Hereditary hemochromatosis (HH) is an autosomal recessive Autosomal recessive Autosomal inheritance, both dominant and recessive, refers to the transmission of genes from the 22 autosomal chromosomes. Autosomal recessive diseases are only expressed when 2 copies of the recessive allele are inherited. Autosomal Recessive and Autosomal Dominant Inheritance disorder most often associated with HFE gene Gene A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. Basic Terms of Genetics mutations. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship have increased iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements intestinal absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption and iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements deposition in several organs, such as the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, heart, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, and pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy. The clinical presentation includes the triad of cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, and skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions bronzing. Other findings depend on the organ(s) involved. Diagnosis consists of iron studies Iron Studies Iron Deficiency Anemia, showing transferrin Transferrin An iron-binding beta1-globulin that is synthesized in the liver and secreted into the blood. It plays a central role in the transport of iron throughout the circulation. Heme Metabolism (Tf) and ferritin elevation. Genetic screening Genetic Screening Physical Examination of the Newborn is recommended among family members. Imaging and invasive studies are performed depending on the associated complications. Management requires phlebotomy (or iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements chelation therapy in some cases) to prevent disease progression. The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is good for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are early in the disease and undergoing treatment. The presence of hepatic fibrosis Hepatic fibrosis Autosomal Recessive Polycystic Kidney Disease (ARPKD) is a poor prognostic factor.
Last updated: Apr 26, 2025
Hereditary hemochromatosis (HH) is:
It is important to note that causes of iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements overload may overlap or occur at the same time.
Secondary iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements overload disorders (acquired):
Certain conditions require a decrease or increase in iron absorption Iron absorption Digestion and Absorption and circulating iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements, a pathway regulated by hepcidin:
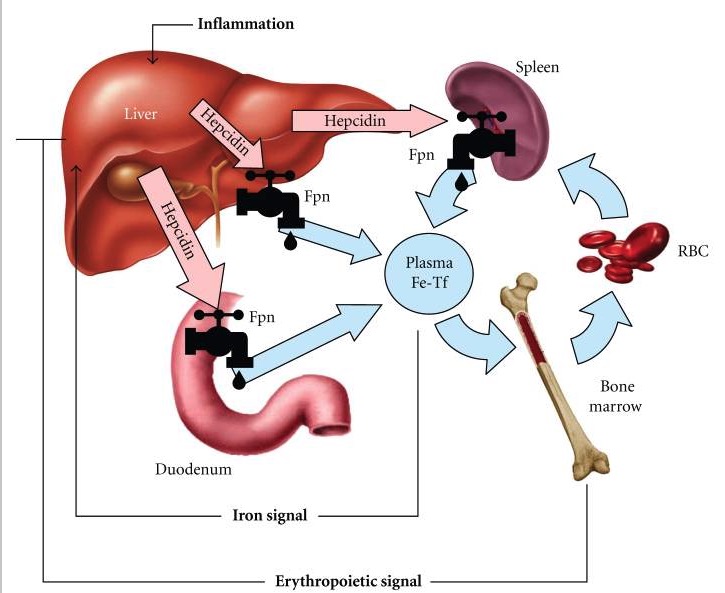
Hepcidin-ferroportin (Fpn) interaction determines the flow of iron into plasma:
1. Dietary iron undergoes intestinal uptake in the duodenum.
2.
Iron moves from the duodenum via the iron exporter, ferroportin (Fpn), and enters the circulation via transferrin (Tf).
3.
Tf supplies iron to the bone marrow for hemoglobin synthesis.
4.
As the red blood cells (RBC) age, they are phagocytosed by macrophages (mainly in the spleen), releasing iron again into the circulation through ferroportin.
5.
When there is increased iron or inflammation, the liver-derived hepcidin increases; this reduces duodenal absorption or iron and the release of iron from the degradation of old RBCs.
6.
When there is a need for more RBC formation, erythropoietin inhibits hepcidin to allow more iron absorption (from the intestine) and release from the macrophages with RBCs.
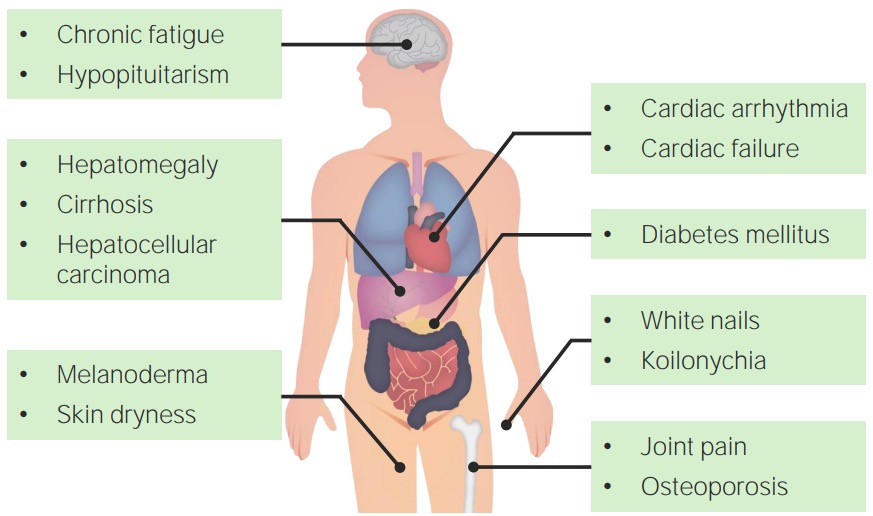
Clinical features of hemochromatosis
Image by Lecturio.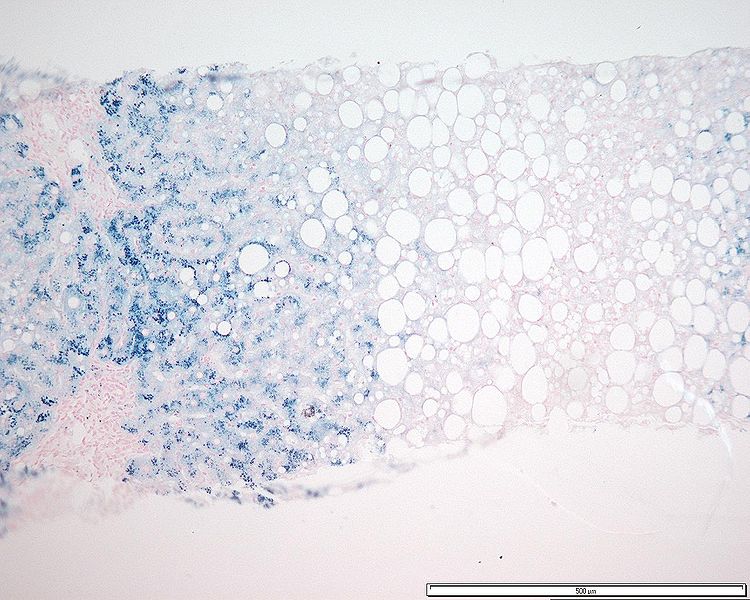
Hepatocyte iron accumulation in a patient with hemochromatosis (stained with Perls Prussian blue)
Image: “Grade 3 hepatocyte iron accumulation” by Mathew, J. et al. License: CC BY 3.0.