Hypocalcemia, a serum calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes < 8.5 mg/dL, can result from various conditions. The causes may include hypoparathyroidism Hypoparathyroidism Hypoparathyroidism is defined as reduced parathyroid hormone (PTH) levels due to poor function of the parathyroid glands. The cause of hypoparathyroidism is most commonly iatrogenic following neck surgery, but it can also be associated with genetic or autoimmune disorders as well as infiltrative diseases causing destruction of the normal parathyroid tissue. Hypoparathyroidism, drugs, disorders leading to vitamin D deficiency Vitamin D Deficiency A nutritional condition produced by a deficiency of vitamin D in the diet, insufficient production of vitamin D in the skin, inadequate absorption of vitamin D from the diet, or abnormal conversion of vitamin D to its bioactive metabolites. It is manifested clinically as rickets in children and osteomalacia in adults. Fat-soluble Vitamins and their Deficiencies, and more. Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes levels are regulated and affected by different elements such as dietary intake, parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone (PTH), vitamin D Vitamin D A vitamin that includes both cholecalciferols and ergocalciferols, which have the common effect of preventing or curing rickets in animals. It can also be viewed as a hormone since it can be formed in skin by action of ultraviolet rays upon the precursors, 7-dehydrocholesterol and ergosterol, and acts on vitamin D receptors to regulate calcium in opposition to parathyroid hormone. Fat-soluble Vitamins and their Deficiencies, pH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance, and albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests. Presentation can range from an asymptomatic (mild deficiency) to a life-threatening condition (acute, significant deficiency). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can exhibit symptoms from neuromuscular irritability (tetany, Chvostek sign, Trousseau sign) to cardiovascular dysfunction (arrhythmia). Confirmation of hypocalcemia is required with correction of the value depending on albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests level or ionized calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes (the metabolically active form), followed by PTH level, and determination of the underlying cause. Correction of calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes is dictated by the degree of severity of hypocalcemia. In severe cases, IV calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes administration is required. Treatment of the underlying cause is recommended.
Last updated: May 16, 2024
Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes is the most abundant mineral in the human body; 99% is found in bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types. Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes in the blood exists in 3 forms:
Levels:
Importance of calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes:
Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, intestine, and kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy are involved in homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death.
Key elements of calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes regulation:
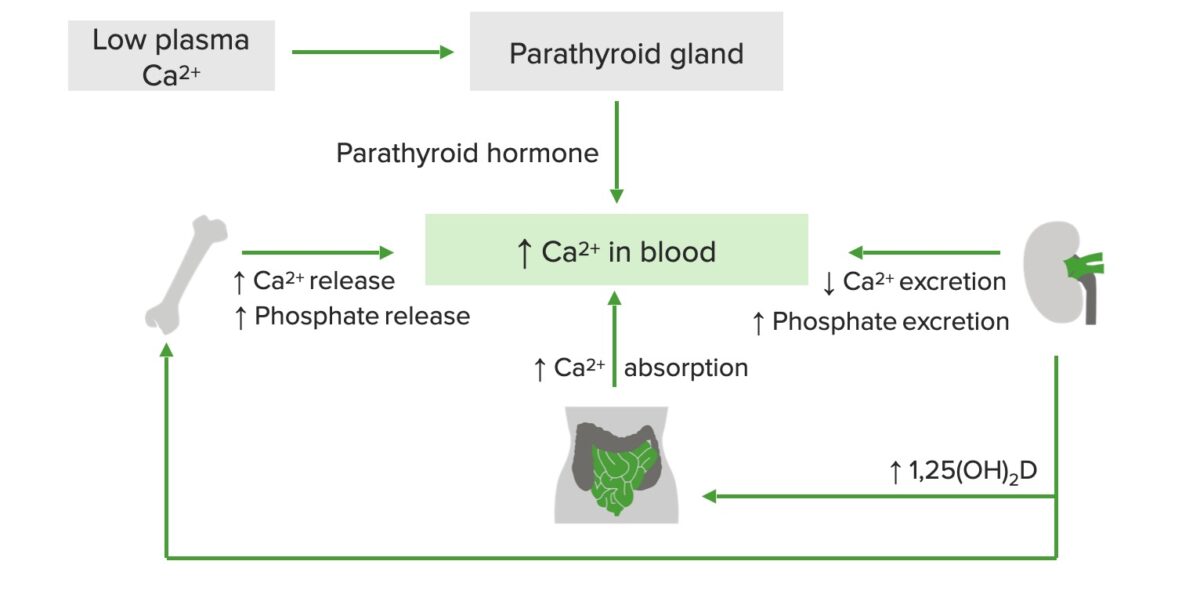
Schematic diagram of calcium regulation:
Low plasma calcium stimulates the release of parathyroid hormone (PTH), which increases calcium and phosphate release from bones, calcium absorption in the GI tract, and vitamin D production in the kidneys. In turn, active vitamin D increases calcium release from bones and calcium absorption in the small intestine.
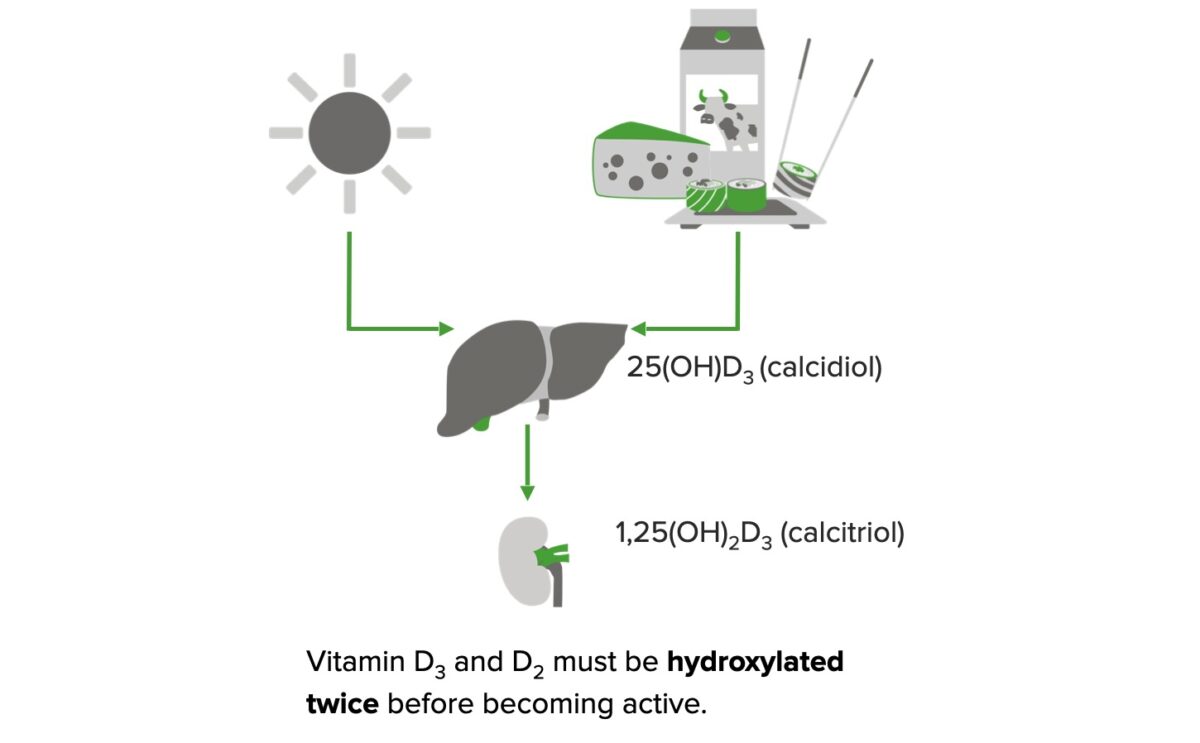
Formation of active vitamin D:
In the presence of sunlight, 7-dehydrocholesterol is converted to cholecalciferol (vitamin D3) in the skin.
Vitamin D2 (plant sources/supplements) and vitamin D3 (animal sources/supplements) are obtained from the diet.
Both forms require a 2-step enzymatic hydroxylation process before they can exert biological effects.
Vitamin D2/D3 is converted to 25-hydroxy vitamin D3 (calcidiol) in the liver. In the kidney, calcidiol is converted to 1,25-dihydroxy vitamin D3 (calcitriol), which is the active form.
Associated with ↑ PTH:
Hypoparathyroidism Hypoparathyroidism Hypoparathyroidism is defined as reduced parathyroid hormone (PTH) levels due to poor function of the parathyroid glands. The cause of hypoparathyroidism is most commonly iatrogenic following neck surgery, but it can also be associated with genetic or autoimmune disorders as well as infiltrative diseases causing destruction of the normal parathyroid tissue. Hypoparathyroidism (↓ PTH):
Drug induced:
Others:
Manifestations depend on the level and onset of hypocalcemia:
Symptoms:

Trousseau sign:
Trousseau sign is induced by inflating the blood pressure cuff above systolic pressure for 3 minutes. The sign is demonstrated by an adducted thumb, flexed metacarpophalangeal joints, extended interphalangeal joints, and flexed wrist.

Chvostek sign:
Chvostek sign is Induced by tapping on the facial nerve of the cheek, which leads to twitching of the mouth musculature.
| Diagnosis | Hypoparathyroidism Hypoparathyroidism Hypoparathyroidism is defined as reduced parathyroid hormone (PTH) levels due to poor function of the parathyroid glands. The cause of hypoparathyroidism is most commonly iatrogenic following neck surgery, but it can also be associated with genetic or autoimmune disorders as well as infiltrative diseases causing destruction of the normal parathyroid tissue. Hypoparathyroidism | Vitamin D deficiency Vitamin D Deficiency A nutritional condition produced by a deficiency of vitamin D in the diet, insufficient production of vitamin D in the skin, inadequate absorption of vitamin D from the diet, or abnormal conversion of vitamin D to its bioactive metabolites. It is manifested clinically as rickets in children and osteomalacia in adults. Fat-soluble Vitamins and their Deficiencies | Magnesium deficiency Magnesium Deficiency A nutritional condition produced by a deficiency of magnesium in the diet, characterized by anorexia, nausea, vomiting, lethargy, and weakness. Symptoms are paresthesias, muscle cramps, irritability, decreased attention span, and mental confusion, possibly requiring months to appear. Deficiency of body magnesium can exist even when serum values are normal. In addition, magnesium deficiency may be organ-selective, since certain tissues become deficient before others. Electrolytes | Chronic kidney disease Chronic Kidney Disease Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease |
|---|---|---|---|---|
| PTH | Low | High | Normal/low | High |
| Phos | High | Low | Normal | High |
| 25(OH)D | Normal | Low* | Normal | Normal/low |
| 1,25(OH)2D | Normal/low | Normal/high* | Normal | Low |
| Mg | Normal | Normal | Low | Normal/high |
| Clinical clues |
|
|
|
Abnormal creatinine |
Management depends on the underlying cause and severity.
Approach for:
Treatment:
Approach for:
Treatment:
The following are conditions related to hypocalcemia: