The membrane attack complex Membrane attack complex A product of complement activation cascade, regardless of the pathways, that forms transmembrane channels causing disruption of the target cell membrane and cell lysis. It is formed by the sequential assembly of terminal complement components (complement C5b; complement C6; complement C7; complement C8; and complement C9) into the target membrane. The resultant C5b-8-poly-c9 is the 'membrane attack complex' or MAC. Type II Hypersensitivity Reaction (MAC), which is formed by complement proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis, plays a crucial role in the eradication of bacterial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, especially Neisseria Neisseria Neisseria is a genus of bacteria commonly present on mucosal surfaces. Several species exist, but only 2 are pathogenic to humans: N. gonorrhoeae and N. meningitidis. Neisseria species are non-motile, gram-negative diplococci most commonly isolated on modified Thayer-Martin (MTM) agar. Neisseria species and other encapsulated Encapsulated Klebsiella bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology, by attaching to the bacterial plasma membrane Plasma membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane and forming pores that eventually lead to cell lysis. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with terminal complement pathway deficiency may present with recurrent and severe neisserial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease as they are unable to synthesize MAC because of a deficiency in one of its components (e.g., late complement proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis). Treatment is antibiotics for the infection and vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination against encapsulated Encapsulated Klebsiella bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology.
Last updated: Sep 19, 2022
Membrane attack complex Membrane attack complex A product of complement activation cascade, regardless of the pathways, that forms transmembrane channels causing disruption of the target cell membrane and cell lysis. It is formed by the sequential assembly of terminal complement components (complement C5b; complement C6; complement C7; complement C8; and complement C9) into the target membrane. The resultant C5b-8-poly-c9 is the ‘membrane attack complex’ or MAC. Type II Hypersensitivity Reaction (MAC) structure and function:
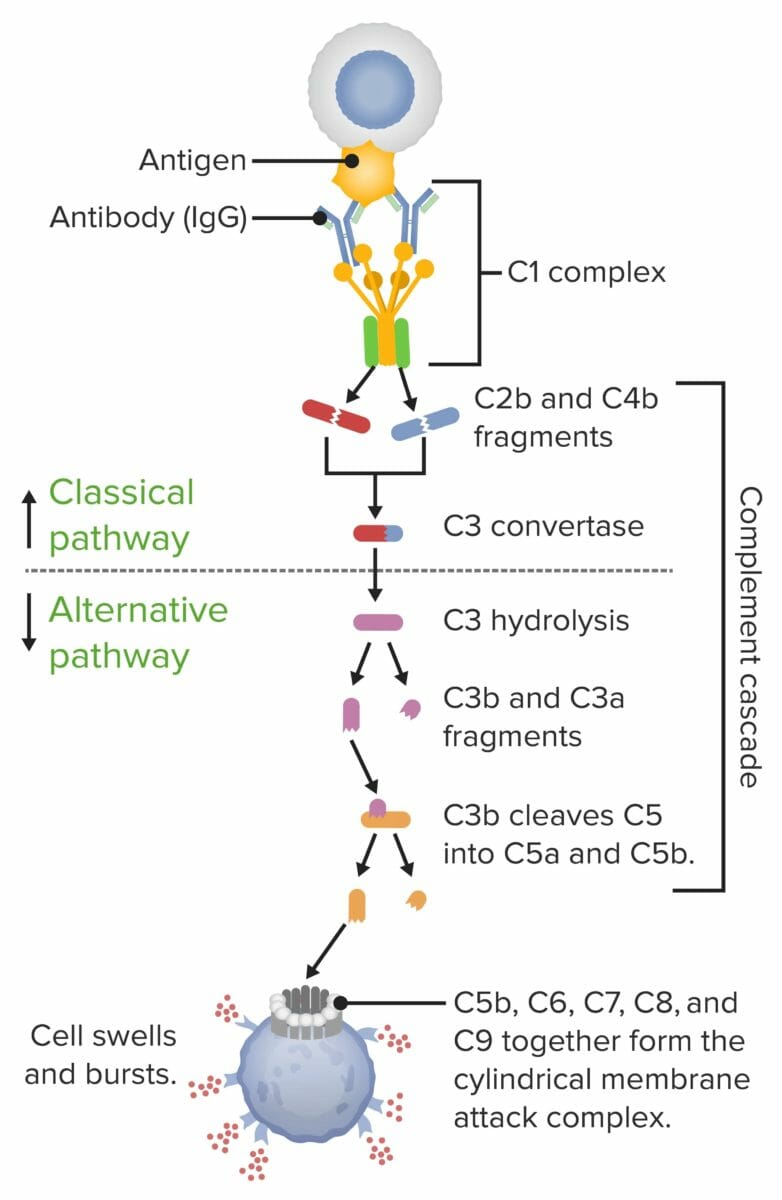
Membrane attack complex (MAC) formation:
When the 1st protein in the complement series is activated (typically by an antibody locked onto an antigen), a domino effect is set into motion. Each component takes a turn in a precise chain of steps known as the complement cascade. The end product is the cylindrical MAC, which inserts into and punctures a hole in the cell’s wall. With fluids and molecules flowing in and out, the cell swells and bursts.
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic.
Symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with:
Total complement activity (CH50) is used for screening Screening Preoperative Care. If CH50 is low/undetectable, measurement of the serum protein level for complement proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis should be ordered. Findings include: