The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy at the level of the 9th‒11th ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy just below the diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology. The spleen can also activate immune responses, produce antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, and function as a reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli for platelet storage. There are 2 primary types of splenic tissue: red pulp Red pulp Secondary Lymphatic Organs, which contains dense fibrovascular networks for filtering the blood, and white pulp White pulp Secondary Lymphatic Organs, which is primarily made up of lymphoid tissue surrounding the larger vessels. The spleen has a relatively weak capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides; thus, it can rupture more easily than other abdominal organs and lead to life-threatening hemorrhage.
Last updated: Mar 31, 2025
The spleen is the largest lymphatic organ in the body.
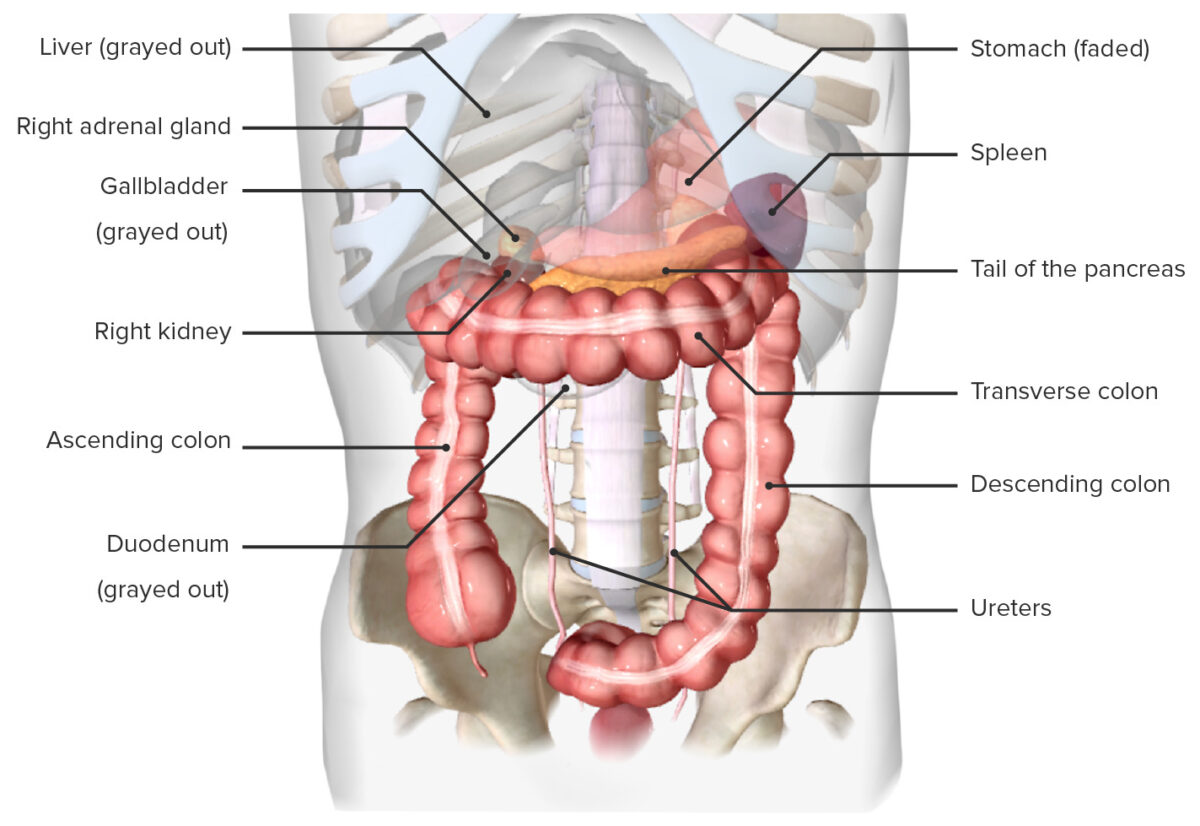
Location of the spleen, in situ (anterior view)
Image by BioDigital, edited by Lecturio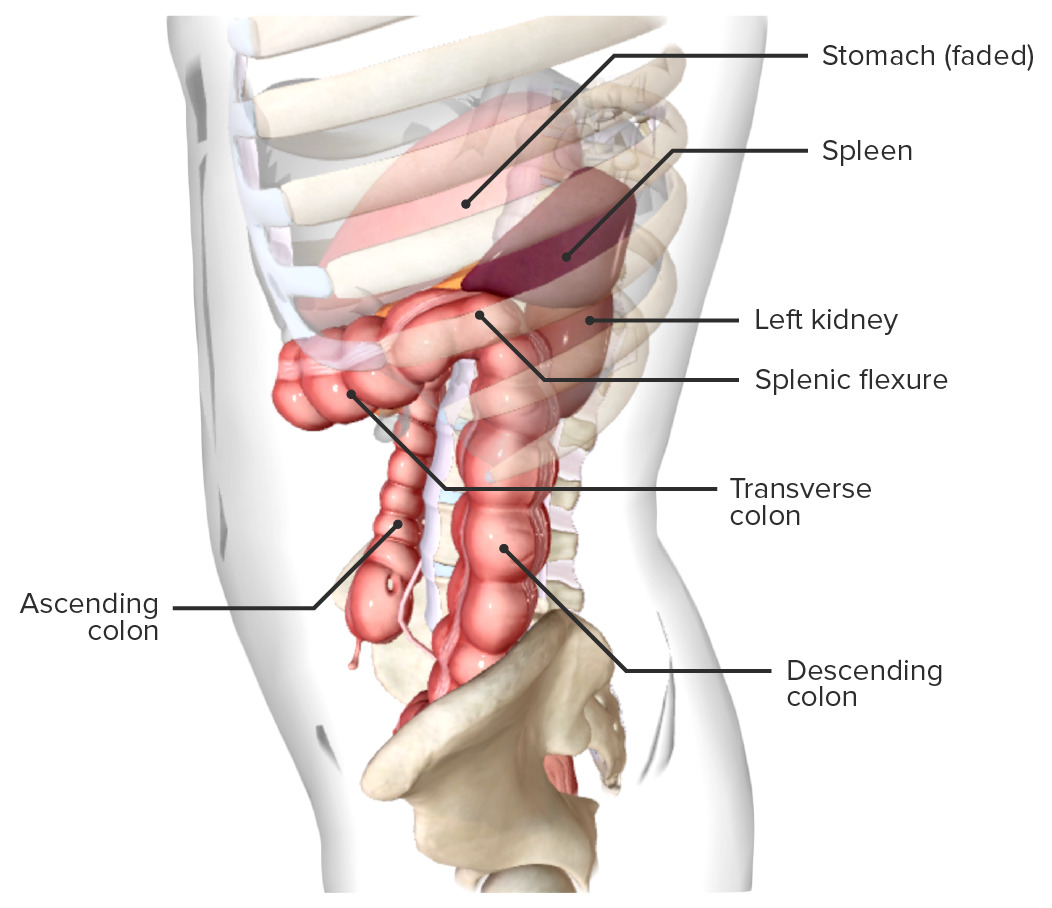
Location of the spleen, in situ (lateral view)
Image by BioDigital, edited by Lecturio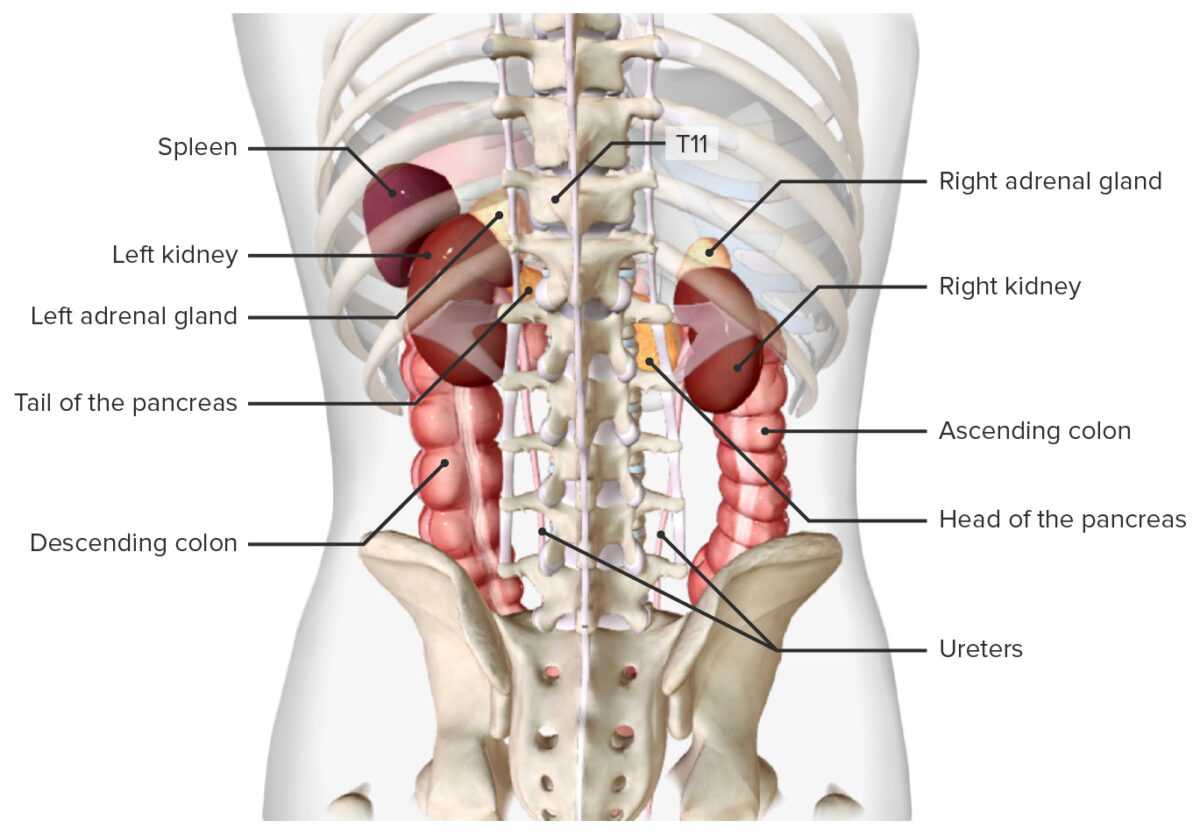
Location of the spleen, in situ (posterior view)
Image by BioDigital, edited by LecturioAverage measurements in normal healthy adults:
The spleen is connected to adjacent organs via several important ligaments.
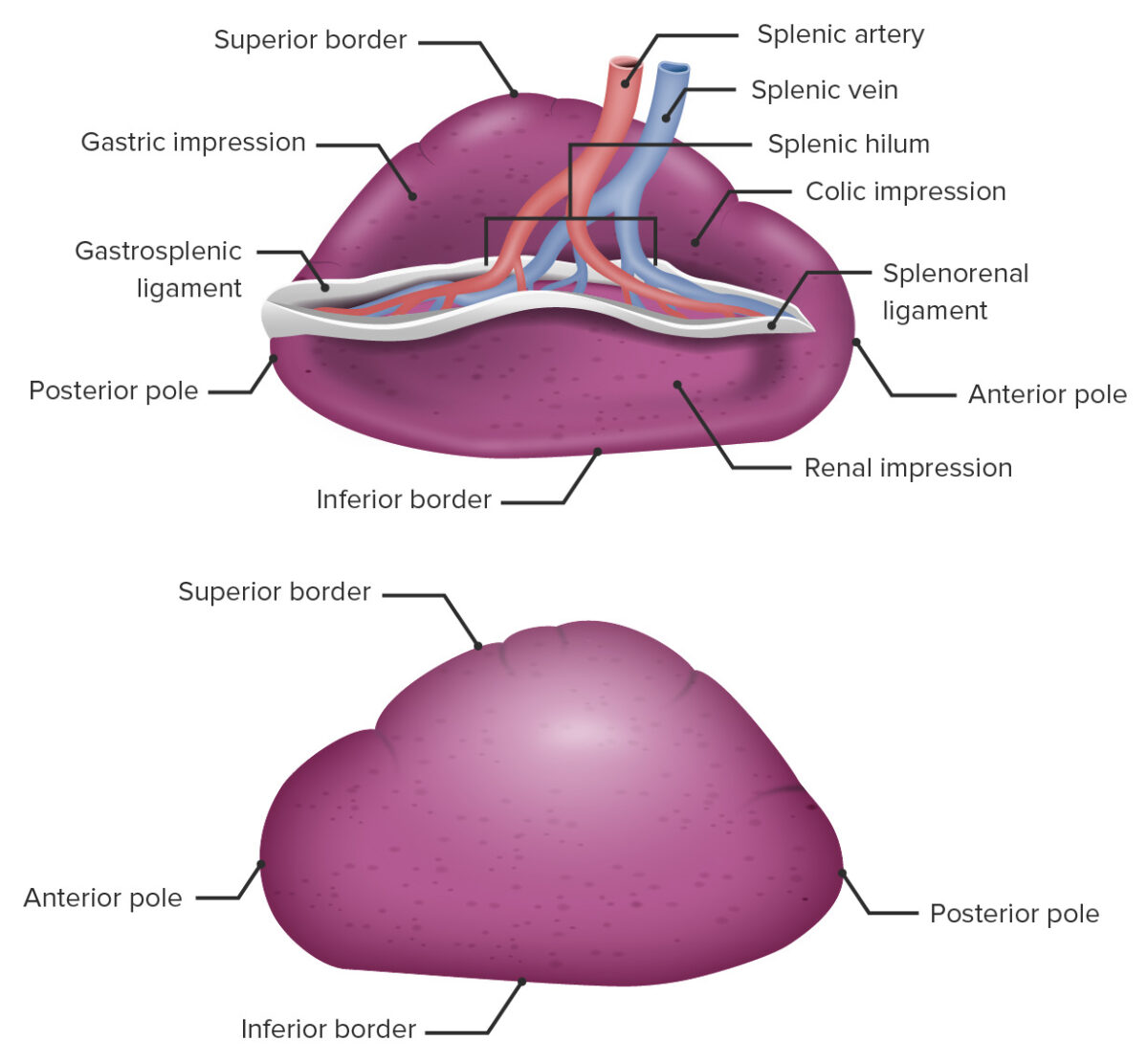
Gross anatomy of the spleen
Image by Lecturio.The spleen consists of a capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides and inner tissue known as parenchyma. The parenchyma consists of 2 types of tissues, white pulp White pulp Secondary Lymphatic Organs and red pulp Red pulp Secondary Lymphatic Organs.
The white pulp White pulp Secondary Lymphatic Organs makes up 25% of the spleen, surrounds the larger