest of radiology because it is functional, rather than structural, imaging.
| Imaging finding | What it means |
|---|---|
| Bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy ducts visible | Normal hepatic function |
| Filling of the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy | Patent cystic Cystic Fibrocystic Change duct |
| Radiotracer seen in the duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy | Patent common bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy duct |
| No radiotracer seen in the gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy | Obstructed gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy ( acute cholecystitis Acute cholecystitis Acute inflammation of the gallbladder wall. It is characterized by the presence of abdominal pain; fever; and leukocytosis. Gallstone obstruction of the cystic duct is present in approximately 90% of the cases. Cholecystitis) |
| No radiotracer seen in the duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy | Biliary atresia Atresia Hypoplastic Left Heart Syndrome (HLHS) |
| Radiotracer outside the biliary system | Biliary leak |
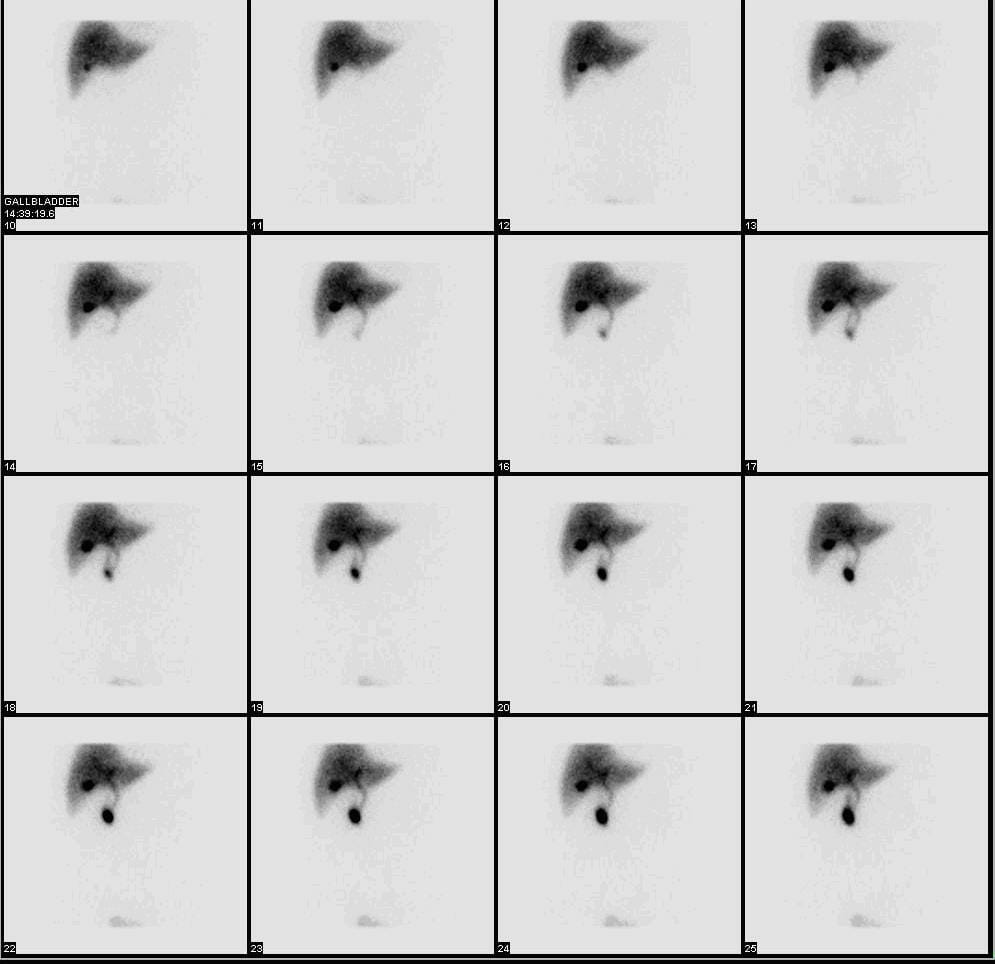
Normal hepatobiliary iminodiacetic acid scan showing the radioactive substance moving through the biliary system
Image: “HIDA” by Myo Han. License: CC BY 3.0
B-mode ultrasound showing hyperechoic liver as compared with the kidney parenchyma and posterior attenuation of the deep liver parenchyma in the context of hepatic steatosis
Image: “Figure 1” by Lăpădat, A.M et al. License: CC BY 3.0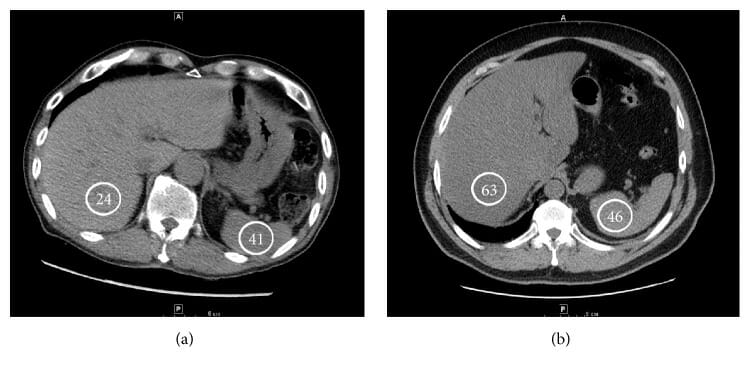
CT images showing an example of a steatotic liver (a) and a normal hepatic attenuation (b):
Hounsfield units are indicated in the circles
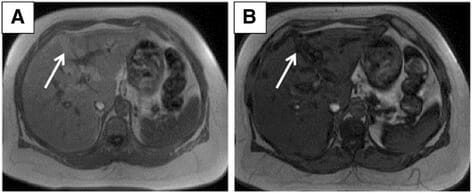
Subcapsular hepatic steatosis:
A: Axial T1-weighted in-phase gradient echo MRI shows areas of hyperintensity in the subcapsular region (arrow).
B: Axial T1-weighted opposed-phase gradient echo MRI shows signal loss in the corresponding subcapsular regions (arrow).

Cholecystitis on ultrasound:
Gallbladder with thickened wall

CT scan showing gallbladder with gallstone
Image: “F1” by Zagouri, F. et al. License: CC BY 2.0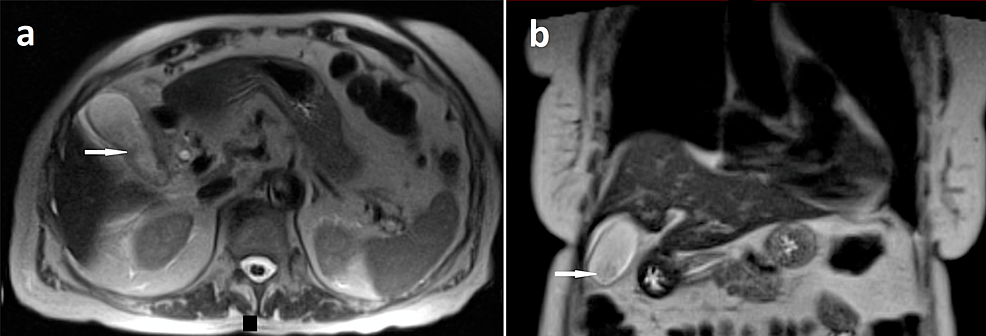
MRI of the abdomen showing cholecystitis:
Axial (a) and coronal (b) sections of T2-weighted contrast-enhanced abdominal MRI showing layering sludge in the gallbladder (white arrows) with gallbladder wall thickening and trace pericholecystic fluid
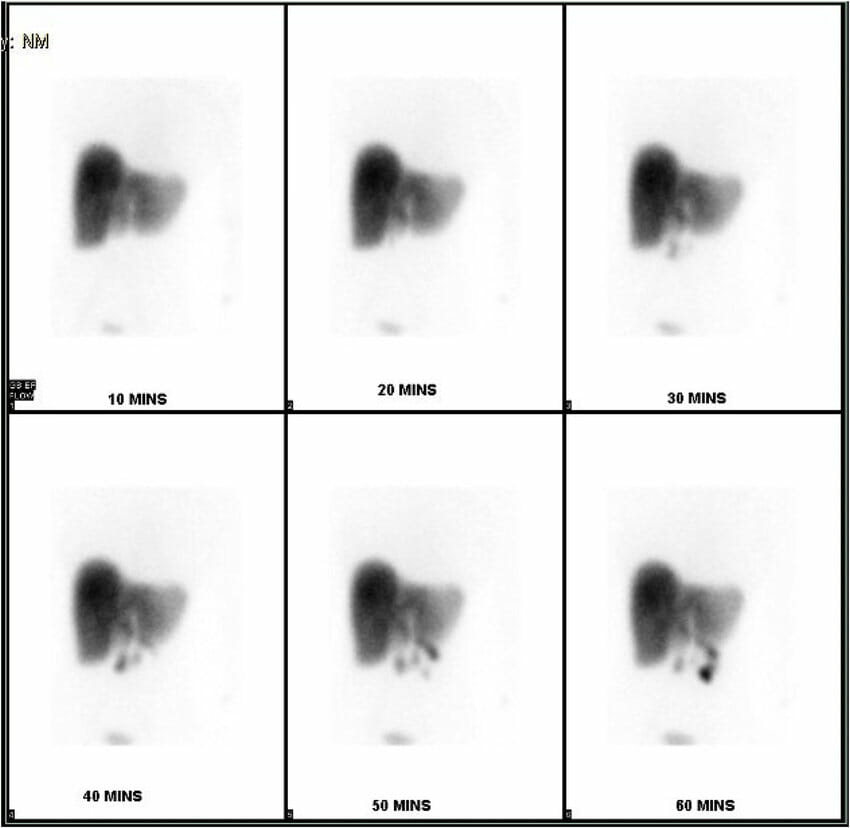
Hepatobiliary iminodiacetic acid scan showing nonaccumulation of the isotope within the gallbladder in a case of acalculous cholecystitis
Image: “HIDA scan showing non-accumulation of the isotope within the gallbladder” by Rezkallah, K. et al. License: CC BY 4.0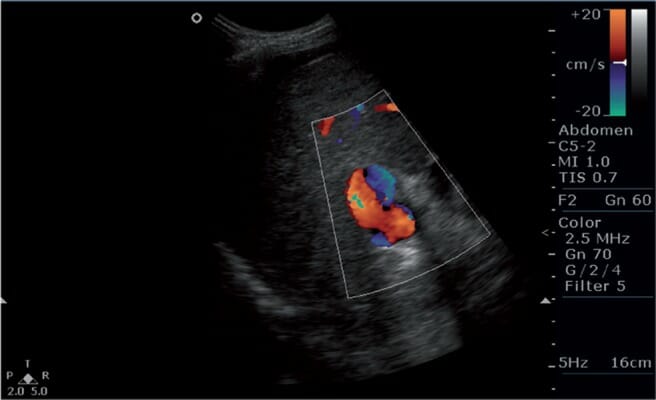
Color Doppler image showing bidirectional flow (or inversion of flow) in the portal vein, a finding suggestive of portal hypertension
Image: “s5fig2” by Mittal, P. et al. License: CC BY 2.5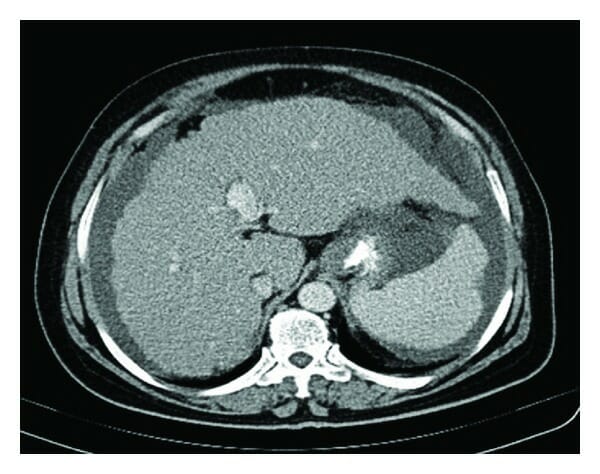
Abdominal CT scan showing a cirrhotic liver, splenomegaly, and ascites
Image: “Figure 1” by Nasrollah, M. et al. License: CC BY 3.0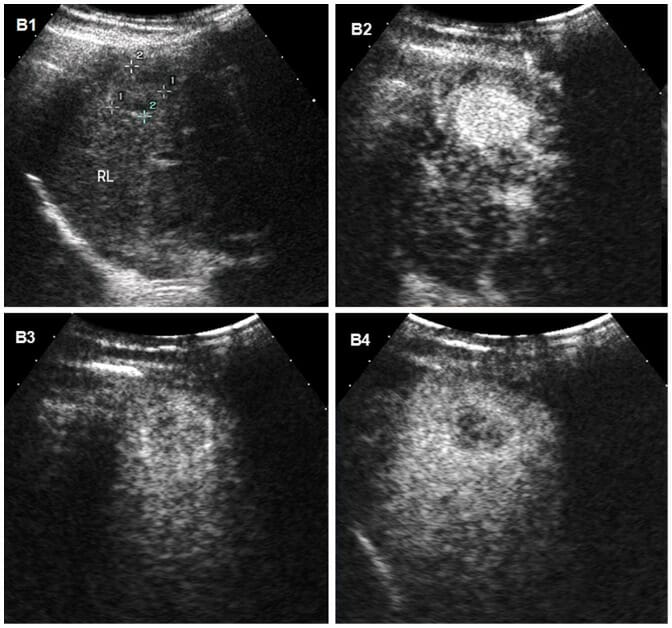
Hepatocellular carcinoma on ultrasound:
Ultrasound images of hepatocellular carcinoma in the liver of a 31-year-old man with cirrhosis.
