Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli Bacilli Shigella. They form pink colonies on MacConkey agar MacConkey agar Yersinia spp./Yersiniosis due to lactose fermentation. The main virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus factor is a polysaccharide capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides. Klebsiella pneumoniae Klebsiella Pneumoniae Gram-negative, non-motile, capsulated, gas-producing rods found widely in nature and associated with urinary and respiratory infections in humans. Aminoglycosides (the most important pathogenic species) is commonly associated with lobar aspiration pneumonia Aspiration pneumonia A type of lung inflammation resulting from the aspiration of food, liquid, or gastric contents into the upper respiratory tract. Pneumonia in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with alcohol-use disorder. It also causes nosocomial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, such as hospital-acquired pneumonia Hospital-Acquired Pneumonia Pneumonia in Children and urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, as well as tissue-destructing abscesses ( liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, lung, spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy). Treatment is with cephalosporins Cephalosporins Cephalosporins are a group of bactericidal beta-lactam antibiotics (similar to penicillins) that exert their effects by preventing bacteria from producing their cell walls, ultimately leading to cell death. Cephalosporins are categorized by generation and all drug names begin with "cef-" or "ceph-." Cephalosporins for sensitive strains. However, many Klebsiella species have plasmids Plasmids Extrachromosomal, usually circular DNA molecules that are self-replicating and transferable from one organism to another. They are found in a variety of bacterial, archaeal, fungal, algal, and plant species. They are used in genetic engineering as cloning vectors. DNA Types and Structure that confer multidrug resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing.
Last updated: Jan 26, 2025
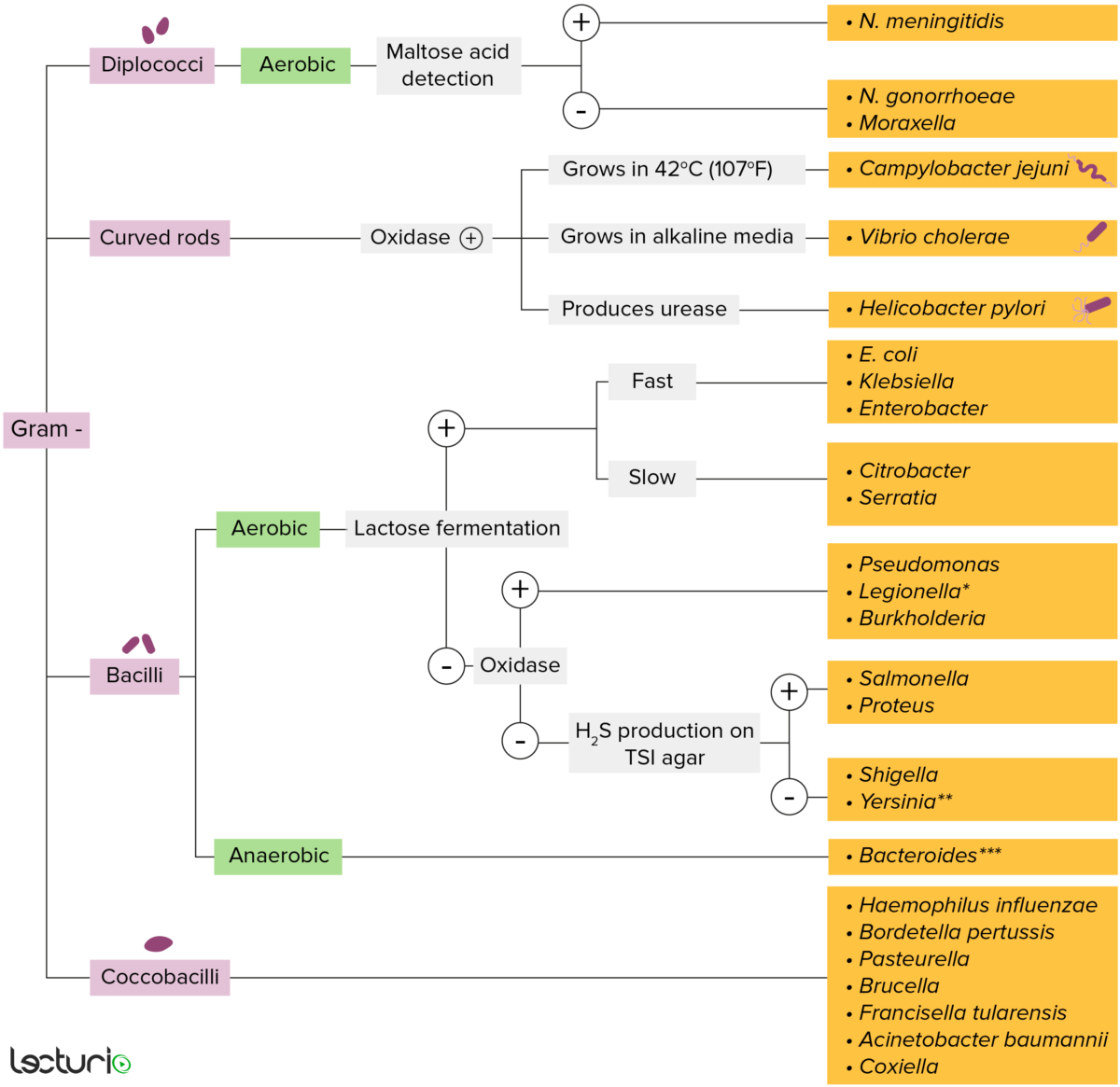
Gram-negative bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thin layer of peptidoglycan do not retain the crystal violet stain utilized in Gram staining. These bacteria do, however, retain the safranin counterstain and thus appear as pinkish-red on the stain, making them gram negative. These bacteria can be further classified according to morphology (diplococci, curved rods, bacilli, and coccobacilli) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The bacteria can be more narrowly identified by growing them on specific media (triple sugar iron (TSI) agar) where their enzymes can be identified (urease, oxidase) and their ability to ferment lactose can be tested.
* Stains poorly on Gram stain
** Pleomorphic rod/coccobacillus
*** Require special transport media

Klebsiella pneumoniae: Scanning electron micrograph of Carbapenem-resistant K. pneumoniae interacting with a human neutrophil
Image: “Klebsiella pneumoniae bacterium” by NIAID. License: CC BY 2.0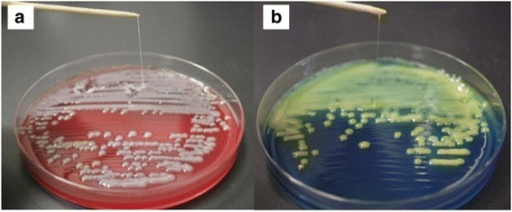
Klebsiella mucoid colonies forming a string of > 5 mm in length in sheep blood agar (a) and in bromothymol blue lactose agar (b)
Image: “Invasive liver abscess syndrome caused by Klebsiella pneumoniae with definite K2 serotyping in Japan: a case report” by Seo R, Kudo D, Gu Y, Yano H, Aoyagi T, Omura T, Irino S, Kaku M, Kushimoto S. License: CC BY 4.0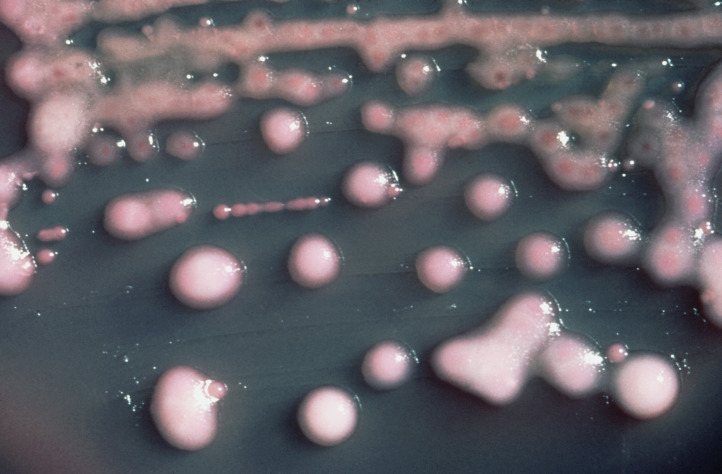
K. pneumoniae forming pink colonies on MacConkey agar
Image: “Klebsiella pneumoniae 01” by CDC. License: Public DomainPneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia:
Urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease (UTIs):
Catheter-related bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides:
Less frequent infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:
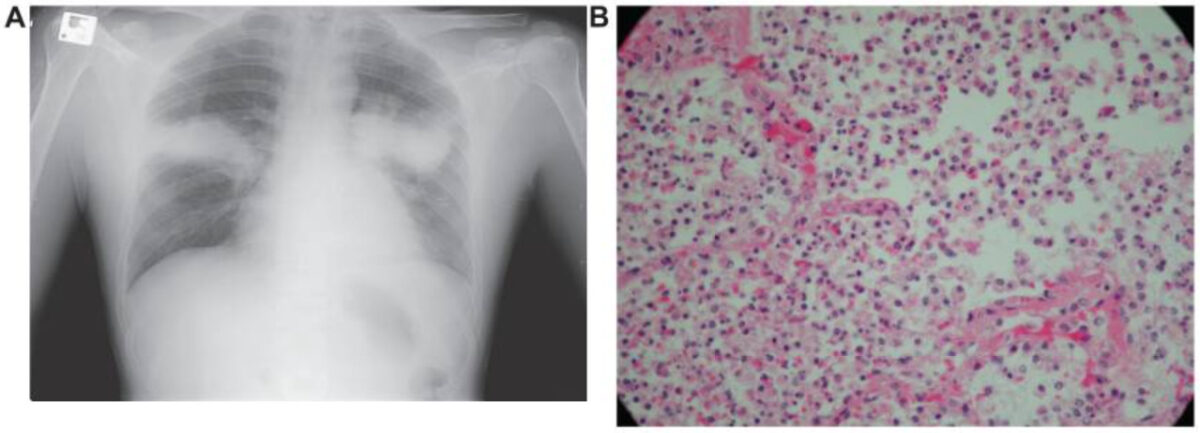
Radiological (A) and pathological (B) representation of Klebsiella pneumoniae: prominent voluminous hyperdense, symmetric bilateral lung consolidation, and the massive infiltration of neutrophils in the interstitium and intra-alveolar spaces
Image: “Fulminant Klebsiella pneumoniae pneumonia in an immunocompetent patient without alcohol-use disorder” by Benyashvili Z, Djirbe A, Assy N. License: CC BY 3.0To help remember the clinical manifestations of Klebsiella, remember “the 5 As of KlebsiellA:”
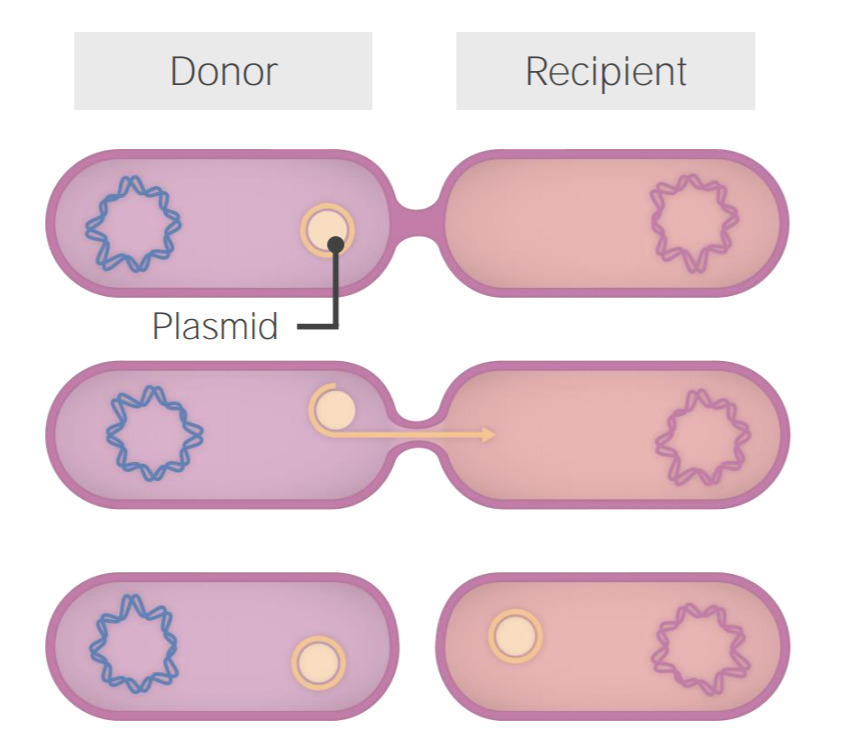
Plasmid exchange in Klebsiella
A pilus allows for the exchange of replicated plasmid between 2 cells. As soon as the pilus is formed, the plasmid is replicated and then transferred through the pilus from the donor into the recipient cell.