Carpal tunnel syndrome (CTS) is a complex of signs and symptoms caused by compression Compression Blunt Chest Trauma of the median nerve Median Nerve A major nerve of the upper extremity. In humans, the fibers of the median nerve originate in the lower cervical and upper thoracic spinal cord (usually C6 to T1), travel via the brachial plexus, and supply sensory and motor innervation to parts of the forearm and hand. Cubital Fossa: Anatomy as it crosses the carpal tunnel. Presentation is with pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and paresthesia of the dermatomal Dermatomal Dermatologic Examination target tissues innervated by the median nerve Median Nerve A major nerve of the upper extremity. In humans, the fibers of the median nerve originate in the lower cervical and upper thoracic spinal cord (usually C6 to T1), travel via the brachial plexus, and supply sensory and motor innervation to parts of the forearm and hand. Cubital Fossa: Anatomy as well as weakness and atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation of the nerve's myotomal targets. Risk factors that cause a predisposition to CTS include obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity, female sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria, pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, inflammatory conditions, genetic predisposition, and occupational factors. A clinical diagnosis may be made on the basis of history and physical examination and confirmed with electrodiagnostic testing. Conservative management includes splinting and physical therapy Physical Therapy Becker Muscular Dystrophy; more severe cases may require surgical correction.
Last updated: Mar 25, 2025
Mnemonic:
Median-innervated hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy muscles (Meat-LOAF):
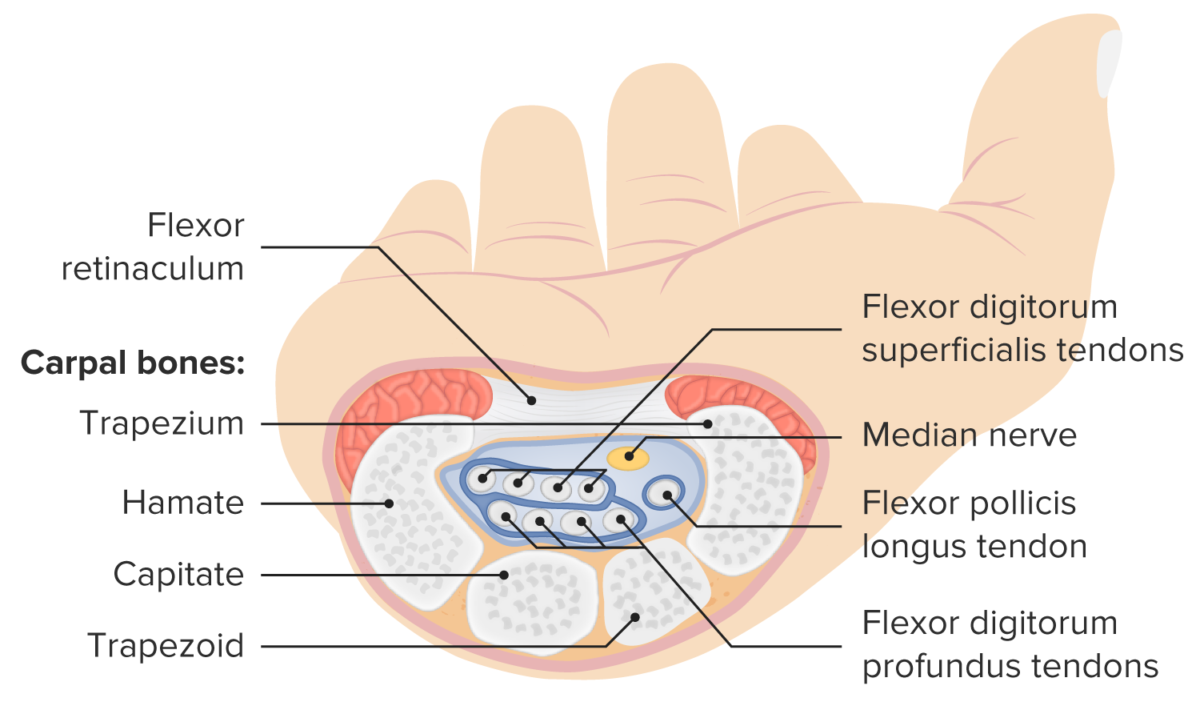
Structure and contents of the carpal tunnel
Image by Lecturio.
Thenar muscles of the hand
Image by Lecturio.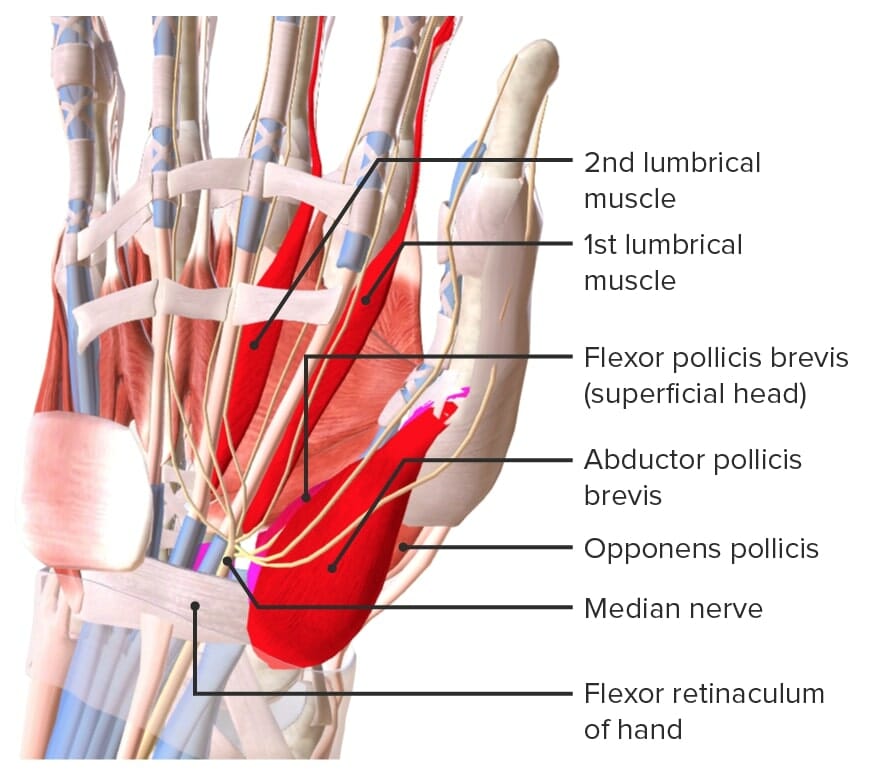
Median-innervated hand muscles (Meat-LOAF):
Meat: median nerve
L: 1st and 2nd lumbricals
O: opponens pollicis
A: abductor pollicis brevis
F: flexor pollicis brevis
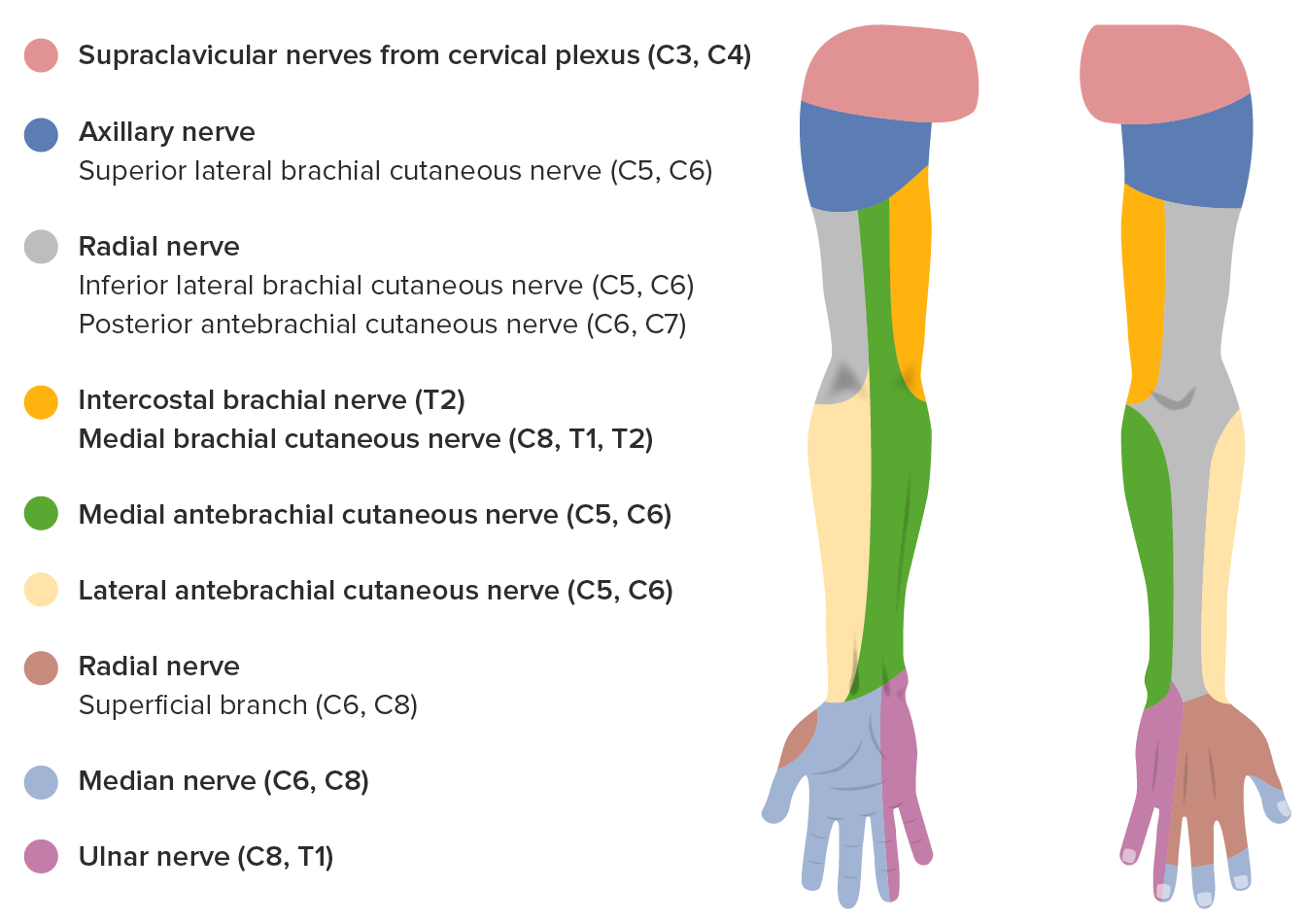
Sensory innervation of the median nerve
Image by Lecturio.The pathophysiology of narrowing of the carpal tunnel and median nerve Median Nerve A major nerve of the upper extremity. In humans, the fibers of the median nerve originate in the lower cervical and upper thoracic spinal cord (usually C6 to T1), travel via the brachial plexus, and supply sensory and motor innervation to parts of the forearm and hand. Cubital Fossa: Anatomy dysfunction are multifactorial.
Carpal tunnel syndrome is a clinical diagnosis. A combination of clinical findings with confirmatory electrodiagnostic testing is more accurate for diagnosis.
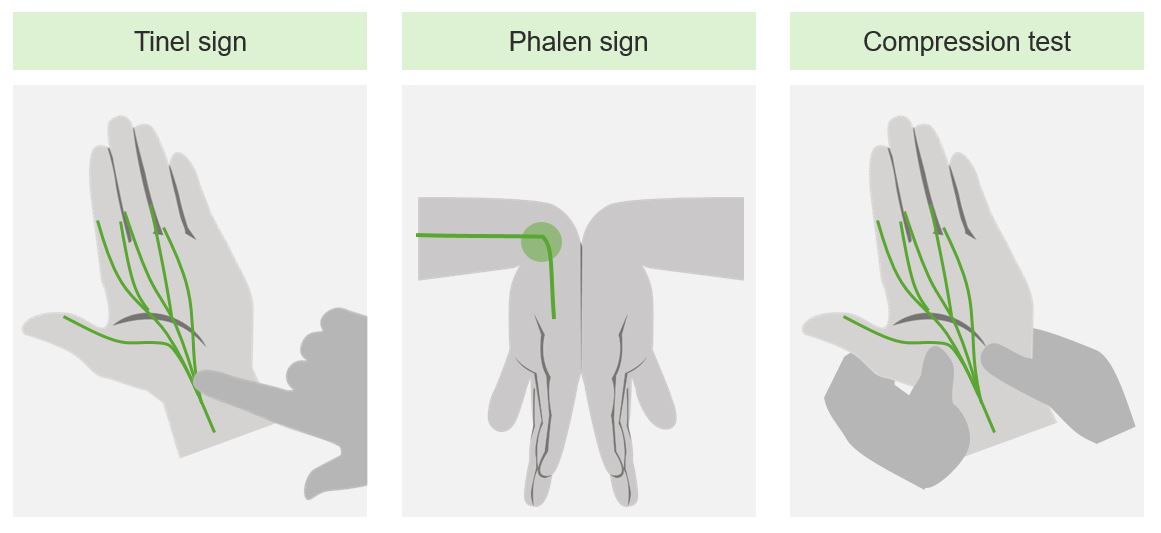
Provocative maneuvers for clinical evaluation of carpal tunnel syndrome
Image by Lecturio.
Untreated carpal tunnel syndrome
Image: “Untreated Carpal Tunnel Syndrome” by Dr. Harry Gouvas. License: CC BY 4.0Imaging is useful if structural abnormality is suspected.
Clinical grading Grading Methods which attempt to express in replicable terms the level of cell differentiation in neoplasms as increasing anaplasia correlates with the aggressiveness of the neoplasm. Grading, Staging, and Metastasis of CTS severity:
Electrodiagnostic grading Grading Methods which attempt to express in replicable terms the level of cell differentiation in neoplasms as increasing anaplasia correlates with the aggressiveness of the neoplasm. Grading, Staging, and Metastasis of CTS severity:
Management is based on the acuity and severity of clinical symptoms and the degree of neurogenic injury as assessed by electrodiagnostic studies.
For individuals with mild to moderate CTS, the rate of successful outcomes is 20%–93%. Options include: