Pleuritis, also known as pleurisy, is an inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the visceral and parietal Parietal One of a pair of irregularly shaped quadrilateral bones situated between the frontal bone and occipital bone, which together form the sides of the cranium. Skull: Anatomy layers of the pleural membranes of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy. The condition can be primary or secondary and results in sudden, sharp, and intense chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways on inhalation and exhalation. Etiologies include infection, trauma, cardiac ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, and lung cancer Lung cancer Lung cancer is the malignant transformation of lung tissue and the leading cause of cancer-related deaths. The majority of cases are associated with long-term smoking. The disease is generally classified histologically as either small cell lung cancer or non-small cell lung cancer. Symptoms include cough, dyspnea, weight loss, and chest discomfort. Lung Cancer. The most common primary infectious cause is a viral infection, and underlying lung infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease account for the majority of secondary infectious causes. Management consists of pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways control and the treatment of the underlying condition.
Last updated: May 17, 2024
| Transudate Transudate Transudates are fluids that pass through a membrane or squeeze through tissue or into the extracellular space of tissues. Transudates are thin and watery and contain few cells or proteins. Pleural Effusion | Exudate Exudate Exudates are fluids, cells, or other cellular substances that are slowly discharged from blood vessels usually from inflamed tissues. Pleural Effusion | |
|---|---|---|
| Protein (pleural/serum) | ≤ 0.5 | > 0.5 |
| LDH LDH Osteosarcoma (pleural/serum) | ≤ 0.6 | > 0.6 |
| Pleural LDH LDH Osteosarcoma ≤ two-thirds upper limit Limit A value (e.g., pressure or time) that should not be exceeded and which is specified by the operator to protect the lung Invasive Mechanical Ventilation of normal serum LDH LDH Osteosarcoma | Pleural LDH LDH Osteosarcoma > two-thirds upper limit Limit A value (e.g., pressure or time) that should not be exceeded and which is specified by the operator to protect the lung Invasive Mechanical Ventilation of normal serum LDH LDH Osteosarcoma | |
| Common causes |
|
|
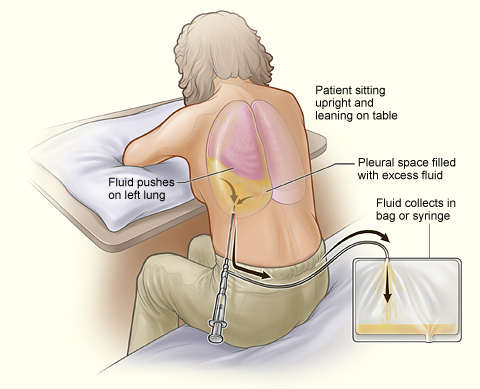
Patient undergoing thoracentesis. Note that the person sits upright and leans on a table. Excess fluid from the pleural space is drained into a bag.
Image: “A person undergoing thoracentesis.” by National Heart, Lung and Blood Institute. License: Public Domain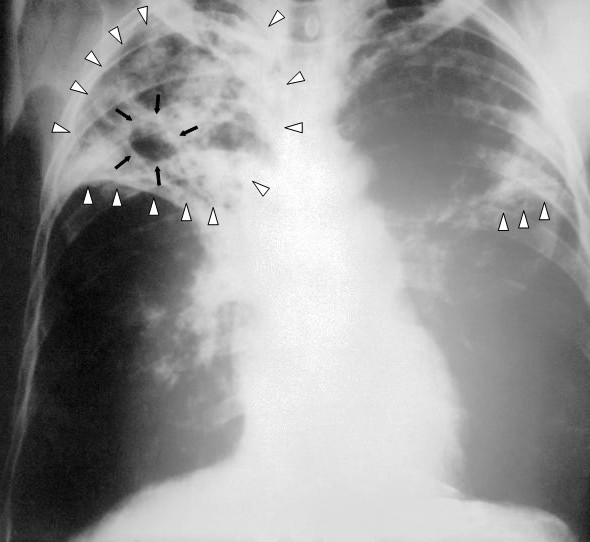
Chest X-ray showing advanced bilateral pulmonary tuberculosis. Notice the presence of bilateral pulmonary infiltrates (white triangles) and cavitary formation (black arrows) in the right apical region.
Image: “An anteroposterior X-ray of a patient diagnosed with advanced bilateral pulmonary tuberculosis” by Centers for Disease Control and Prevention’s Public Health Image Library (PHIL). License: Public Domain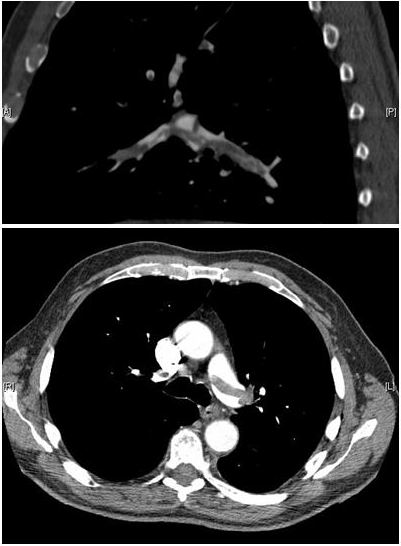
CT pulmonary angiography showing a “saddle embolus” at the bifurcation of the main pulmonary artery and thrombus burden in the lobar arteries on both sides. Can cause pleuritic symptomatology.
Image: “CT pulmonary angiography images confirming the presence of a saddle embolus” by Aung Myat and Arif Ahsan. License: CC BY 2.0