Gastrointestinal bleeding indicates underlying pathology in either the upper or lower gastrointestinal (GI) tract. Hematemesis (vomiting red blood or “coffee-ground” material) and melena (black, tarry stool) usually indicate upper GI bleeding proximal to the suspensory ligament of the duodenum, also called the ligament of Treitz. Peptic ulcer disease (PUD) is the most common cause of upper GI bleeding. Hematochezia (red blood in the stool) is most often associated with lower GI bleeding (although it infrequently occurs with massive upper GI bleeding that is typically associated with hypotension). Lower GI bleeding can be from diverticular disease, angiodysplasia, polyps or tumors, inflammatory bowel disease, or internal hemorrhoids. Diagnosis is made by clinical history and physical exam, followed by upper and/or lower GI endoscopy. The source of the bleeding can usually be identified and treated with endoscopy.
Last updated: May 17, 2024
Upper gastrointestinal bleed (proximal to the ligament of Treitz):
Lower GIB (distal to the ligament of Treitz):

Thrombosed external hemorrhoid with prolapsing internal hemorrhoid
Image: “Circular perianal thrombosis” by Rohde et al; licensee BioMed Central Ltd.. License: CC BY 2.0Diagnosis and management of GIB tend to go hand-in-hand and will vary depending on the hemodynamic stability of the patient.
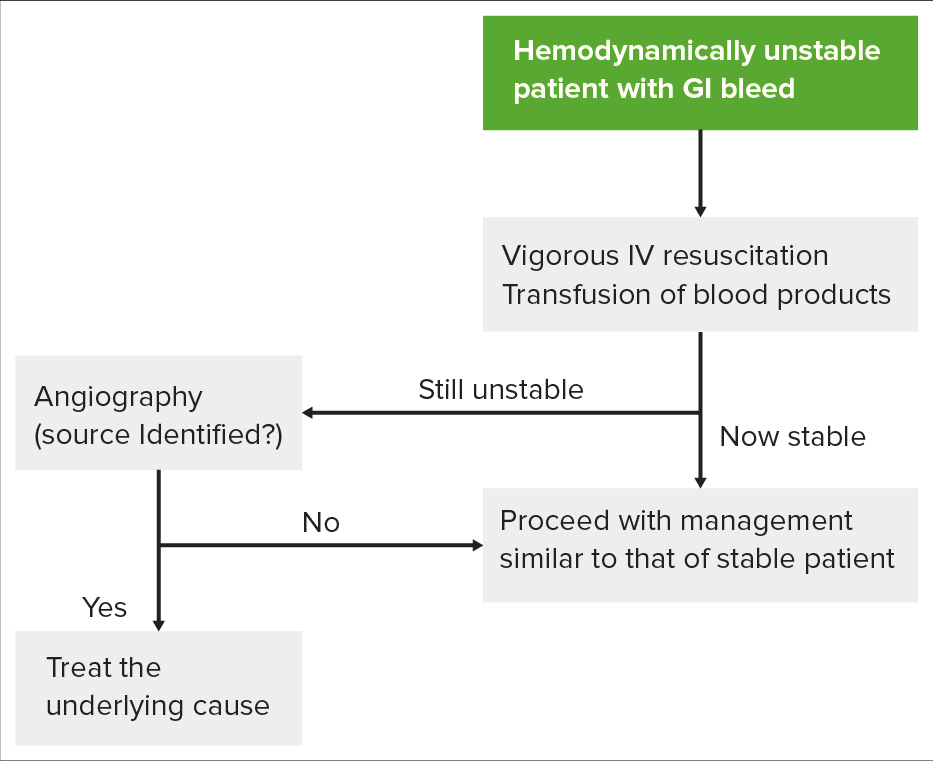
Algorithm for evaluating a hemodynamically unstable patient: The first step requires attempting to stabilize the patient before pursuing workup. The patient’s response will then determine whether the patient should go straight to angiography for diagnosis and treatment, or endoscopy.
Image by Lecturio.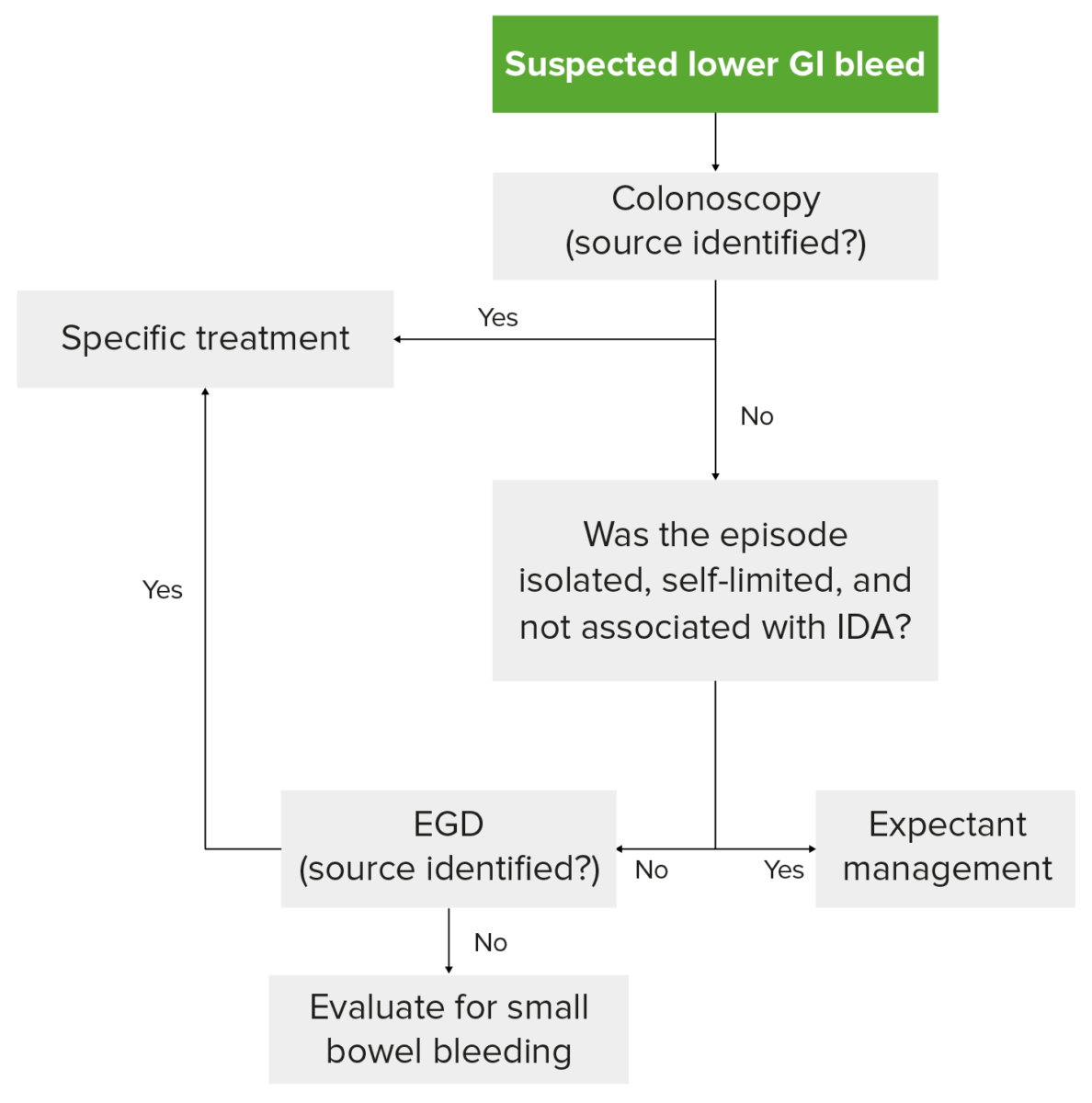
Diagnostic algorithm for LGIB in a hemodynamically stable patient: Colonoscopy is the preferred 1st step. If colonoscopy is unremarkable, the bleed has ceased and not recurred, and the patient does not have iron deficiency anemia (IDA), then expectant management is pursued.
Image by Lecturio.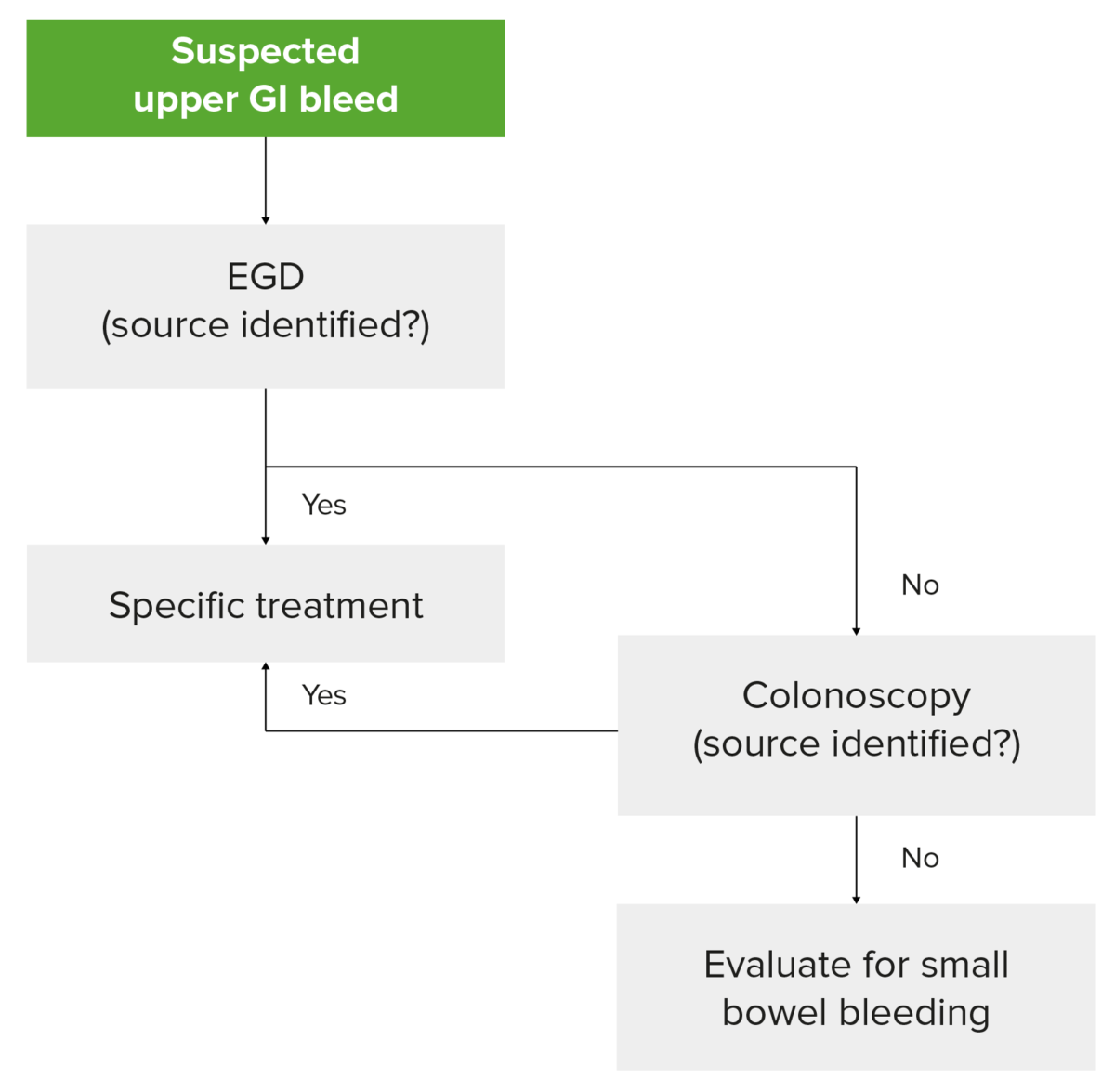
Diagnostic algorithm for UGIB in a hemodynamically stable patient: Notice that capsule endoscopy to evaluate the small bowel should be considered if EGD and colonoscopy do not reveal a source.
Image by Lecturio.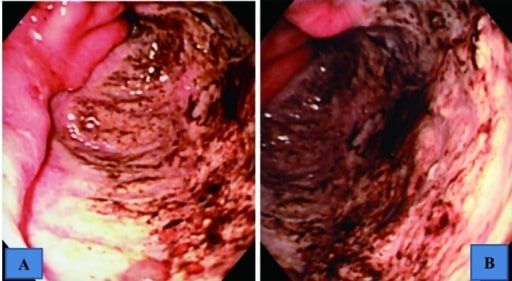
Upper GI endoscopic findings showing a giant ulcer in the greater curvature of the antrum, which occupied halfway around the lumen
A: intermediate view
B: near view

Endoscopic picture obtained from an 83-year-old woman showing the site of angiodysplasia between the 1st and the 2nd portion of the duodenum
Image: “Angiodysplasia” by Department of Cardiology, San Raffaele Hospital, Via Olgettina 60, 20131 Milan, Italy. License: CC BY 3.0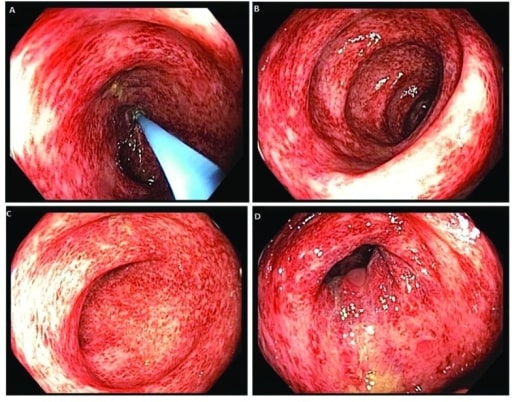
Colonoscopy images revealing patchy and diffuse colitis throughout the colon
Image: “ Colonoscopy” by US National Library of Medicine. License: CC BY 2.0Assess the patient’s hemodynamics Hemodynamics The movement and the forces involved in the movement of the blood through the cardiovascular system. Vascular Resistance, Flow, and Mean Arterial Pressure and stabilize: