Mediastinitis refers to an infection or inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation involving the mediastinum Mediastinum The mediastinum is the thoracic area between the 2 pleural cavities. The mediastinum contains vital structures of the circulatory, respiratory, digestive, and nervous systems including the heart and esophagus, and major thoracic vessels. Mediastinum and Great Vessels: Anatomy (a region in the thoracic cavity containing the heart, thymus Thymus A single, unpaired primary lymphoid organ situated in the mediastinum, extending superiorly into the neck to the lower edge of the thyroid gland and inferiorly to the fourth costal cartilage. It is necessary for normal development of immunologic function early in life. By puberty, it begins to involute and much of the tissue is replaced by fat. Lymphatic Drainage System: Anatomy gland, portions of the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy, and trachea Trachea The trachea is a tubular structure that forms part of the lower respiratory tract. The trachea is continuous superiorly with the larynx and inferiorly becomes the bronchial tree within the lungs. The trachea consists of a support frame of semicircular, or C-shaped, rings made out of hyaline cartilage and reinforced by collagenous connective tissue. Trachea: Anatomy). Acute mediastinitis can be caused by bacterial infection due to direct contamination, hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases or lymphatic spread, or extension Extension Examination of the Upper Limbs of infection from nearby structures. Chronic mediastinitis, also known as fibrosing mediastinitis, is commonly related to chronic inflammatory conditions that cause the proliferation of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology. Mediastinitis is treated with broad-spectrum Broad-Spectrum Fluoroquinolones antibiotics and surgery, as well as supportive care, depending on the etiology. Mortality Mortality All deaths reported in a given population. Measures of Health Status from this condition is high.
Last updated: Jan 18, 2024
Mediastinum Mediastinum The mediastinum is the thoracic area between the 2 pleural cavities. The mediastinum contains vital structures of the circulatory, respiratory, digestive, and nervous systems including the heart and esophagus, and major thoracic vessels. Mediastinum and Great Vessels: Anatomy:
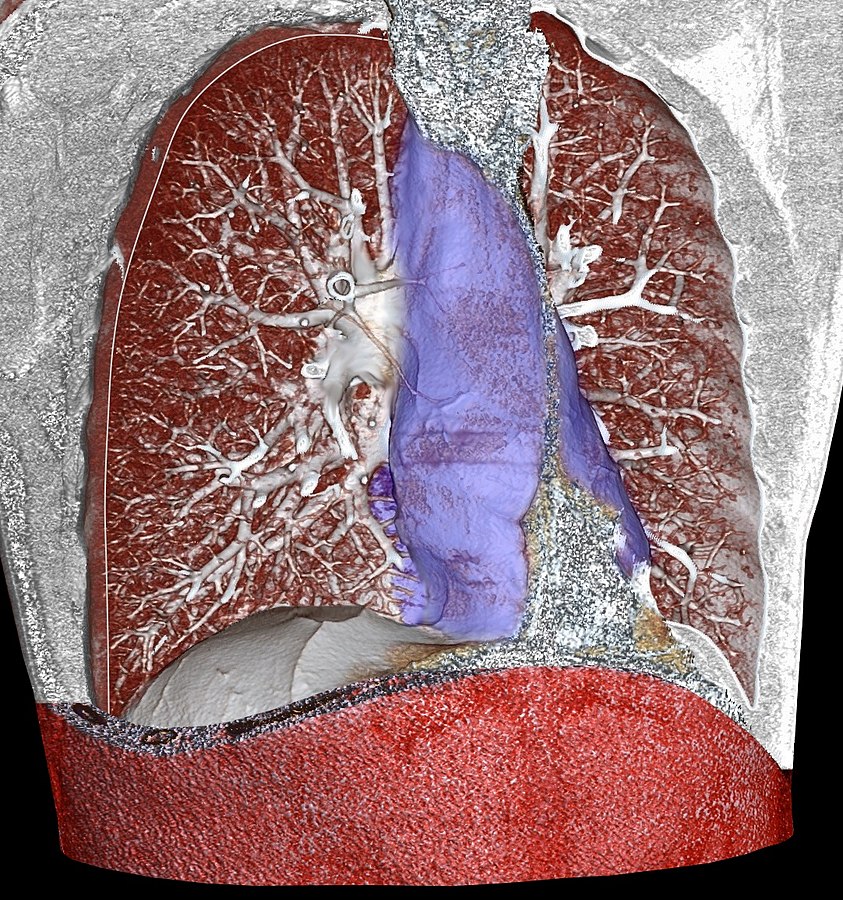
Three-dimensional rendering of high-resolution CT identifying the mediastinum:
The area highlighted in blue is the mediastinum. This area is bordered by the lung pleural sacs laterally, the thoracic outlet above, and the diaphragm below. The structures contained in the mediastinum include the heart, thymus, great vessels (vena cava, aorta, pulmonary arteries), esophagus, distal portion of trachea, mainstem bronchi, and phrenic and vagus nerves.
Acute mediastinitis:
Chronic mediastinitis:
Fibrosing mediastinitis:
Acute mediastinitis:
Chronic mediastinitis:
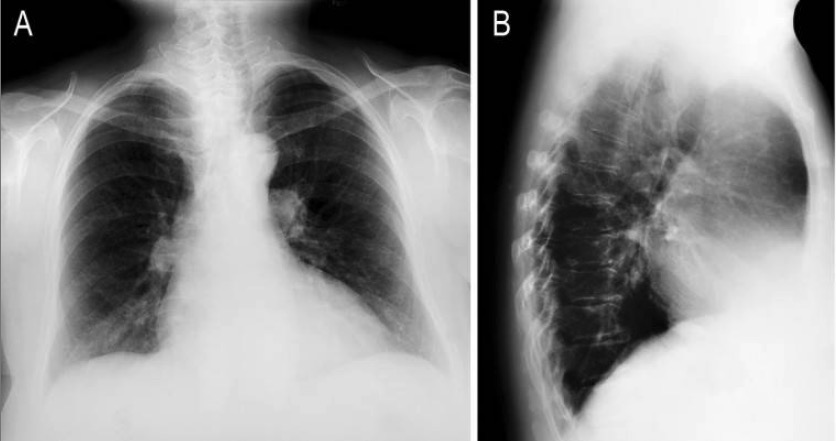
X-rays of mediastinitis:
Widening of the mediastinum can be a nonspecific finding on X-ray, indicating mediastinitis.
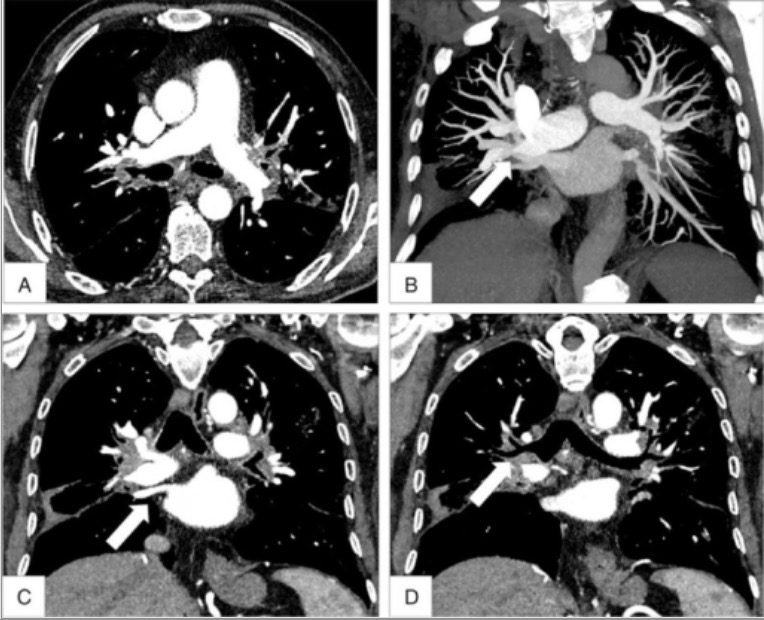
CT of fibrosing mediastinitis:
In fibrosing mediastinitis, chronic inflammation can cause compression of blood vessels and airways, as can be seen in this CT. Panels A and B show compression of both pulmonary arteries, while panel D shows compression of the mainstem bronchi.
Acute mediastinitis:
Chronic fibrosing mediastinitis: