Cardiac arrest is the sudden, complete cessation of cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics with hemodynamic collapse. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation Ventricular fibrillation Ventricular fibrillation (VF or V-fib) is a type of ventricular tachyarrhythmia (> 300/min) often preceded by ventricular tachycardia. In this arrhythmia, the ventricle beats rapidly and sporadically. The ventricular contraction is uncoordinated, leading to a decrease in cardiac output and immediate hemodynamic collapse. Ventricular Fibrillation (V-fib)/ tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, asystole, or pulseless electrical activity. The treatment of cardiac arrest begins with basic life support Basic Life Support Airway Management ( BLS BLS Airway Management) when out-of-hospital and advanced cardiac life support (ACLS) when in-hospital. Basic life support Basic Life Support Airway Management comprises checking the patient’s mental status, activating the emergency response system, and cardiopulmonary resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome (CPR). An automated external defibrillator ( AED AED Cardiac electrical stimulators that apply brief high-voltage electroshocks to the heart. These stimulators are used to restore normal rhythm and contractile function in hearts of patients who are experiencing ventricular fibrillation or ventricular tachycardia that is not accompanied by a palpable pulse. Some defibrillators may also be used to correct certain noncritical dysrhythmias (called synchronized defibrillation or cardioversion), using relatively low-level discharges synchronized to the patient's ECG waveform. Cardiopulmonary Resuscitation (CPR)) should be used once available. High-quality CPR (with early defibrillation Defibrillation Ventricular Fibrillation (V-fib) in shockable rhythms) is crucial to survival in cardiac arrest. Advanced cardiac life support includes CPR, securing the airway Airway ABCDE Assessment, administering medications (such as epinephrine Epinephrine The active sympathomimetic hormone from the adrenal medulla. It stimulates both the alpha- and beta- adrenergic systems, causes systemic vasoconstriction and gastrointestinal relaxation, stimulates the heart, and dilates bronchi and cerebral vessels. Sympathomimetic Drugs), and identifying and treatment of the cause of cardiac arrest. Post-cardiac arrest care follows return of spontaneous circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment (ROSC).
Last updated: May 17, 2024
Sudden cardiac arrest (SCA) is the abrupt cessation of cardiac activity.
The 5 Hs HS Hypertrophic scars and keloids are raised, red, and rigid (3 rs) scars that develop during cutaneous wound healing and are characterized by a local abnormal proliferation of fibroblasts with over-production of collagen. Over-expression of growth factors and decreased production of molecules that promote matrix breakdown appear to be involved in the etiology. Hypertrophic and Keloid Scars and 5 Ts of the common reversible causes of SCA:
Four major cardiac rhythms are associated with SCA. These rhythms are divided into shockable and non-shockable rhythms.
Shockable rhythms are usually caused by primary cardiac disease (most commonly ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage). Less commonly, they are caused by systemic conditions (electrolyte disturbances, toxins, autoimmunity Autoimmunity Autoimmunity is a pathologic immune response toward self-antigens, resulting from a combination of factors: immunologic, genetic, and environmental. The immune system is equipped with self-tolerance, allowing immune cells such as T cells and B cells to recognize self-antigens and to not mount a reaction against them. Defects in this mechanism, along with environmental triggers (such as infections) and genetic susceptibility factors (most notable of which are the HLA genes) can lead to autoimmune diseases. Autoimmunity).
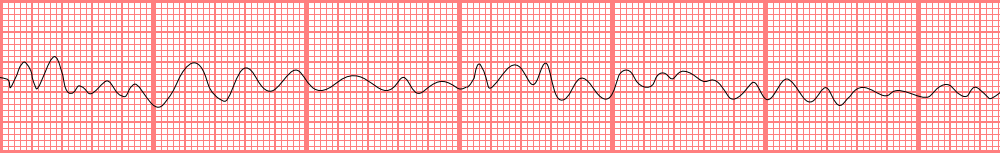
Ventricular fibrillation
Rhythm strip of VF showing the disorganized electrical activity originating in the ventricles.