arterioles Arterioles The smallest divisions of the arteries located between the muscular arteries and the capillaries. Arteries: Histology in the spleen, and contains:
The red pulp Red pulp Secondary Lymphatic Organs makes up 75% of the spleen and is present between the white pulp White pulp Secondary Lymphatic Organs surrounding the larger vessels.
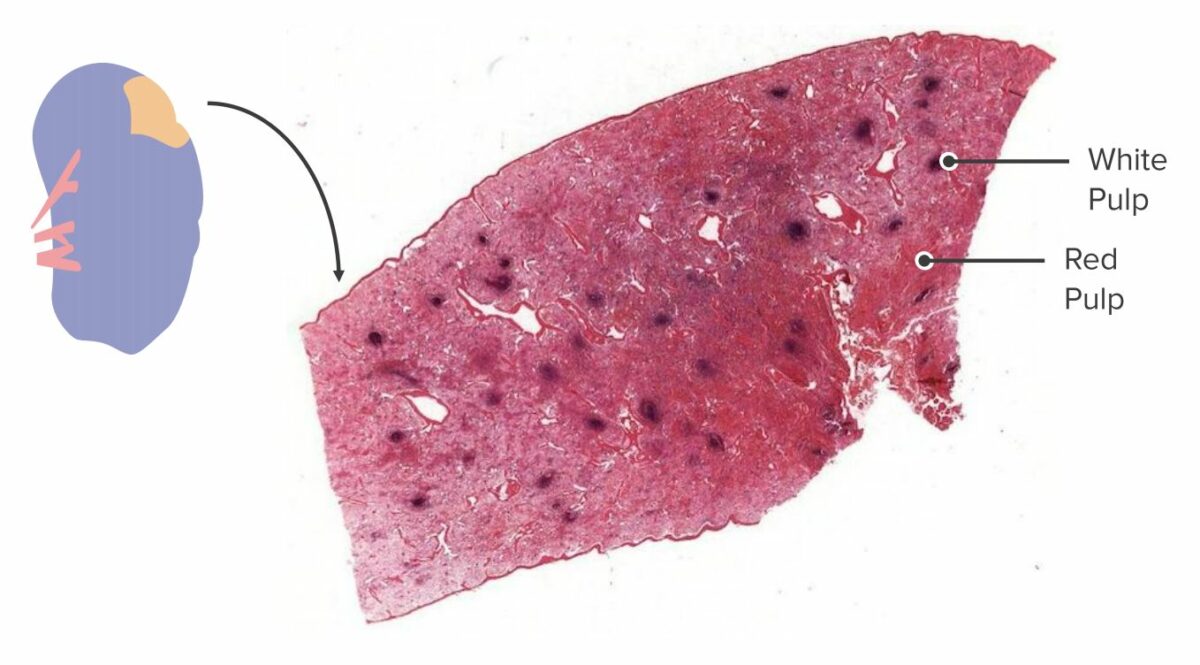
Cross-section of a spleen:
In a gross specimen, the white pulp and red pulp can be identified and differentiated owing to their difference in color and placement. White pulp agglomerates around blood vessels, while red pulp makes up the rest of the parenchyma.

Histologic section of the spleen:
The periarteriolar lymphoid sheath (PALS) engulfs a central arteriole. A lymphoid nodule has formed, surrounded by T cells, indicating that an antigen was detected in the splenic blood supply and an immune response was initiated.
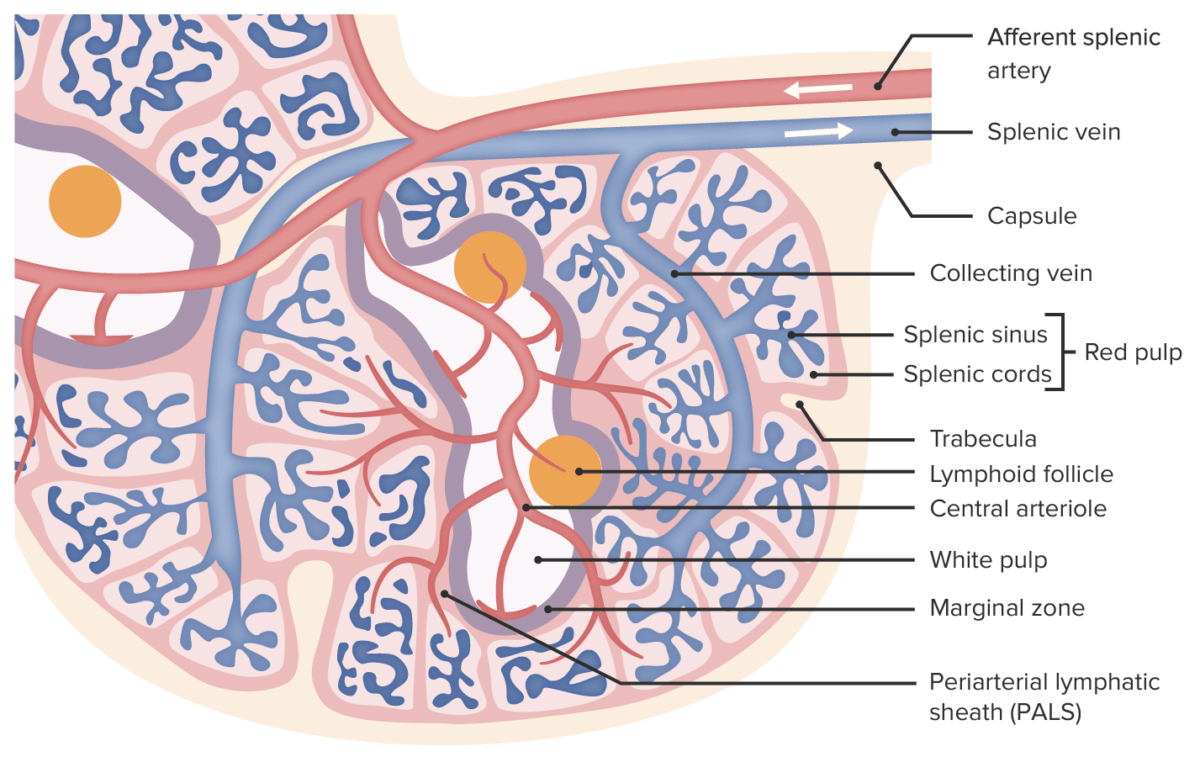
Microscopic anatomy of the spleen
Image by Lecturio.About 10% of the blood stays within the vessels, whereas approximately 90% is filtered out into the splenic tissue. Blood flows to, through, and out of the spleen as follows:
Innervation of the spleen takes place via the ANS ANS The ans is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ans consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy.
The spleen is the largest secondary lymphoid organ in the body. The functions of the spleen are primarily immunologic and hematologic. Survival without a spleen is possible as it is not a vital organ.