B1: Conventional ultrasound shows the mass as a poorly-defined hypoechoic nodule.
B2–B4: Contrast-enhanced ultrasound (CEUS) time-sequenced images were obtained after injection of a microbubble contrast agent.
B2: Typical hypervascularity (enhancement) of HCC is seen during the arterial phase 95 seconds after injection of the contrast agent.
B3, B4: mass becomes hypoechoic in the portal and late phases, with the B4 late-phase image showing mild washout of contrast medium at 179 seconds, which helps differentiate HCC from cholangiocarcinoma or metastatic tumor, which have more rapid washout times.
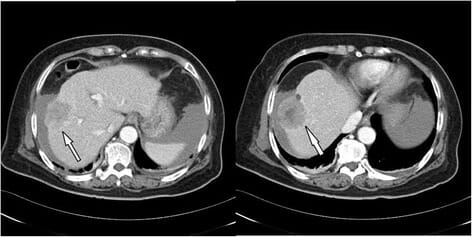
Hepatocellular carcinoma on CT:
Triphasic abdominal CT revealing a large tumor (4.8 cm in diameter) in the right lobe, compatible with HCC (arrow)
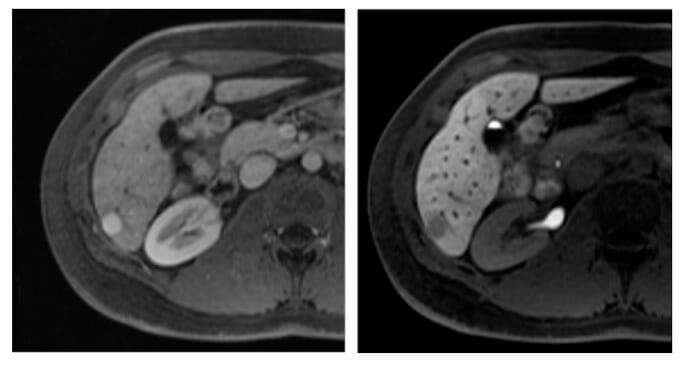
Hepatocellular carcinoma (HCC) on MRI:
Axial MR images of the liver obtained after IV administration of a hepatocyte-specific contrast agent in arterial (left) and hepatobiliary (right) phases obtained 20 minutes after IV contrast application.
