Ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children is any heart rhythm faster than 100 beats/min, with 3 or more irregular beats in a row, arising distal to the bundle of His Bundle of His Small band of specialized cardiac muscle fibers that originates in the atrioventricular node and extends into the membranous part of the interventricular septum. The bundle of his, consisting of the left and the right bundle branches, conducts the electrical impulses to the heart ventricles in generation of myocardial contraction. Heart: Anatomy. Ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children is the most common form of wide-complex tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, and it is associated with a high mortality Mortality All deaths reported in a given population. Measures of Health Status rate. Ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children is often caused by myocardial ischemia Myocardial ischemia A disorder of cardiac function caused by insufficient blood flow to the muscle tissue of the heart. The decreased blood flow may be due to narrowing of the coronary arteries (coronary artery disease), to obstruction by a thrombus (coronary thrombosis), or less commonly, to diffuse narrowing of arterioles and other small vessels within the heart. Coronary Heart Disease, structural disease, congenital Congenital Chorioretinitis conditions, or electrolyte derangement. Individuals may present with chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, palpitations Palpitations Ebstein’s Anomaly, syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope, and hemodynamic instability. Diagnosis is based on characteristic ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) findings of wide-complex QRS, fusion, and capture beats. Management may require antiarrhythmic medications or electrical cardioversion Cardioversion Atrial Fibrillation to avoid complications such as heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), multiorgan failure, and cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest.
Last updated: May 16, 2024
Diagnosis is by ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) or cardiac monitoring.
There are 2 primary types of ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children:
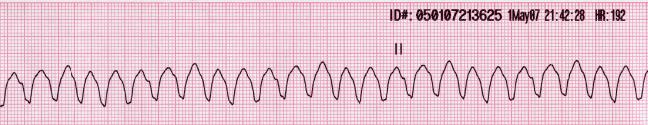
Rhythm strip of ventricular tachycardia showing a regular, wide complex rhythm with a rate over 100/min
This is a shockable rhythm.

Example of an ECG tracing showing beat-to-beat axis deviation of the QRS complexes around the baseline in torsades de pointes
Image: “Torsade de pointes” by Panthro. License: Public DomainManagement of ventricular tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children is based on whether a pulse is present and, if it is, whether the individual is hemodynamically stable.

Management of ventricular tachycardia
Image by Lecturio.Follow the adult cardiac arrest Cardiac arrest Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest algorithm.

Ventricular fibrillation/pulseless ventricular tachycardia management algorithm
Image by Lecturio.