The rhythm is a shockable rhythm.
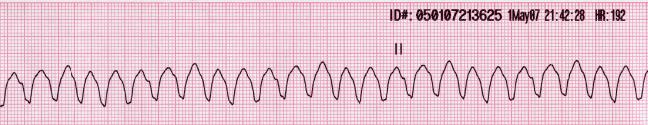
Ventricular tachycardia
Rhythm strip of VT showing a regular, wide complex rhythm with a rate over 100/min.
This rhythm is a shockable rhythm.
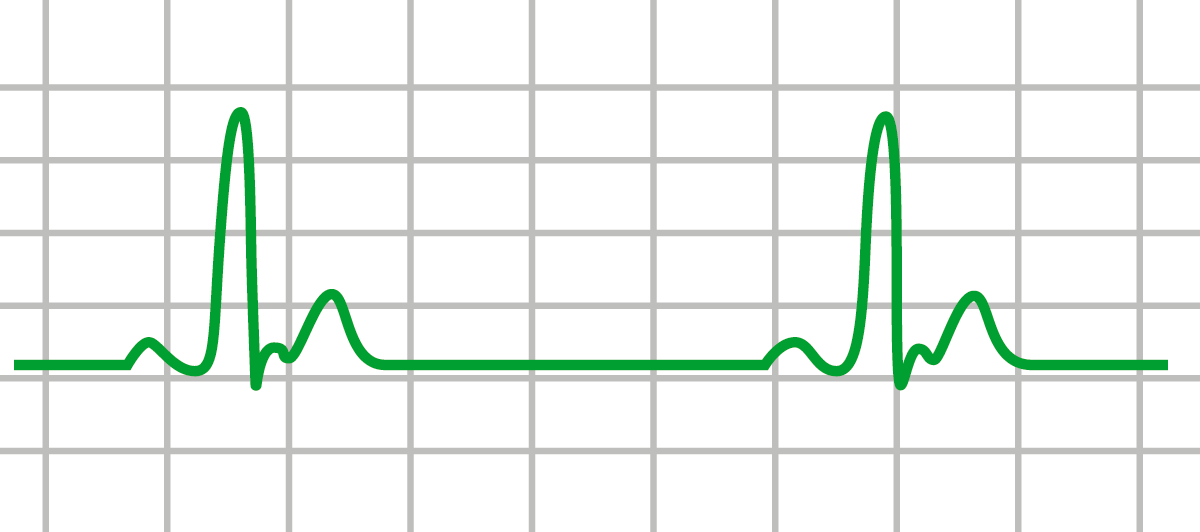
Pulseless electrical activity (PEA): ECG with an organized electrical rhythm. On exam, however, the patient has no pulse
Image by Lecturio.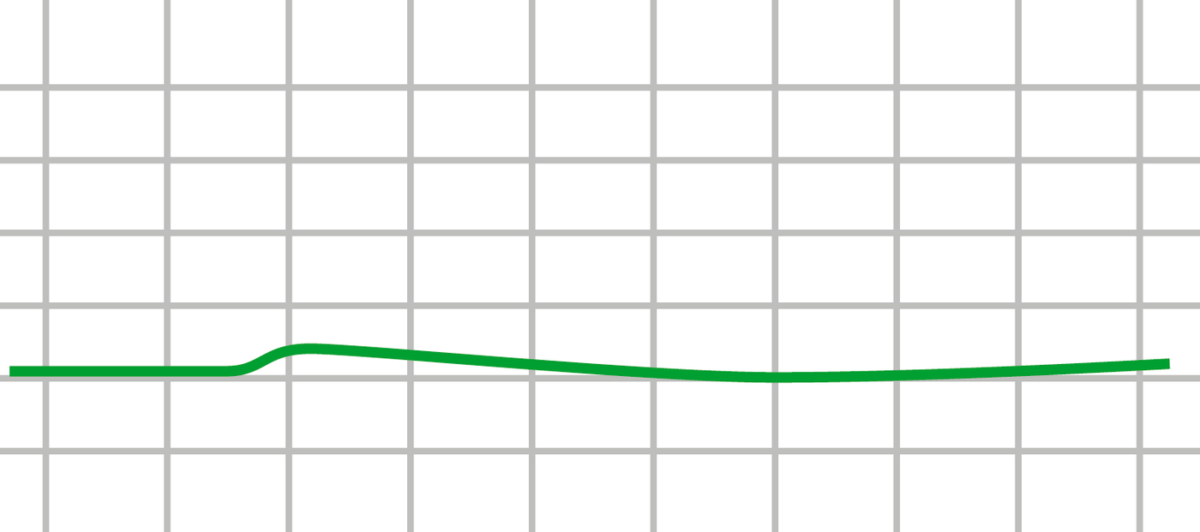
Asystole: ECG of asystole (flat line) showing the absence of electrical activity in the heart
Image by Lecturio.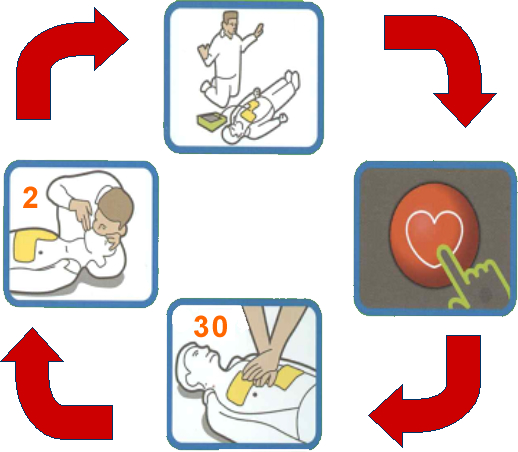
General CPR cycle: (start: bottom image)
1. Upon recognition of cardiac arrest, give 30 firm chest compressions.
2. Follow the compressions with 2 rescue breaths.
3. When an AED arrives, place pads in appropriate areas.
4. When prompted by the AED, check rhythm and deliver the shock when indicated (after making sure that no one is in physical contact with the patient).
Resume CPR cycle after shock delivery.
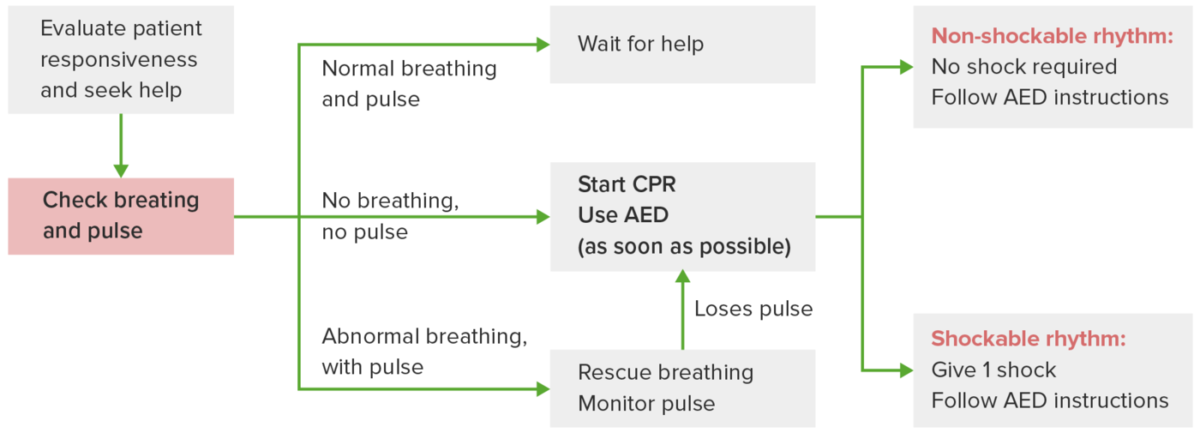
Different scenarios illustrating the use of adult basic life support (BLS)
Once possible cardiac arrest is recognized, a rapid evaluation is needed. If there is normal breathing and pulse, monitor and stay with the patient until help arrives. If there is abnormal breathing (gasping) and normal pulse, rescue breaths are recommended. If no breathing and no pulse are noted, begin CPR and use AED as soon as possible, following the prompts. Non-shockable rhythm indicates continuation of CPR. Shockable rhythm indicates the delivery of shock and the need to resume CPR immediately.
