Dacryocystitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the lacrimal sac due to nasolacrimal duct obstruction and the subsequent stasis of tears. The condition can have an acute or chronic onset. Acute dacryocystitis presents within hours or days with redness Redness Inflammation, swelling Swelling Inflammation, tenderness, and excessive tearing. The chronic type has a gradual course, often manifesting with epiphora. Dacryocystitis can be congenital Congenital Chorioretinitis or acquired. The most common etiology of congenital Congenital Chorioretinitis dacryocystitis is nasolacrimal duct obstruction, which affects 6% of newborns. Acquired cases typically occur in adults and are due to trauma, systemic diseases, or tumors. Diagnosis is made clinically. In some cases, laboratory tests and imaging help determine abnormal structures and underlying disease. Initial treatment includes conservative measures such as Crigler massage, warm compresses Warm Compresses Chalazion, and antibiotics, if indicated. If these fail, surgical options are available.
Last updated: May 17, 2024
Dacryocystitis is an inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the lacrimal sac due to nasolacrimal duct (NLD) obstruction and the subsequent stasis of tears.
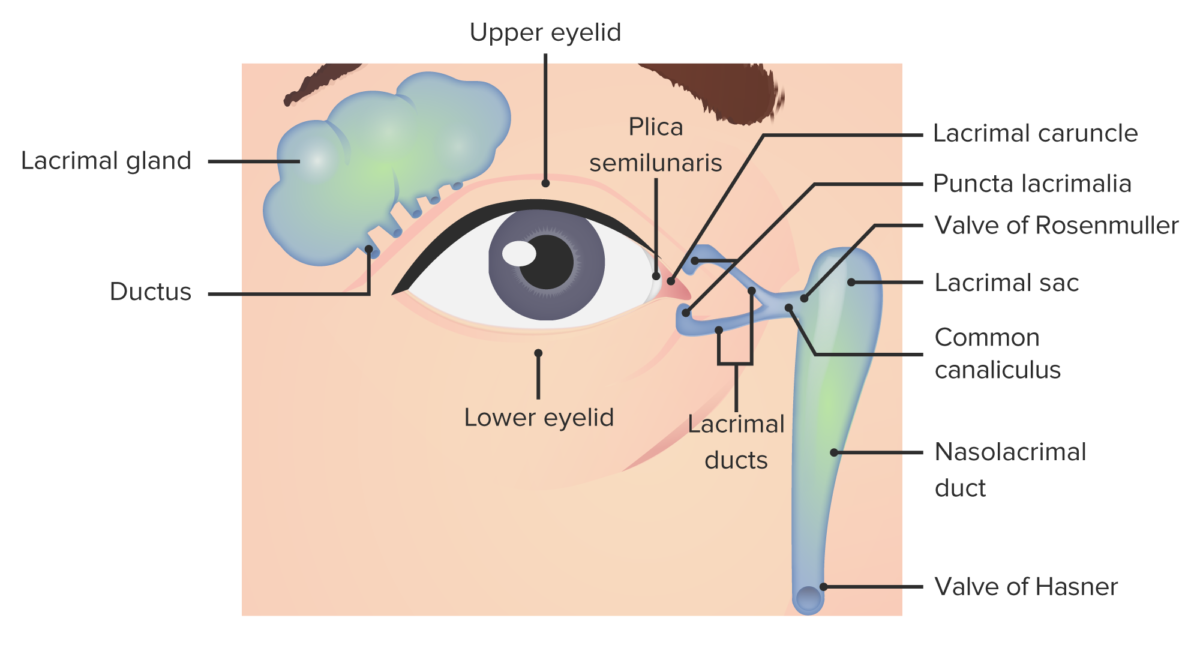
Lacrimal apparatus anatomy
Image by Lecturio.Nasolacrimal system obstruction is the main etiology.
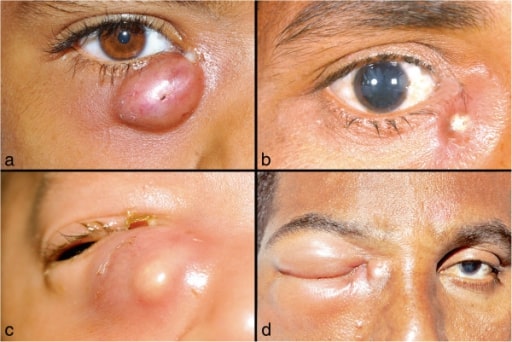
Images of lacrimal abscess:
a. and b. Localized right lacrimal abscess, with discharge at the medial canthus;
c. a neonate with right lacrimal abscess;
d. Lacrimal abscess with orbital cellulitis

Left orbital cellulitis:
Photograph shows left upper and lower eyelid edema and erythema with conjunctival chemosis.
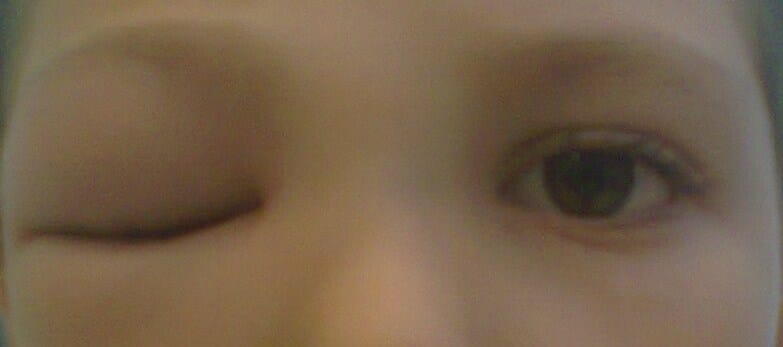
Right preseptal cellulitis:
Image shows marked, isolated, unilateral periocular inflammation. The individual presented with painless eye movement.
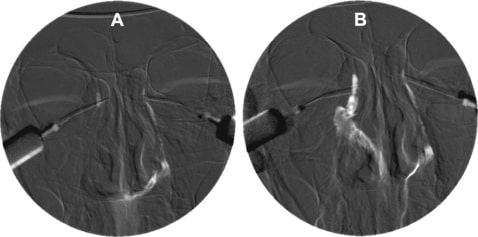
Digital subtraction dacryocystogram.
A. Completely obstructed right NLD showing no flow of contrast medium. Normal left NLD
B. Free flow of the contrast medium through the recanalized right NLD to the inferior meatus after surgery
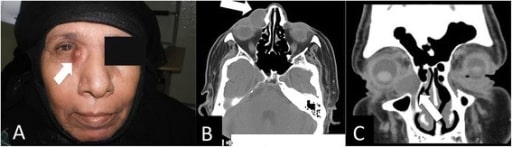
A. Clinical photo of a patient with right eye dacryocele
B. CT axial cut showing the medial canthus dacryocele (white arrow)
C. CT coronal cut showing the same finding (white arrow)