Esophageal rupture or perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis is a transmural defect that occurs in the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy, exposing the mediastinum Mediastinum The mediastinum is the thoracic area between the 2 pleural cavities. The mediastinum contains vital structures of the circulatory, respiratory, digestive, and nervous systems including the heart and esophagus, and major thoracic vessels. Mediastinum and Great Vessels: Anatomy to GI content. The most common cause of esophageal perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis is iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome trauma by instrumentation or surgical procedures. Perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis can also be due to foreign body Foreign Body Foreign Body Aspiration ingestion or non-iatrogenic trauma produced by severe vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. Esophageal perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis presents with substernal chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways that can have a sudden or insidious onset. Diagnosis can be achieved through a CT scan of the chest and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests, or esophagogram. Management commonly includes surgical repair of the transmural esophageal defect. However, conservative therapy may also be considered for a hemodynamically stable patient with a minor defect. The main complication of esophageal perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis is acute mediastinitis Acute Mediastinitis Mediastinitis. The mortality Mortality All deaths reported in a given population. Measures of Health Status rate can range from 10%–50%.
Last updated: Jun 17, 2025
Esophageal perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, also called esophageal rupture, is a transmural defect of the esophageal wall that exposes the mediastinum Mediastinum The mediastinum is the thoracic area between the 2 pleural cavities. The mediastinum contains vital structures of the circulatory, respiratory, digestive, and nervous systems including the heart and esophagus, and major thoracic vessels. Mediastinum and Great Vessels: Anatomy to GI content.
The pathogenesis of esophageal perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis depends on the cause.

Candida esophagitis showing white-yellow plaques
Image: “Esophagogastroduodenoscopy” by Department of Medicine (C-HH), and Institute of Traditional Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan. License: CC BY 4.0History:
Manifestations:
Exam findings:

Posteroanterior chest X-ray showing pneumomediastinum (black arrows) due to esophageal rupture
Image: “Chest X-ray displaying pneumomediastinum” by Faculty of Medicine, University of Toronto, Toronto, ON, Canada. License: CC BY 4.0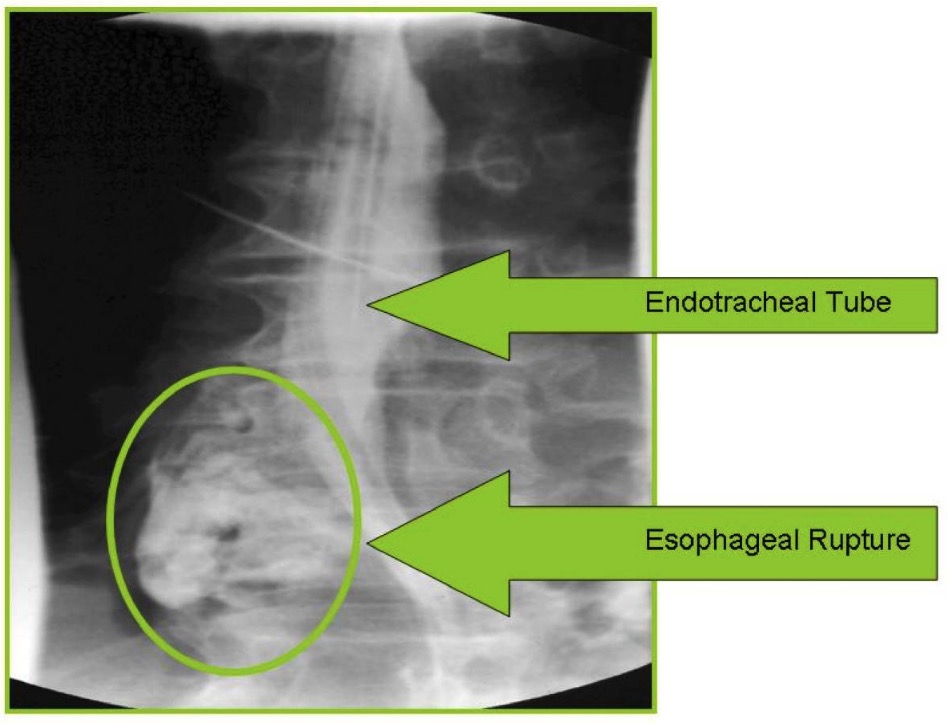
Gastrografin esophagography showing distal esophageal rupture with contrast leak (green circle)
Image: “Intubated patient showing esophageal rupture” by Rockyview General Hospital, Alberta Health Services, 7007-14th Street SW, Calgary, AB, T2P 1P9, Canada. License: CC BY 2.0
Chest CT scan showing distal rupture of the esophagus (white arrow) with contrast leak (black arrow) and pneumomediastinum (asterisk)
Image: “Chest computed tomography” by Faculty of Medicine, University of Toronto, Toronto, ON, Canada. License: CC BY 4.0Initial approach:
Obtain surgical (including cardiothoracic) consult, as even stable patients Stable Patients Blunt Chest Trauma can deteriorate and require surgery.
Further intervention determined by:
Indications:
Procedure:
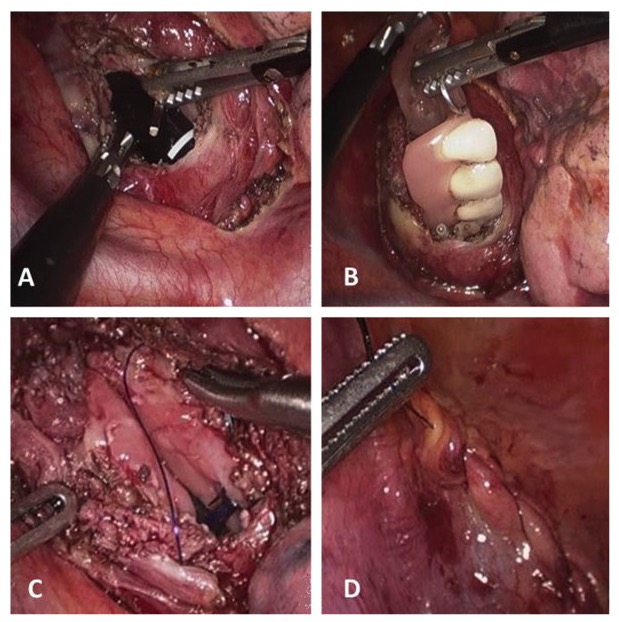
Esophageal perforation by foreign body (dental prosthesis):
A: esophagotomy
B: removal of dental prosthesis
C and D: suture of the esophageal wall and mediastinal pleura