Thyroiditis is a catchall term used to describe a variety of conditions that have inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland in common. It includes pathologies that cause an acute illness with severe thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways (e.g., subacute thyroiditis and infectious thyroiditis) as well as conditions in which there is no clinically evident inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation and the manifestations primarily reflect thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy dysfunction or a goiter Goiter A goiter is a chronic enlargement of the thyroid gland due to nonneoplastic growth occurring in the setting of hypothyroidism, hyperthyroidism, or euthyroidism. Morphologically, thyroid enlargement can be diffuse (smooth consistency) or nodular (uninodular or multinodular). Goiter (e.g., painless thyroiditis and fibrous Fibrous Fibrocystic Change Riedel’s thyroiditis). The etiology of thyroiditis is varied and includes autoimmune inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation (most common), bacterial or viral infection, and drug-induced reactions. The inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy leads to a sequential Sequential Computed Tomography (CT) pathologic process that can result in signs and symptoms of hyperthyroidism Hyperthyroidism Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate. Thyrotoxicosis and Hyperthyroidism followed by signs and symptoms of hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto's disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism. The resulting damage can be temporary or permanent, and the treatment depends on the underlying cause.
Last updated: May 17, 2024
Thyroiditis, or inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland, has multiple etiologies, including autoimmune conditions, infectious agents, and iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome causes. Each causative condition has a specific pathologic mechanism.
| Category | Etiology | Pathophysiology |
|---|---|---|
| Autoimmune | Hashimoto’s thyroiditis |
|
| Painless, silent, or lymphocytic thyroiditis |
|
|
| Postpartum thyroiditis Postpartum thyroiditis Transient autoimmune thyroiditis occurring in the postpartum period. It is characterized by the presence of high titers of autoantibodies against thyroid peroxidase and thyroglobulin. Clinical signs include the triphasic thyroid hormone pattern: beginning with thyrotoxicosis, followed with hypothyroidism, then return to euthyroid state by 1 year postpartum. Postpartum Complications |
|
|
| Riedel’s thyroiditis |
|
|
| Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease | Subacute granulomatous thyroiditis (De Quervain syndrome) |
|
| Acute suppurative thyroiditis |
|
|
| Chronic suppurative thyroiditis | Usually caused by Aspergillus Aspergillus A genus of mitosporic fungi containing about 100 species and eleven different teleomorphs in the family trichocomaceae. Echinocandins or Pneumocystis in immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship | |
| Iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome | Drug-induced |
|
| Radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma thyroiditis |
|
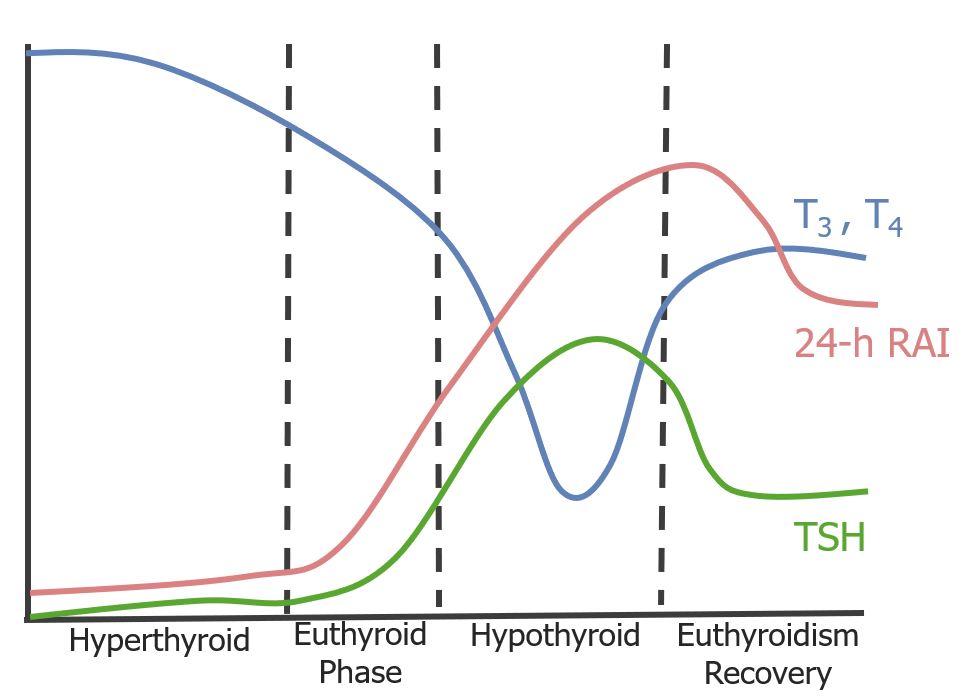
The triphasic clinical course of subacute thyroiditis:
Subacute thyroiditis usually presents initially with signs of hyperthyroidism as large amounts of thyroid hormones are released from the destroyed glandular tissue. Then, as storage runs out, thyroid hormone levels begin to drop and thyroid-stimulating hormone (TSH) rises to compensate. Eventually, months after the onset of the disease, hormonal levels stabilize into a euthyroid state.
RAI: radioactive iodine.
| Manifestations | Hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto’s disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism | Hyperthyroidism Hyperthyroidism Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate. Thyrotoxicosis and Hyperthyroidism |
|---|---|---|
| Metabolic |
|
|
| Dermatologic |
|
|
| Ocular | Periorbital Periorbital Orbital and Preseptal Cellulitis edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema |
|
| Musculoskeletal |
|
|
| Reproductive |
|
|
| Neuropsychiatric |
|
|
| GI |
|
|
| Cardiovascular |
|
|
The type of therapy used will depend on which phase the patient presents or the specific cause of the condition.
The differential diagnosis of thyroiditis depends on the differentiation/recognition of the various conditions that can produce inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland. The following are the most common causes and their characteristic presentations.