Rashes are a group of diseases that cause abnormal coloration and texture Texture Dermatologic Examination to the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. The etiologies are numerous but can include irritation, allergens, infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, or inflammatory conditions. Rashes that present in only 1 area of the body are called localized rashes. Generalized rashes occur diffusely throughout the body. Rashes can be classified by their distribution, configuration, and morphology. The diagnosis is often clinical and based on the patient’s history and physical exam findings. Management is dependent on identifying the correct condition and varies depending on the etiology.
Last updated: Jun 15, 2025
A rash Rash Rocky Mountain Spotted Fever is an abnormal change in the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions’s color or texture Texture Dermatologic Examination.
The list of etiologies for rashes is long but can include irritants, allergens, infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, and inflammatory conditions.
Rashes are described and classified based on certain characteristics, which can assist with forming a differential diagnosis when evaluating a patient.
The configuration refers to the shape or outline of lesions.
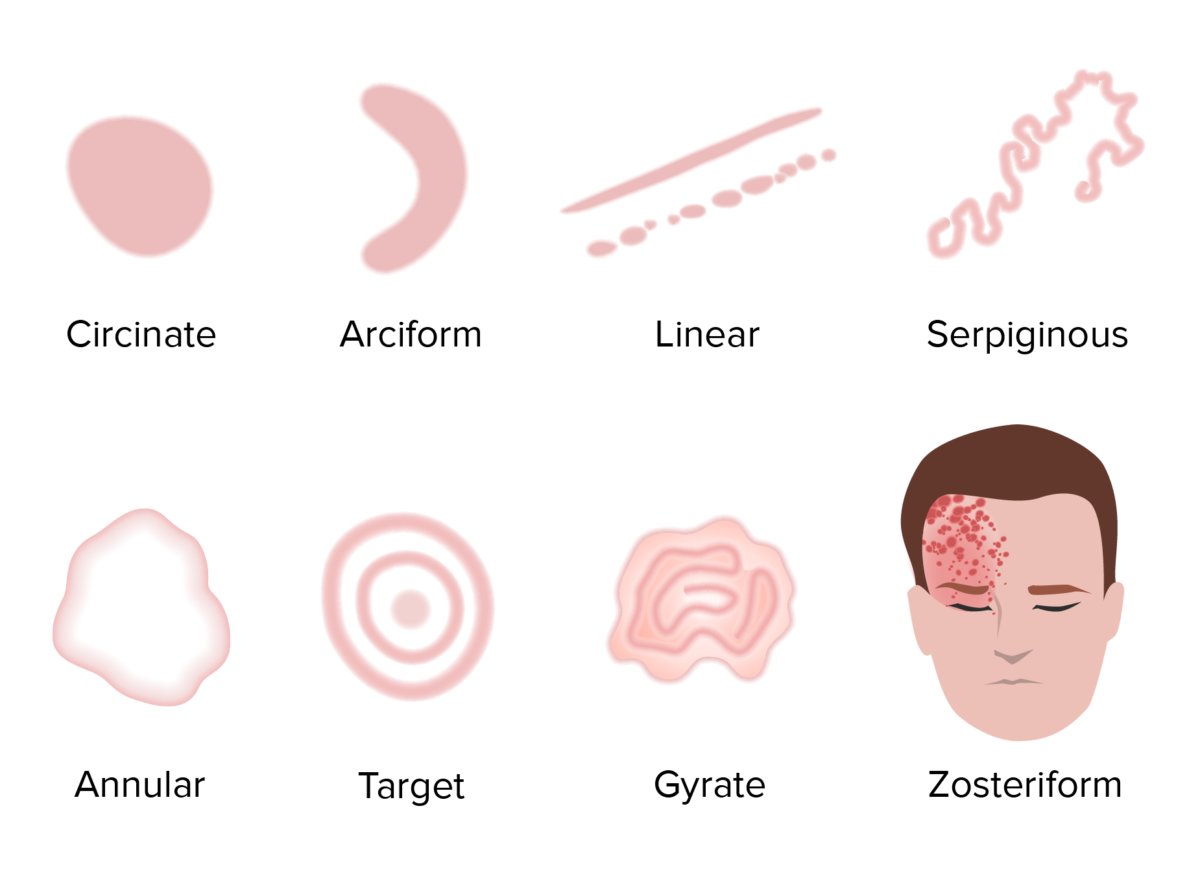
Visualization of different rash configurations
Image by Lecturio.The morphology is based on the size and consistency Consistency Dermatologic Examination of the lesions.
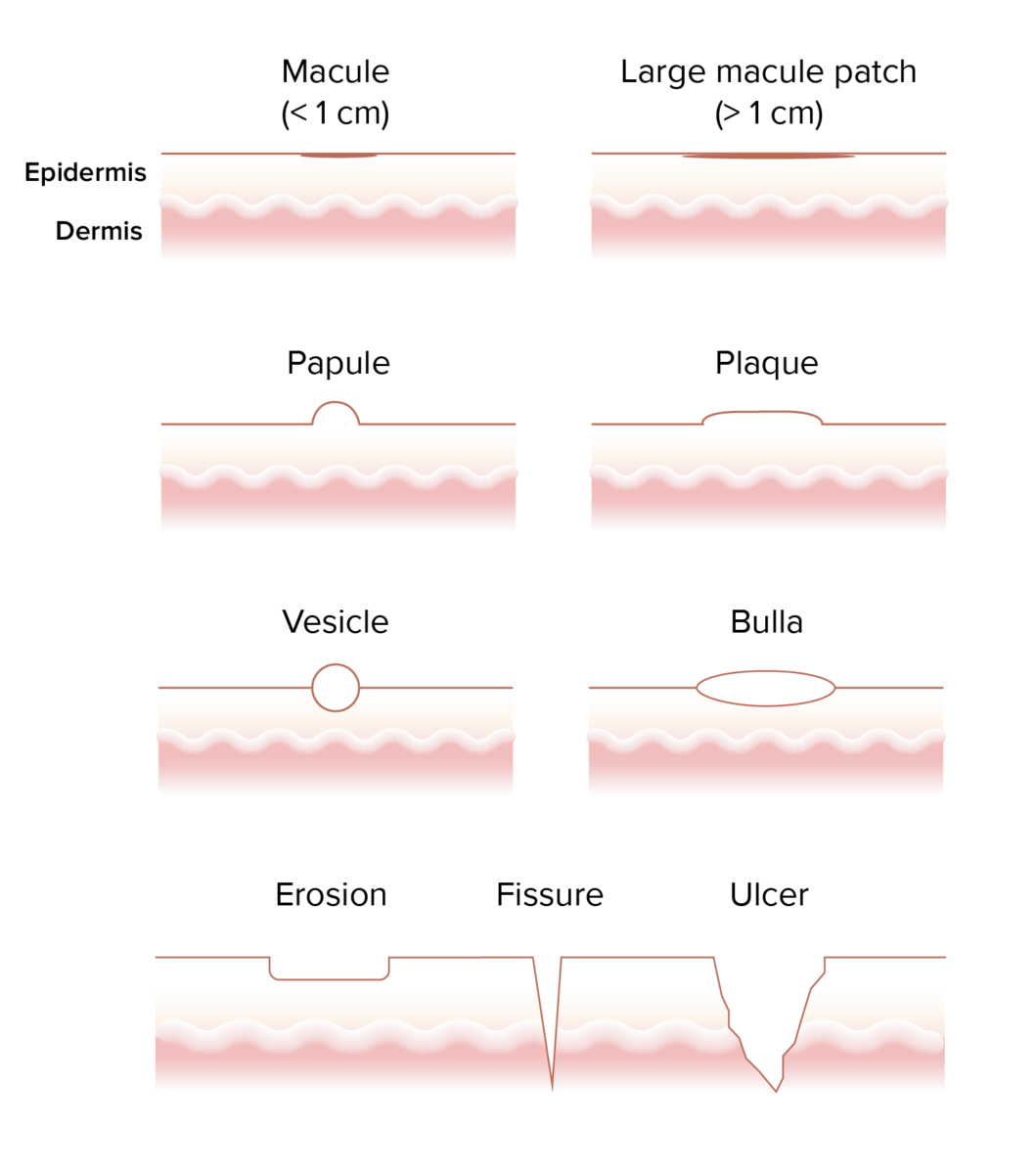
Visualization of different rash morphologies
Image by Lecturio.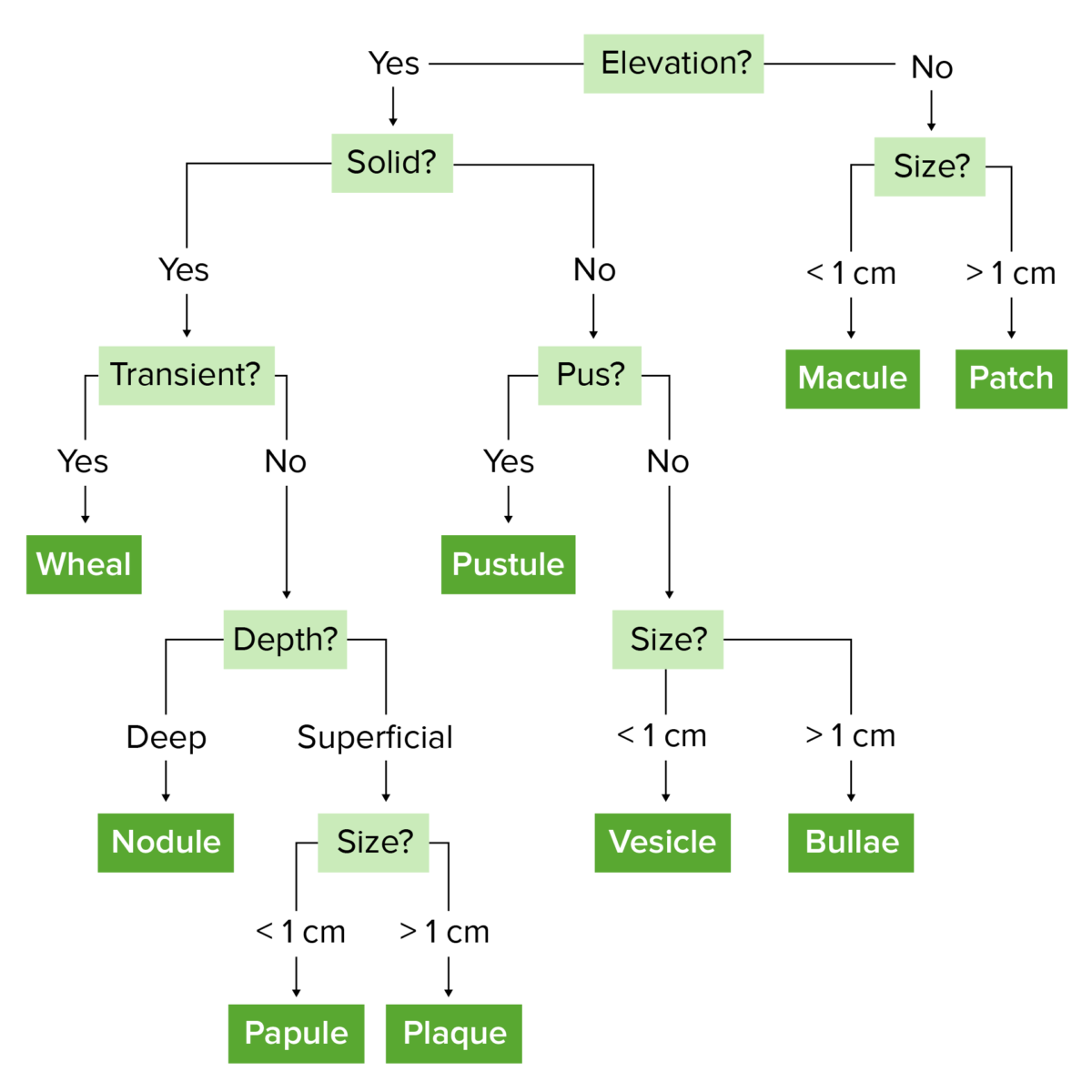
Schematic to help differentiate different morphologies based on their size and characteristics
Image by Lecturio.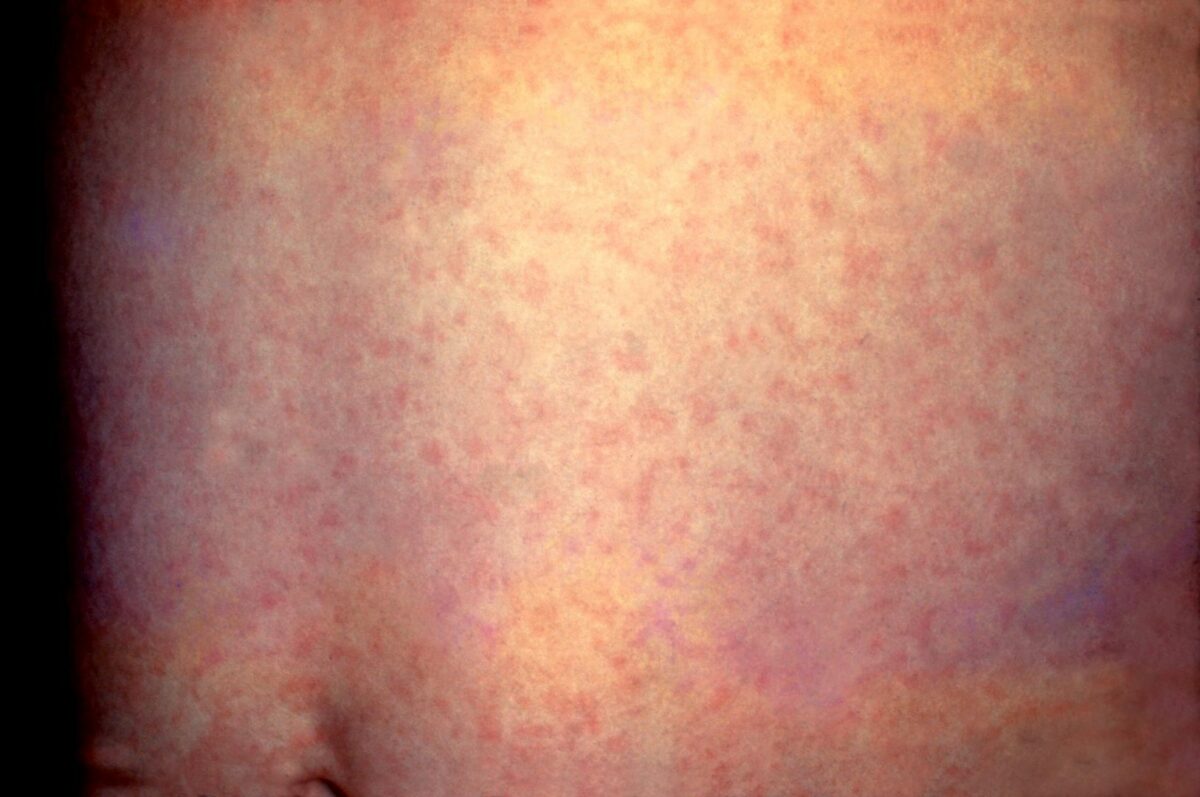
Small, flat macules due to rubella
Image: “Rubella” by CDC. License: Public Domain
Large patches of hypopigmentation in vitiligo
Image: “Split thickness skin grafting in patients with stable vitiligo” by Sameem F, Sultan SJ, Ahmad QM. License: CC BY 2.0
Multiple skin papules on the hands
Image: “Generalized lichen nitidus in childhood” by Mehta V, Balachandran C. License: CC BY 2.0
Skin plaques from psoriasis
