Hypoparathyroidism is defined as reduced parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone (PTH) levels due to poor function of the parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy glands. The cause of hypoparathyroidism is most commonly iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome following neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess surgery, but it can also be associated with genetic or autoimmune disorders as well as infiltrative diseases causing destruction of the normal parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy tissue. Deficiency of PTH results in hypocalcemia Hypocalcemia Hypocalcemia, a serum calcium < 8.5 mg/dL, can result from various conditions. The causes may include hypoparathyroidism, drugs, disorders leading to vitamin D deficiency, and more. Calcium levels are regulated and affected by different elements such as dietary intake, parathyroid hormone (PTH), vitamin D, pH, and albumin. Presentation can range from an asymptomatic (mild deficiency) to a life-threatening condition (acute, significant deficiency). Hypocalcemia, which leads to increased neuromuscular excitability Excitability Skeletal Muscle Contraction and osteosclerosis Osteosclerosis An abnormal hardening or increased density of bone tissue. Paget Disease of Bone, as well as cardiac and neuropsychiatric manifestations. Treatment is based on calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes and vitamin D Vitamin D A vitamin that includes both cholecalciferols and ergocalciferols, which have the common effect of preventing or curing rickets in animals. It can also be viewed as a hormone since it can be formed in skin by action of ultraviolet rays upon the precursors, 7-dehydrocholesterol and ergosterol, and acts on vitamin D receptors to regulate calcium in opposition to parathyroid hormone. Fat-soluble Vitamins and their Deficiencies supplementation.
Last updated: May 17, 2024
Hypoparathyroidism is a condition associated with insufficient secretion Secretion Coagulation Studies of parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone (PTH). Hypocalcemia Hypocalcemia Hypocalcemia, a serum calcium < 8.5 mg/dL, can result from various conditions. The causes may include hypoparathyroidism, drugs, disorders leading to vitamin D deficiency, and more. Calcium levels are regulated and affected by different elements such as dietary intake, parathyroid hormone (PTH), vitamin D, pH, and albumin. Presentation can range from an asymptomatic (mild deficiency) to a life-threatening condition (acute, significant deficiency). Hypocalcemia and hyperphosphatemia Hyperphosphatemia A condition of abnormally high level of phosphates in the blood, usually significantly above the normal range of 0. 84-1. 58 mmol per liter of serum. Hypocalcemia are the pathognomonic biochemical features of hypoparathyroidism, and result directly from a lack of PTH action on the kidney.
Normal physiology of PTH:
Effects of hypoparathyroidism:
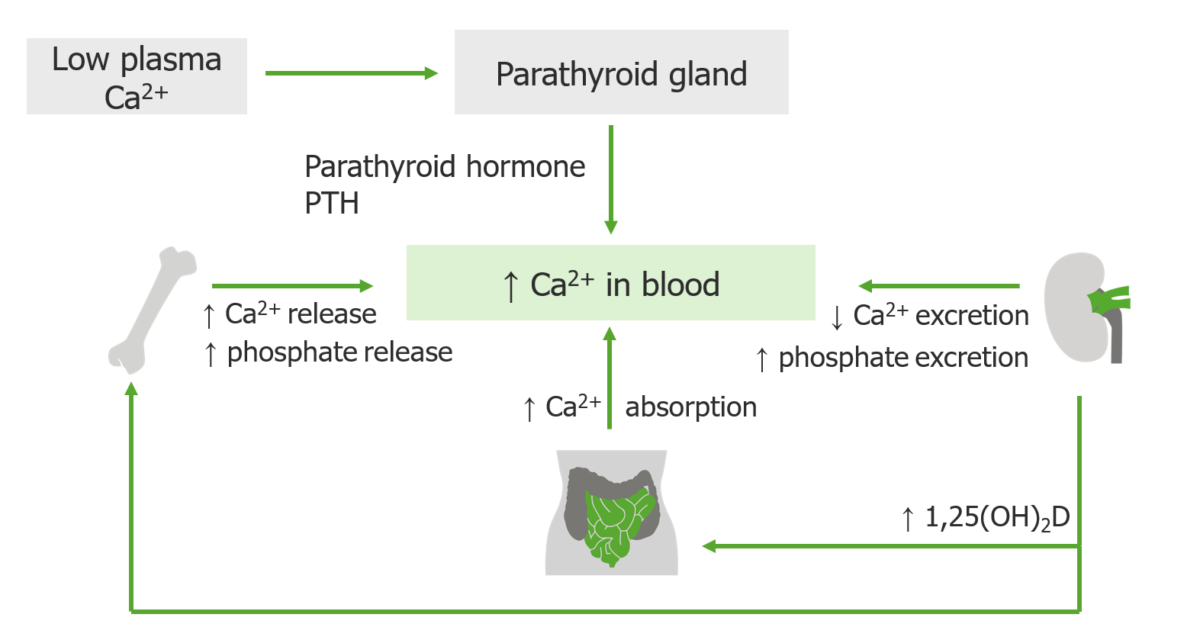
Parathyroid hormone has only one function: to correct hypocalcemia and maintain the serum level of calcium within narrow limits.
If the serum calcium is low, the four parathyroid glands secrete PTH, which is made and stored in the glands. When released, PTH works with and through vitamin D to restore the calcium level to normal.
Acute:
Chronic:

Chvostek’s sign: Induced by tapping on the facial nerve in the area of the cheek, leading to twitching of the mouth musculature
Image: “Use of botulinum toxin in head and face medicine: An interdisciplinary field” by Laskawi R. License: CC BY 2.0
Trousseau’s sign of latent tetany: Induced by applying a BP cuff and inflating to a pressure greater than the systolic pressure
Image: “Trousseau’s Sign of Latent Tetany” by Huckfinne. License: Public DomainHistory:
Physical exam:
Laboratory studies:
| Diagnosis | PTH | Phosphate Phosphate Inorganic salts of phosphoric acid. Electrolytes | Vitamin D Vitamin D A vitamin that includes both cholecalciferols and ergocalciferols, which have the common effect of preventing or curing rickets in animals. It can also be viewed as a hormone since it can be formed in skin by action of ultraviolet rays upon the precursors, 7-dehydrocholesterol and ergosterol, and acts on vitamin D receptors to regulate calcium in opposition to parathyroid hormone. Fat-soluble Vitamins and their Deficiencies | Magnesium Magnesium A metallic element that has the atomic symbol mg, atomic number 12, and atomic weight 24. 31. It is important for the activity of many enzymes, especially those involved in oxidative phosphorylation. Electrolytes | Clinical clues |
|---|---|---|---|---|---|
| Hypoparathyroidism | Low | High | High/low | Normal | History of neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess surgery, irradiation, or autoimmune disease |
| Vitamin D deficiency Vitamin D Deficiency A nutritional condition produced by a deficiency of vitamin D in the diet, insufficient production of vitamin D in the skin, inadequate absorption of vitamin D from the diet, or abnormal conversion of vitamin D to its bioactive metabolites. It is manifested clinically as rickets in children and osteomalacia in adults. Fat-soluble Vitamins and their Deficiencies | High or normal | Low | Low (25-hydroxyvitamin D) | Normal | Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types tenderness, weakness, and osteomalacia Osteomalacia Disorder caused by an interruption of the mineralization of organic bone matrix leading to bone softening, bone pain, and weakness. It is the adult form of rickets resulting from disruption of vitamin d; phosphorus; or calcium homeostasis. Osteomalacia and Rickets |
| Hungry bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types syndrome | Low | Low | Low | Acute bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types uptake of Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)/P and Mg after parathyroidectomy Parathyroidectomy Excision of one or more of the parathyroid glands. Hyperparathyroidism | |
| Magnesium deficiency Magnesium Deficiency A nutritional condition produced by a deficiency of magnesium in the diet, characterized by anorexia, nausea, vomiting, lethargy, and weakness. Symptoms are paresthesias, muscle cramps, irritability, decreased attention span, and mental confusion, possibly requiring months to appear. Deficiency of body magnesium can exist even when serum values are normal. In addition, magnesium deficiency may be organ-selective, since certain tissues become deficient before others. Electrolytes (impaired PTH secretion Secretion Coagulation Studies and PTH resistance PTH resistance Hypocalcemia) | Normal or low | Normal | Normal | Low |
|
| CKD CKD Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease | High | High | Low |
|
Acute hypoparathyroidism:
Chronic hypoparathyroidism: