The spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy plays a crucial role in immune function, blood filtration, and platelet storage. Asplenia is the absence of splenic tissue or function and can stem from several factors ranging from congenital to iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome. There is a distinction between anatomic asplenia, which is due to the surgical removal of the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy, and functional asplenia, which is due to a condition that leads to splenic atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation, infarct Infarct Area of necrotic cells in an organ, arising mainly from hypoxia and ischemia Ischemic Cell Damage, congestion, or infiltrative disease. Howell-Jolly bodies are commonly seen on peripheral blood smear Peripheral Blood Smear Anemia: Overview and Types. Abdominal imaging and scintigraphy Scintigraphy Sjögren Syndrome are used for diagnosis. High risk of sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock caused by encapsulated Encapsulated Klebsiella bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology requires adherence to a strict vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination schedule and early antibiotic treatment when an infection is suspected. Thromboembolic events are common.
Last updated: Apr 14, 2025
The spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy is one of the secondary lymphatic organs Secondary lymphatic organs The secondary lymphoid organs, also called peripheral lymphoid/lymphatic organs, include MALT, the lymph nodes, and the spleen. These collections of lymphoid tissues provide constant surveillance for pathogens. In their distinct sites, these tissues are filled with immune cells ready to mount a response when antigens are detected. Secondary Lymphatic Organs central to immune function that plays a role in filtering the blood and removing old or damaged erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology. Asplenia is defined as the lack of a spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy or splenic function.
Epidemiology differs based on etiology.
| Category | Disease/condition |
|---|---|
| Congenital |
|
| Iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome |
|
| Circulatory |
|
| Hematologic/oncologic |
|
| Hepatic |
|
| Autoimmune |
|
| GI |
|
| Infectious |
|
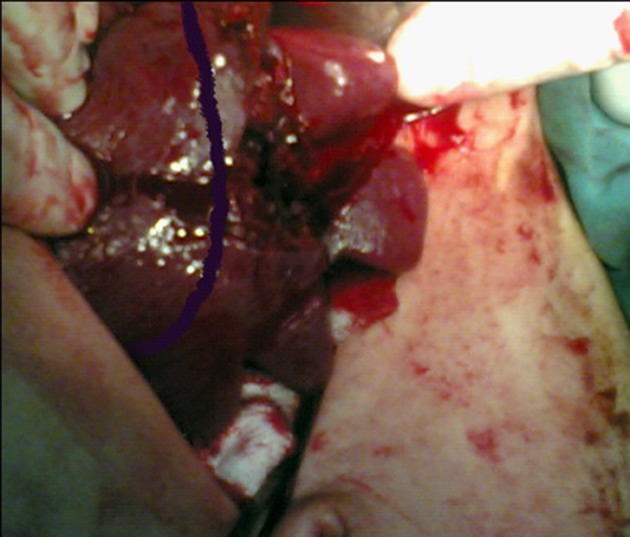
Stage IV splenic injury in a 34-year-old patient
Image: “Stage IV Splenic injury in a 34 Year Old Patient” by Eskandarlou, M., Derakhshanfar, A. License: CC BY 3.0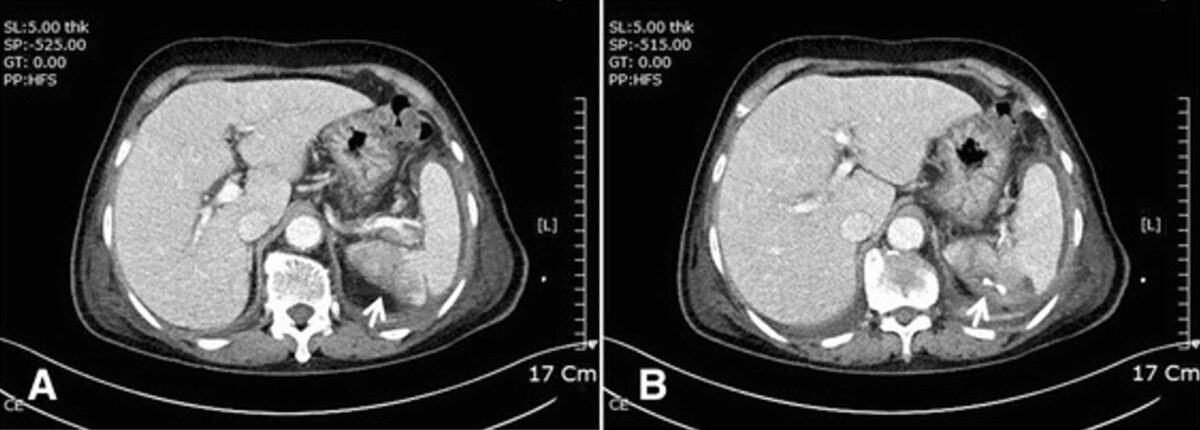
Computed tomography shows splenic infarction (A: white arrow) and abscess with percutaneous drainage (B: white arrow).
Image: “Complicated infective endocarditis: a case series” by Journal of Medical Case Reports. License: CC BY 4.0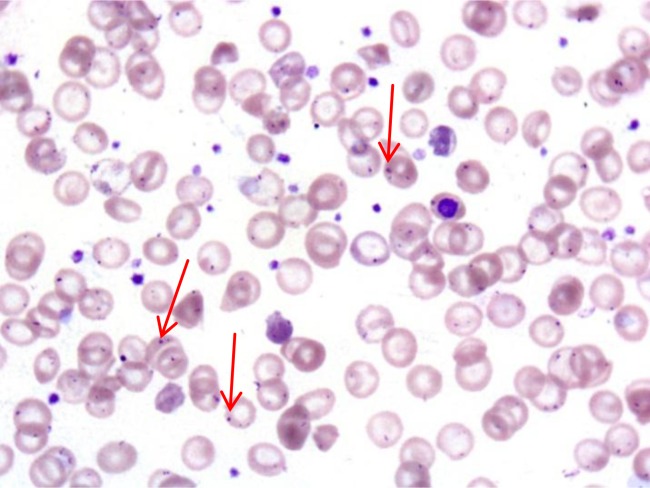
Howell-Jolly bodies:
Howell-Jolly bodies (red arrows) in circulating RBCs of a patient with overwhelming post-splenectomy infection (OPSI)
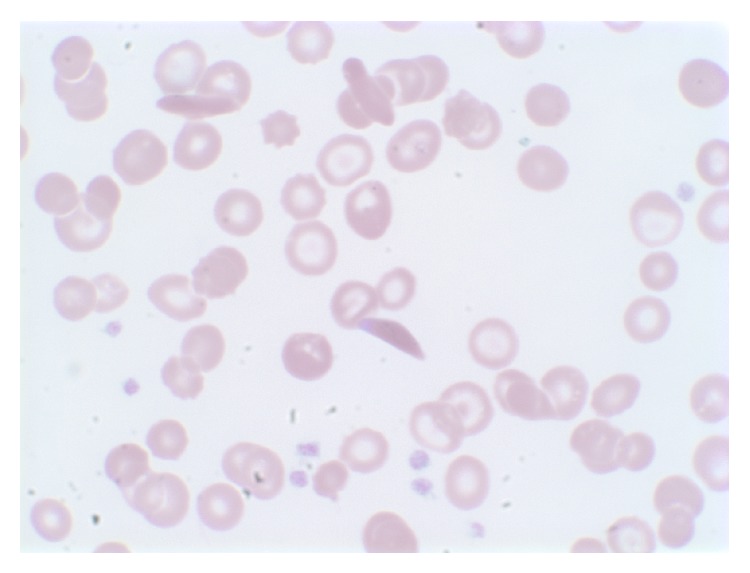
Peripheral blood smear of patient on high magnification shows irreversible sickled cells, anisocytosis, poikilocytosis, and target cells.
Image: “Peripheral blood smear” by Shemisa K, Jafferjee N, Thomas D, Jacobs G, Meyerson HJ. License: CC BY 3.0Management depends on the underlying cause, degree of asplenia, and age. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship > 5 years of age have a better prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas. Prevention of infection is the cornerstone of long-term care because of the increased risk of rapidly progressing septicemia that is fatal in 50% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
Rapid-onset septicemia:
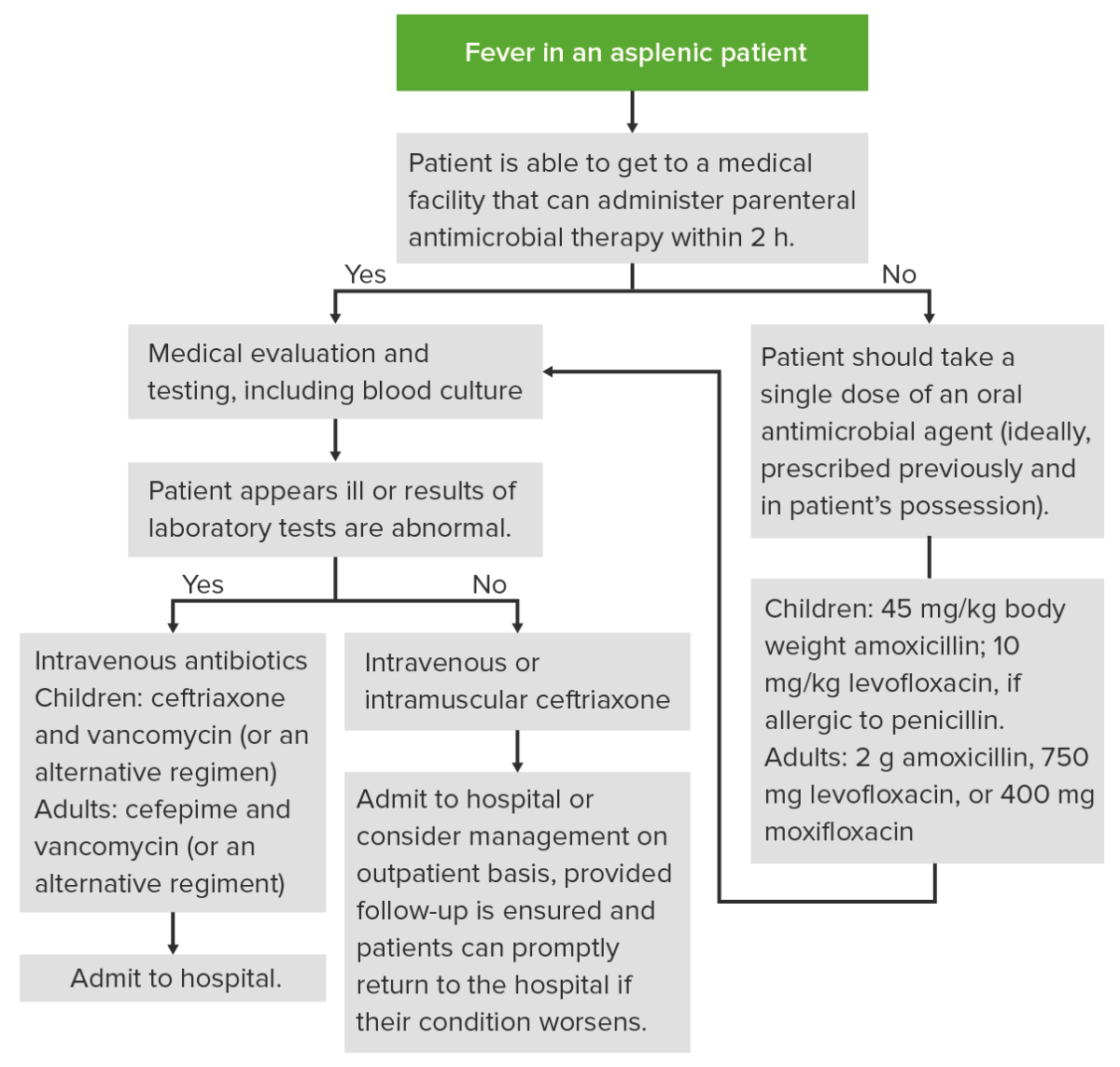
Management of an episode of fever in an asplenic patient
Image by Lecturio. License: CC BY-NC-SA 4.0