Image: “Pulmonary sarcoidosis associated with psoriasis vulgaris: coincidental occurrence or causal association? Case report” by Nikolopoulou M, Katsenos S, Psathakis K, Rallis E, Sampaziotis D, Panagou P, Tsintiris K, Bouros D. License: CC BY 2.0
A large skin nodule
Image: “Ovarian carcinoma presenting as cutaneous nasal metastasis” by Anais Brasileiros de Dermatologia. License: CC BY 4.0
Multiple vesicles on the neck due to shingles
Image: “Herpes Zoster am Hals” by M.S. License: Public Domain
Several wheals due to skin testing for allergies
Image: “Autologous serum skin test in children” by Godse KV. License: CC BY 2.0
Picture of multiple pustules (pus-filled blisters)
Image: “A rare presentation of pemphigus vulgaris as multiple pustules” by Yang Y, Lin M, Huang SJ, Min C, Liao WQ. License: CC BY 2.0
Tense bulla on the dorsum of the 2nd toe and a larger collapsed bulla on the ball of the great toe
Image: “Bullosis diabeticorum: A distinctive blistering eruption in diabetes mellitus” by Ghosh SK, Bandyopadhyay D, Chatterjee G. License: CC BY 2.0
An overlying crust
Image: “Diabetic dermopathy (“shin spots”) and diabetic bullae (“bullosis diabeticorum”) at the same patient” by Brzezinski P, Chiriac AE, Pinteala T, Foia L, Chiriac A. License: CCC BY 3.0
Scale on a herald patch of pityriasis rosea
Image: “Pityriasis rosea” by CDC. License: Public Domain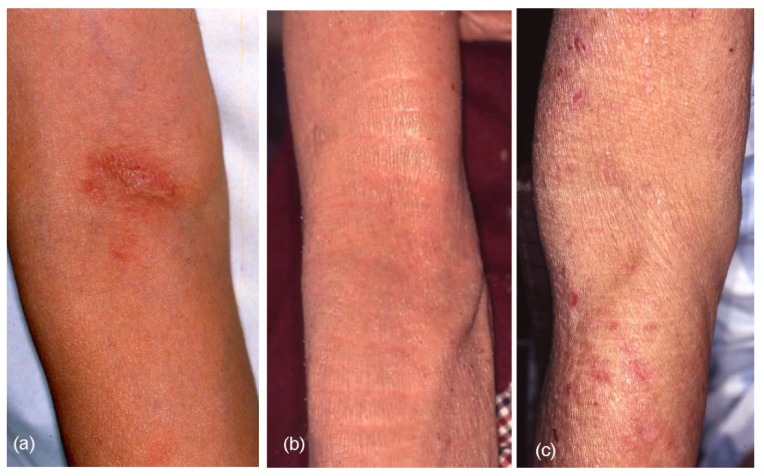
Thick, leathery skin (lichenification) due to eczema
Image: “Clinical Characteristics, Treatments, and Prognosis of Atopic Eczema in the Elderly” by Tanei R. License: CC BY 4.0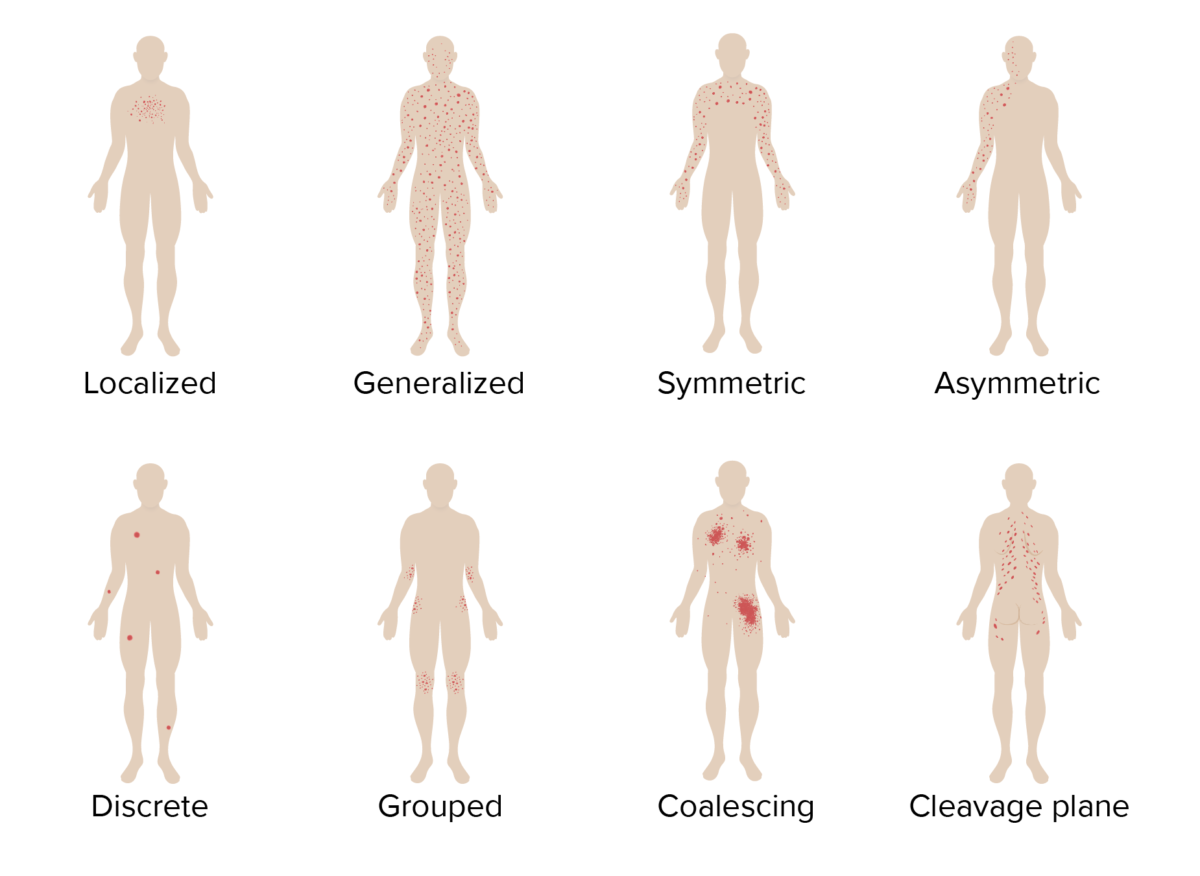
Visualization of different rash distributions
Image by Lecturio.The diagnosis for many conditions is purely clinical and based on the patient’s history and physical exam.
| Patient’s history | Associated disease |
|---|---|
| Chronic illness |
|
| Contact with ill persons |
|
| Drug exposure |
|
| Occupational or environmental exposure | Contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination |
| Insect and arthropod exposure |
|
| Recent systemic symptoms |
|
| Sexual history |
|
| Travel |
|
A full skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions exam should be performed.
A diagnostic workup may be performed if the history and physical exam do not provide enough clues to the diagnosis. The differential diagnosis will dictate which studies should be performed.
The management of a rash Rash Rocky Mountain Spotted Fever depends on the underlying condition. Many rashes will be self-limited and may not require any treatment.
| Condition | Features | Diagnosis | Management |
|---|---|---|---|
| Atopic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) ( eczema Eczema Atopic dermatitis, also known as eczema, is a chronic, relapsing, pruritic, inflammatory skin disease that occurs more frequently in children, although adults can also be affected. The condition is often associated with elevated serum levels of IgE and a personal or family history of atopy. Skin dryness, erythema, oozing, crusting, and lichenification are present. Atopic Dermatitis (Eczema)) |
|
|
|
| Drug eruption |
|
|
|
| Pityriasis rosea Pityriasis rosea Pityriasis rosea is an acute, self-limited skin disease. The etiology is not known, and it commonly occurs in young adults. Patients initially present with a single, ovoid “herald patch.” This is followed by diffuse, pruritic, scaly, oval lesions over the trunk (often in a “Christmas tree” distribution on the back) and extremities. Pityriasis Rosea |
|
Clinical diagnosis |
|
| Lichen planus Lichen planus Lichen planus (LP) is an idiopathic, cell-mediated inflammatory skin disease. It is characterized by pruritic, flat-topped, papular, purple skin lesions commonly found on the flexural surfaces of the extremities. Other areas affected include genitalia, nails, scalp, and mucous membranes. Lichen Planus |
|
|
Topical steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors |
| Psoriasis Psoriasis Psoriasis is a common T-cell-mediated inflammatory skin condition. The etiology is unknown, but is thought to be due to genetic inheritance and environmental triggers. There are 4 major subtypes, with the most common form being chronic plaque psoriasis. Psoriasis |
|
|
Local therapy:
|

Erythema and lichenification in the kneefolds of a patient with atopic dermatitis
Image: “Role of the skin microbiome in atopic dermatitis” by Salava A, Lauerma A. License: CC BY 4.0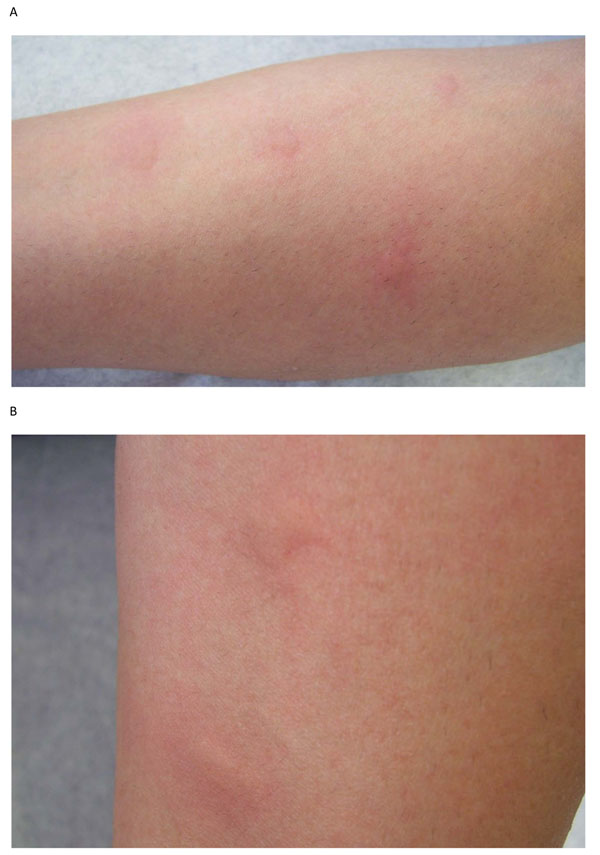
Edematous wheals suggestive of urticaria. This can be a manifestation of a drug eruption.
Image: “Urticaria and angioedema” by Kanani A, Schellenberg R, Warrington R. License: CC BY 2.0
Target lesions of erythema multiforme, which may be a manifestation of a drug eruption
Image: “Erythema multiforme as first sign of incomplete Kawasaki disease” by Vierucci F, Tuoni C, Moscuzza F, Saggese G, Consolini R. License: CC BY 2.0, edited by Lecturio.
Drug-induced toxic epidermal necrolysis with peeled skin over the back and buttocks
Image: “Drug induced toxic epidermal necrolysis: two case reports.” by Qadir SN, Raza N, Qadir F. License: CC BY 3.0
The secondary, generalized eruption of pityriasis rosea:
Multiple small, pink lesions are seen. Their oblique positioning is due to their orientation along Langer’s lines. In some patients, this can give a “Christmas tree” appearance.

Lichen planus located on the upper thigh. Notice the common characteristics of these lesions: polygonal in shape, purple/violaceous in color, and planar. Primary lesions are often a few millimeters in size but can coalesce in larger plaques and are often pruritic.
Image: “12188” by CDC/ Wallace N. McLeod, M.D.; Bob Craig. License: Public Domain
Psoriatic lesion on the knee
Image: “Myelin-associated glycoprotein-related neuropathy associated with psoriasis: a case report” by Murata KY, Miwa H, Kondo T. License: CC BY 2.0| Condition | Features | Diagnosis | Management |
|---|---|---|---|
| Hand-foot-and-mouth disease |
|
Clinical diagnosis | Symptomatic treatment |
| Roseola infantum Roseola infantum An acute, short-lived, viral disease of infants and young children characterized by a high fever at onset that drops to normal after 3-4 days and the concomitant appearance of a macular or maculopapular rash that appears first on the trunk and then spreads to other areas. It is the sixth of the classical exanthematous diseases and is caused by HHV-6. Human Herpesvirus 6 and 7 ( exanthem Exanthem Diseases in which skin eruptions or rashes are a prominent manifestation. Classically, six such diseases were described with similar rashes; they were numbered in the order in which they were reported. Only the fourth (Duke’s disease), fifth (erythema infectiosum), and sixth (exanthema subitum) numeric designations survive as occasional synonyms in current terminology. Varicella-Zoster Virus/Chickenpox subitum) |
|
Clinical diagnosis | Symptomatic treatment |
| Measles Measles Measles (also known as rubeola) is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. It is highly contagious and spreads by respiratory droplets or direct-contact transmission from an infected person. Typically a disease of childhood, measles classically starts with cough, coryza, and conjunctivitis, followed by a maculopapular rash. Measles Virus ( rubeola Rubeola Measles (also known as rubeola) is caused by a single-stranded, linear, negative-sense RNA virus of the family Paramyxoviridae. It is highly contagious and spreads by respiratory droplets or direct-contact transmission from an infected person. Typically a disease of childhood, measles classically starts with cough, coryza, and conjunctivitis, followed by a maculopapular rash. Measles Virus) |
|
Clinical diagnosis | Symptomatic treatment |
| Rubella Rubella An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus ( German measles German measles An acute infectious disease caused by the rubella virus. The virus enters the respiratory tract via airborne droplet and spreads to the lymphatic system. Rubella Virus) |
|
|
Symptomatic treatment |
| 5th disease ( erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion infectiosum) |
|
|
Symptomatic treatment |
| Scarlet fever Scarlet fever Infection with group a Streptococci that is characterized by tonsillitis and pharyngitis. An erythematous rash is commonly present. Scarlet Fever |
|
|
|
| Chickenpox Chickenpox A highly contagious infectious disease caused by the varicella-zoster virus. It usually affects children, is spread by direct contact or respiratory route via droplet nuclei, and is characterized by the appearance on the skin and mucous membranes of successive crops of typical pruritic vesicular lesions that are easily broken and become scabbed. Chickenpox is relatively benign in children, but may be complicated by pneumonia and encephalitis in adults. Varicella-Zoster Virus/Chickenpox |
|
|
|

Painful vesicles on a hand (A) and foot (B) due to hand-foot-and-mouth disease
Image: “Hand, foot and mouth disease: changing Indian scenario” by Rao PK, Veena K, Jagadishchandra H, Bhat SS, Shetty SR. License: CC BY 3.0, edited by Lecturio.
Diffuse maculopapular rash on the chest and abdomen due to roseola infantum
Image: “Sestamalattia” by Emiliano Burzagli. License: Public Domain
Maculopapular rash on the face of a child with measles
Image: “Measles child Philippines” by Jim Goodson. License: Public Domain
Macular rash of rubella on the skin of a child’s back
Image: “ଫାଇଲ:Rash of rubella on back (crop)” by CDC. License: Public Domain
Pediatric patient with 5th disease: erythematous facial rash accompanied by rash on the torso and extremities
Image: “Fifth disease” by Andrew Kerr. License: Public Domain
Face looks flushed but with “white mustache” or circumoral pallor, typical of scarlet fever.
Image: “Slapped cheeks and white mustache” by Estreya. License: CC BY-SA 4.0
Diffuse vesicles on a red base due to chickenpox
Image: “21501” by K.L. Herrmann. License: Public Domain| Condition | Features | Diagnosis | Management |
|---|---|---|---|
| Contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination |
|
|
|
| Tinea corporis Tinea corporis Dermatophytes/Tinea Infections |
|
|
Topical or oral antifungals |
| Seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) |
|
|
|
| Impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts. Impetigo |
|
|
|
| Cellulitis Cellulitis Cellulitis is a common infection caused by bacteria that affects the dermis and subcutaneous tissue of the skin. It is frequently caused by Staphylococcus aureus and Streptococcus pyogenes. The skin infection presents as an erythematous and edematous area with warmth and tenderness. Cellulitis |
|
|
|
| Erysipelas Erysipelas Erysipelas is a bacterial infection of the superficial layer of the skin extending to the skin’s superficial lymphatic vessels. This infection presents as a raised, well-defined, tender, and bright red rash. Typically on the legs or face, but erysipelas can occur anywhere on the skin. Erysipelas |
|
|
|
| Necrotizing fasciitis Necrotizing fasciitis Necrotizing fasciitis is a life-threatening infection that causes rapid destruction and necrosis of the fascia and subcutaneous tissues. Patients may present with significant pain out of proportion to the presenting symptoms and rapidly progressive erythema of the affected area. Necrotizing Fasciitis |
|
|
|
| Herpes zoster Herpes Zoster Varicella-zoster virus (VZV) is a linear, double-stranded DNA virus in the Herpesviridae family. Shingles (also known as herpes zoster) is more common in adults and occurs due to the reactivation of VZV. Varicella-Zoster Virus/Chickenpox ( shingles Shingles Varicella-zoster virus (VZV) is a linear, double-stranded DNA virus in the Herpesviridae family. Shingles (also known as herpes zoster) is more common in adults and occurs due to the reactivation of VZV. Varicella-Zoster Virus/Chickenpox) |
|
|
|

A pruritic, vesicular eruption due to contact dermatitis
Image: “Neoprene Orthopaedic Supports: An Underrecognised Cause of Allergic Contact Dermatitis” by Hawkey S, Ghaffar S. License: CC BY 3.0
Annular, scaling lesion of tinea corporis
Image: “Ringworm on the arm, or tinea corporis due to Trichophyton mentagrophytes PHIL 2938 lores” by /Dr. Lucille K.. License: Public Domain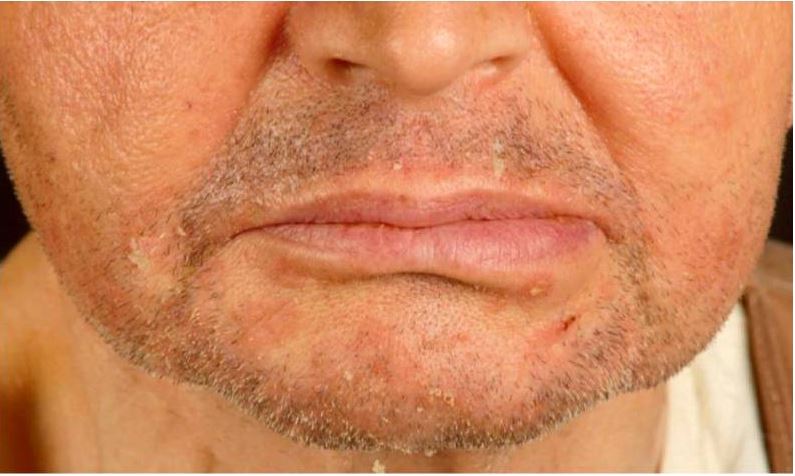
Seborrheic dermatitis in a renal transplant recipient.
Note the erythematous scaly papules on the chin and nasolabial folds.

Crusted, non-bullous impetigo on the upper extremity of a pediatric patient
Image: “Diagnosis of Atopic Dermatitis: Mimics, Overlaps, and Complications” by Siegfried EC, Hebert AA. License: CC BY 4.0
Photograph showing marked pitting edema and erythema with poorly demarcated borders due to cellulitis
Image: “How 40 kilograms of fluid retention can be overlooked: two case reports” by Ong HS, Sze CW, Koh TW, Coppack SW. License: CC BY 2.0
Facial erysipelas presenting as an erythematous and edematous plaque covering the cheeks and nose with the presence of excoriations and vesicles.
Compared with cellulitis, this rash is well demarcated with raised borders.

Cutaneous necrosis, erythema, and bullous changes due to necrotizing fasciitis of the leg
Image: “Necrotizing fasciitis left leg” by Piotr Smuszkiewicz, Iwona Trojanowska and Hanna Tomczak. License: CC BY 2.0
Vesicular eruption involving the V3 dermatome in shingles
Image: “Facial herpes zoster infection precipitated by surgical manipulation of the trigeminal nerve during exploration of the posterior fossa: a case report” by Mansour N, Kaliaperumal C, Choudhari KA. License: CC BY 3.0