A hypervascular lesion is observed (left image, arrow pointing to lesion). In the hepatobiliary phase image in the image on the right, the lesion (at arrow) is hypointense in relation to the surrounding liver due to reduced uptake of contrast agent (attributed to the loss of functioning hepatocytes in the poorly differentiated HCC lesion).
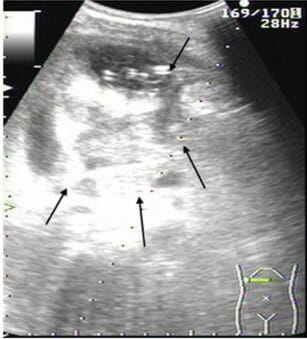
Abdominal ultrasonography scan of liver abscess in right lobe of the liver:
Large (82 mm × 78 mm) multiple low-signal areas (arrows)
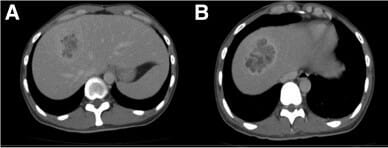
CT images of a liver abscess:
A: Cystic heterogeneous lesion in segment 8 of the right liver lobe, with a partly liquefied component.
B: Axial images showing a rim-enhancing lesion with central hypoattenuation, pointing to an abscess
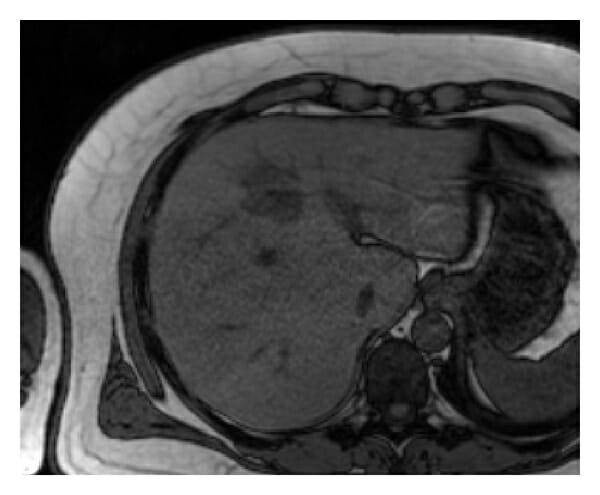
MRI of the liver showing an abscess:
The nodular mass is hypointense on axial T1-weighted out-of-phase MRI.
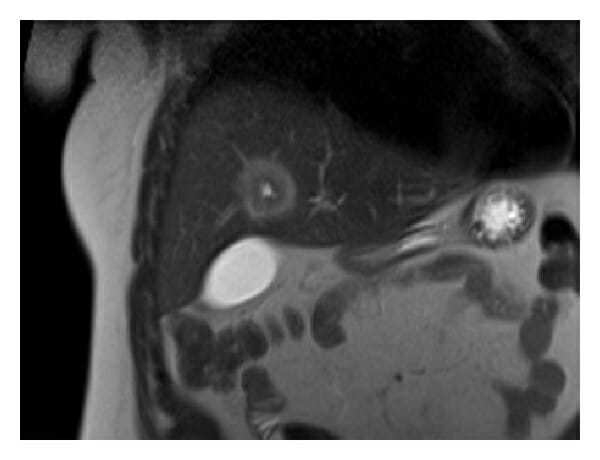
MRI of the liver showing an abscess:
The lesion exhibits a target-like appearance on coronal T2-weighted MRI, with the rim having higher signal intensity than the central component.

Ultrasound image showing a diffusely hyperechoic lesion representing a hemangioma
Image: “Fig3” by Kaltenbach, T.E. et al. License: CC BY 4.0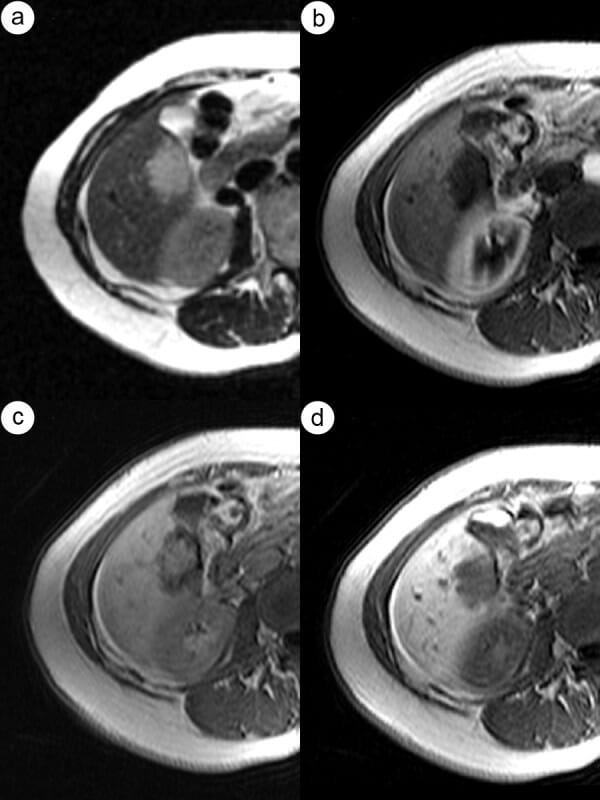
CT and MR images of hepatic hemangioma:
a: Hepatic arterial phase (HAP)–CT image visualizes globular type of enhancement.
b: Globular pattern of enhancement is also visible in HAP–MR image.
c and d: Progressive fill-in enhancement pattern can be observed in the portal venous (c) and equilibrium (d) phases of the MR study.
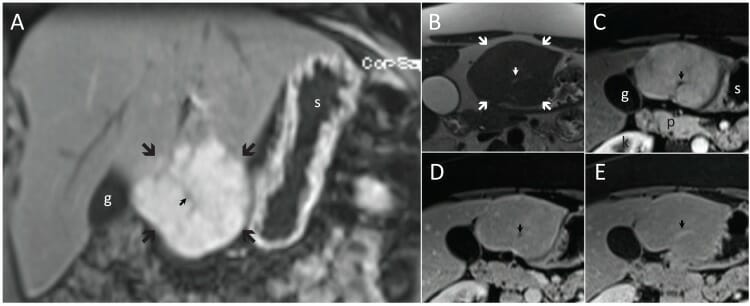
Typical focal nodular hyperplasia ( FNH, large arrows) in coronal (A) and transverse planes (B–E). Focal nodular hyperplasia is slightly hyperintense to the liver on T2 (B) and enhances richly on T1 in the arterial phase (A and C) followed by isointensity in the delayed phases (D and E).
Note the central scar (small arrow), which is hyperintense on T2 (B) and hypointense on T1 in arterial (A and C) and portal venous (D) phases, and hyperintense after 5 minutes (E).
g: gallbladder
k: right kidney
p: pancreas
s: stomach
Image: “F4” by Albiin, N. License: CC BY 2.5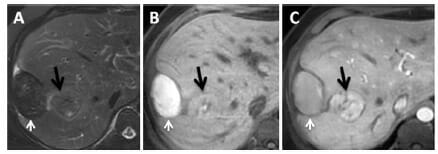
MRI in a patient with adenoma with bleeding:
A: A T2 sequence with fat saturation shows a hepatic subcapsular nodule with hypointense signal.
B: A precontrast T1 sequence reveals a lesion with a hyperintense signal, indicating products of hemoglobin degradation
C: A postcontrast T1 sequence in the arterial phase emphasizes the intrahepatic lesion, where the black arrow points to the lesion and the white arrow to the hematoma.