Abbreviations:
AED: automated external defibrillator
CPR: cardiopulmonary resuscitation

Public access defibrillation
Because cardiac arrest is a cause of avoidable death, public access defibrillation programs ensure the availability of AEDs for immediate use by lay bystanders whenneeded.
Circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment, airway Airway ABCDE Assessment, breath is the advanced cardiac life support mantra. Since 2010, management has focused on starting chest compressions Chest Compressions Cardiopulmonary Resuscitation (CPR) first to address circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment, then airway Airway ABCDE Assessment access and rescue breathing Rescue Breathing Drowning.
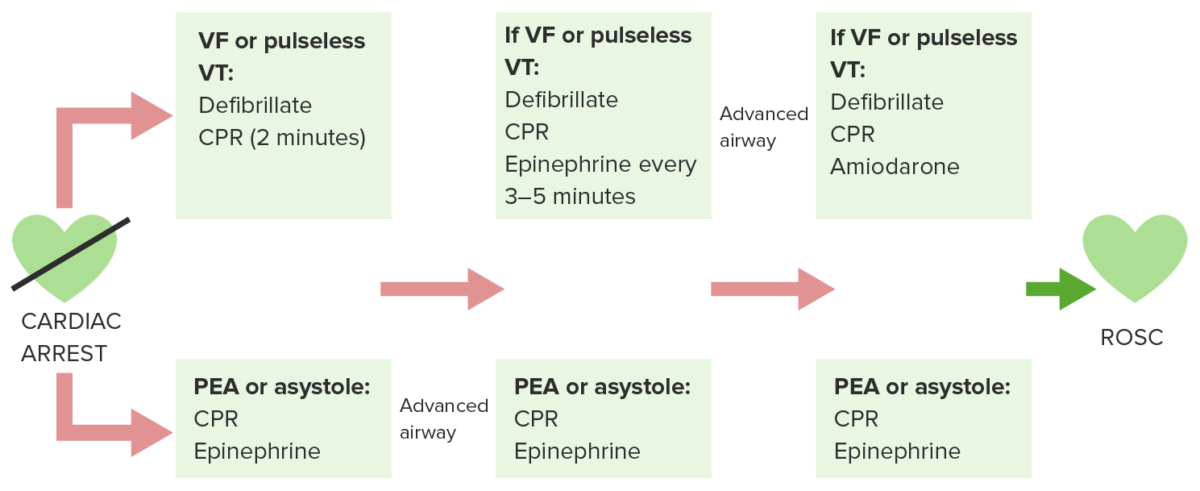
Adult cardiac arrest diagram
Upon recognition of cardiac arrest, rapid evaluation of breathing, pulse and rhythm (once cardiac monitor is available) is done and cardiopulmonary resuscitation (CPR) is initiated. Defibrillate shockable rhythms, ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). If with pulseless electrical activity/asystole, CPR continues. Simultaneously through the process, intravenous (IV) access (or intraosseous access) is obtained to administer needed medications. IV epinephrine is given every 3–5 minutes.
Endotracheal intubation (advanced airway) is performed. Quantitative waveform capnography (which shows end-tidal (et)CO₂) is monitored. If (et)CO₂ is low, reassess CPR quality.
Cycle of steps (defibrillation and/or CPR with minimal interruption + airway support → rhythm, pulse and blood pressure check → IV medication administration) continues until return of spontaneous circulation (ROSC). Continuation of the cycle is also assessed if there is no ROSC. Signs of ROSC are: pulse and blood pressure present, abrupt sustained increase in etCO₂ (about ≥ 40 mm Hg) and spontaneous arterial pressure waves with intra-arterial monitoring.
Return of spontaneous circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment signs
Criteria for termination of resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome:
The following conditions are causes of cardiac arrest: