Wound healing is a physiological process involving tissue repair in response to injury. It involves a complex interaction of various cell types, cytokines Cytokines Non-antibody proteins secreted by inflammatory leukocytes and some non-leukocytic cells, that act as intercellular mediators. They differ from classical hormones in that they are produced by a number of tissue or cell types rather than by specialized glands. They generally act locally in a paracrine or autocrine rather than endocrine manner. Adaptive Immune Response, and inflammatory mediators. The overall process protects underlying structures from further damage. Wound healing stages include hemostasis Hemostasis Hemostasis refers to the innate, stepwise body processes that occur following vessel injury, resulting in clot formation and cessation of bleeding. Hemostasis occurs in 2 phases, namely, primary and secondary. Primary hemostasis involves forming a plug that stops the bleeding temporarily. Secondary hemostasis involves the activation of the coagulation cascade. Hemostasis, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, granulation, and remodeling. Certain conditions such as diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, peripheral vascular disease, and malnutrition Malnutrition Malnutrition is a clinical state caused by an imbalance or deficiency of calories and/or micronutrients and macronutrients. The 2 main manifestations of acute severe malnutrition are marasmus (total caloric insufficiency) and kwashiorkor (protein malnutrition with characteristic edema). Malnutrition in children in resource-limited countries can limit Limit A value (e.g., pressure or time) that should not be exceeded and which is specified by the operator to protect the lung Invasive Mechanical Ventilation the body’s ability to heal itself, thus resulting in complications.
Last updated: May 17, 2024
There are 3 main stages of wound healing:
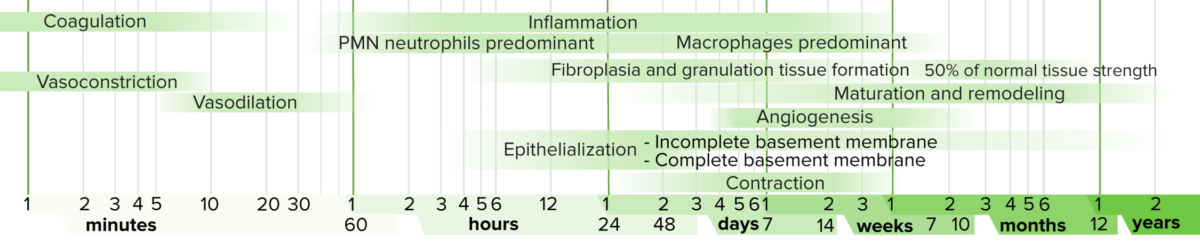
Timeline of wound healing
Image: “Timeline of Wound Healing” by Wikimedia Commons. License: Public Domain Files| Day 1 |
|
|---|---|
| Day 2 |
|
| Day 3 |
|
| Days 4-6 |
|
| Week 2 |
|
| Month 1 |
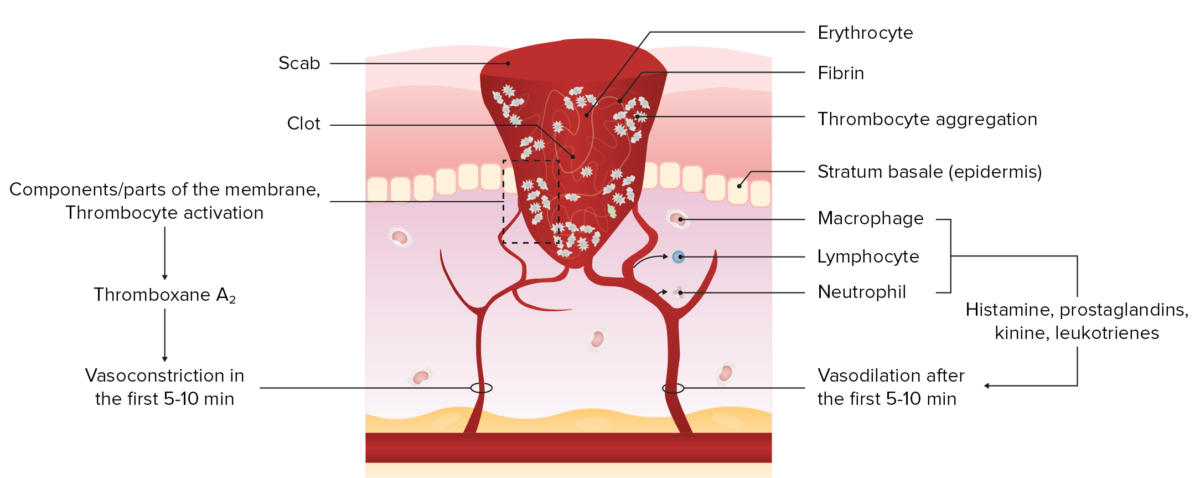
Exudative phase (immediately after injury): hemostasis and inflammation
Image by Lecturio.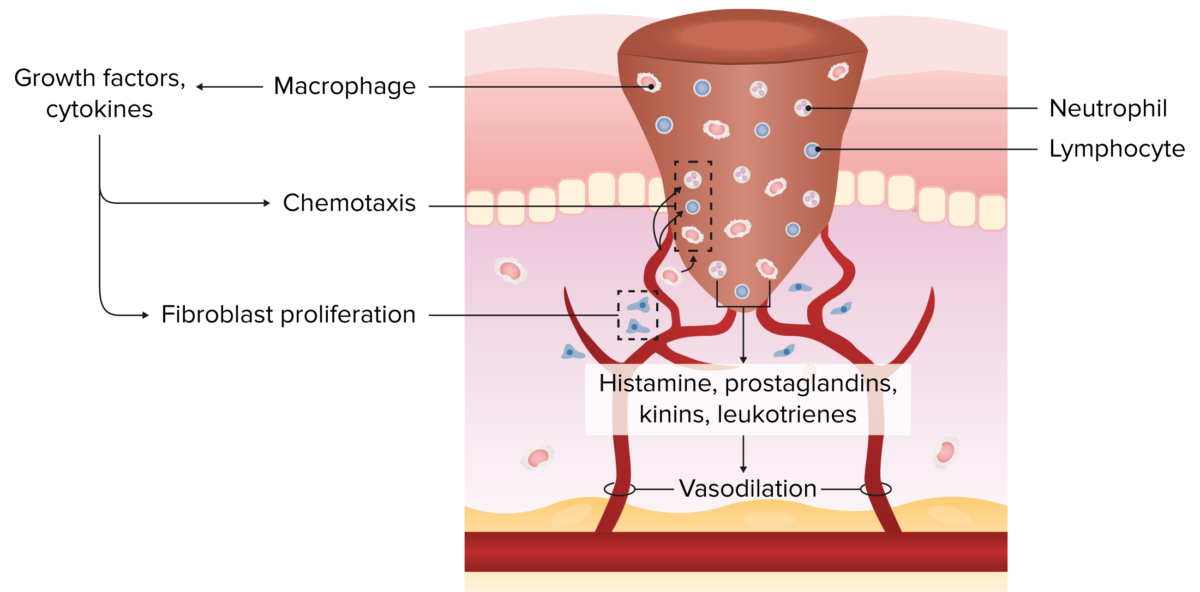
Exudative phase (day 1–4): inflammation and resorption
Image by Lecturio.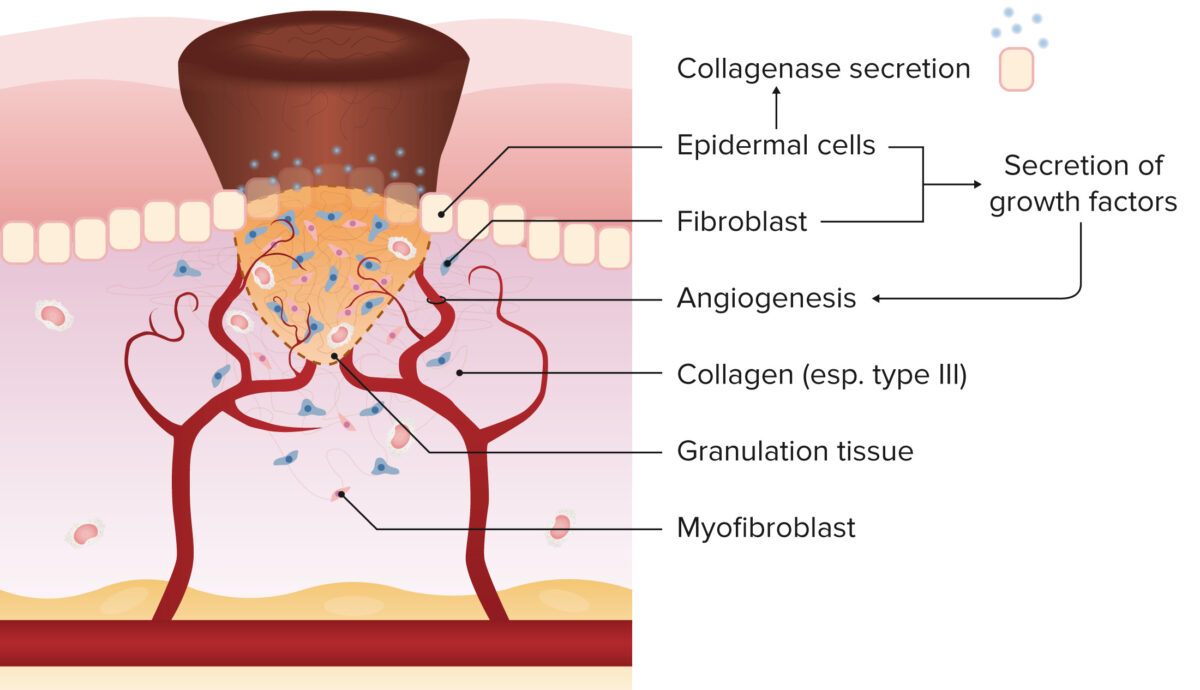
Proliferative phase (day 2–16): granulation
Image by Lecturio.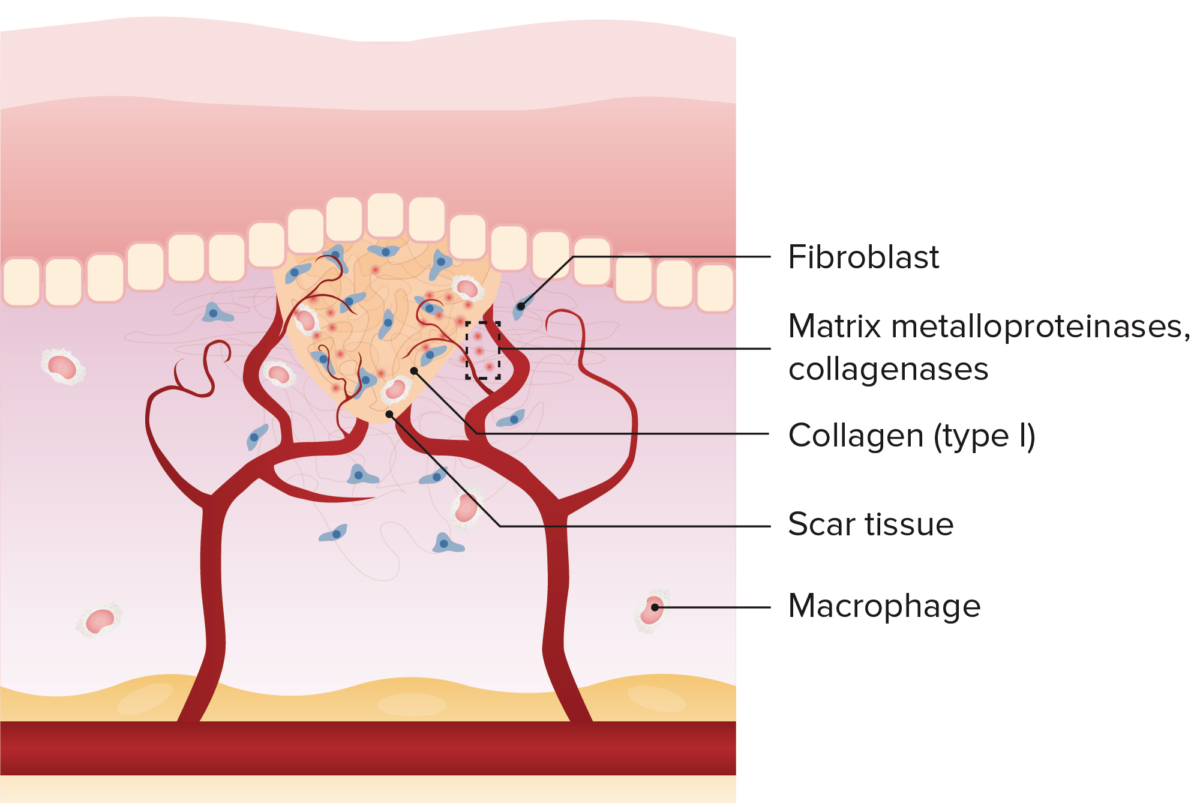
Reparative phase (day 5–25): epithelization
Image by Lecturio.
Wound on palm of the hand a day after falling off a bike onto concrete: day 1
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 2
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 3
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 4
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 5
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 6
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 7
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 8
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 9
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 10
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 11
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files
Wound on palm of the hand after falling off a bike onto concrete: day 12
Image: “Wound on palm of hand” by Arria Belli – Own Work. License: Public Domain Files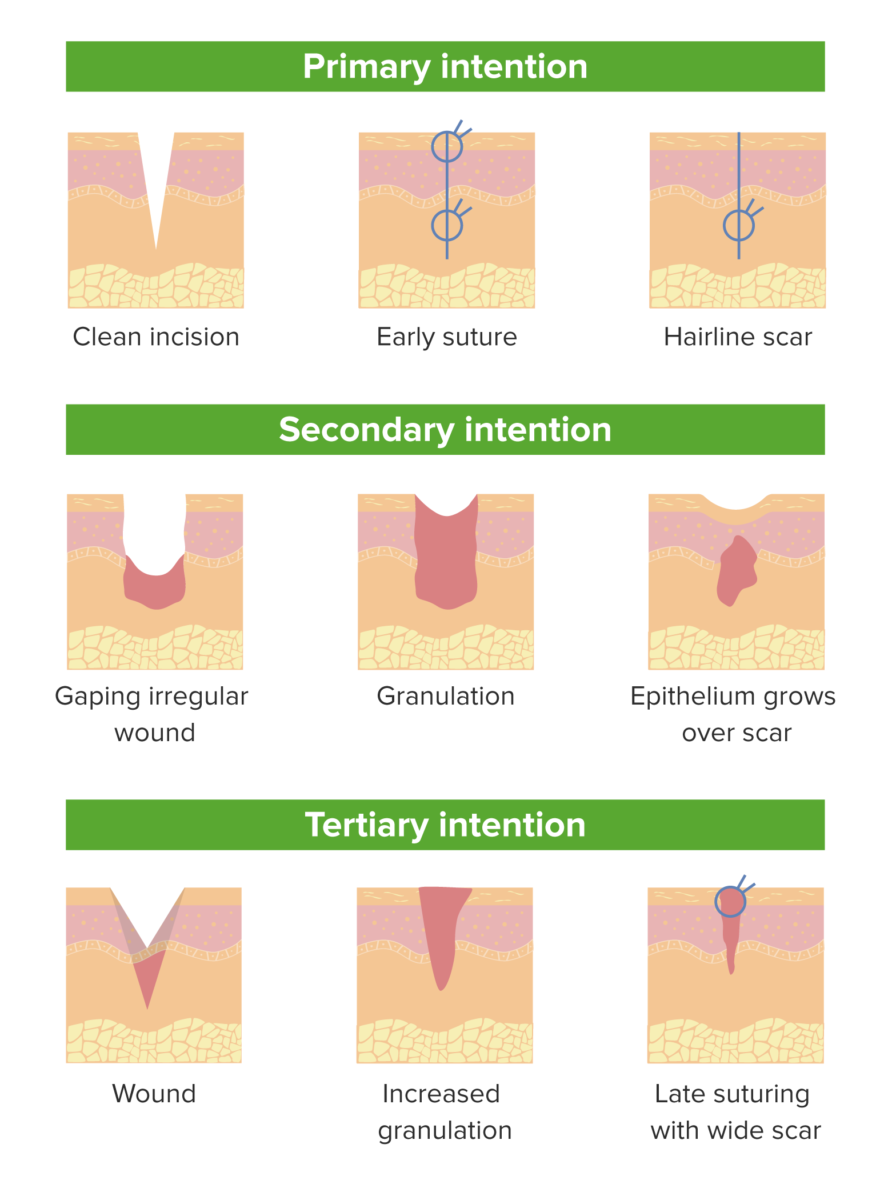
Processes of primary, secondary, and tertiary wound healing
Image by Lecturio.
Keloid found on the foot of a patient
Image: “Preoperative appearance of a patient” by Department of Plastic and Reconstructive Surgery, Kangbuk Samsung Hospital, Seoul; Deokjeok Health Care Center, Incheon. License: CC BY 2.0
Diabetic foot syndrome
Image: by Intermedichbo from Wikimedia Commons. License: CC BY-SA 4.0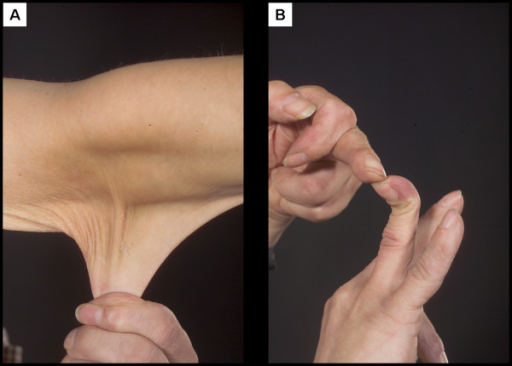
Example of a patient with Ehlers-Danlos syndrome
Image: by Division of Ophthalmology and Visual Sciences, Queen Medical Centre, University of Nottingham, Nottingham, NG7 2UH, UK. License: CC BY 2.0
Two examples of hypertrophic scars on the dorsum of the hand
Image: “Treatment of Hypertrophic Scar in Human with Autologous Transplantation of Cultured Keratinocytes and Fibroblasts along with Fibrin Glue” by Department of Stem Cells and Developmental Biology at Cell Science Research Center, Royan Institute for Stem Cell Biology and Technology, ACECR, Tehran, Iran. License: CC BY 2.5, edited by Lecturio.
DIABETIC ulcer on the great toe
Image: “Diabetisches Fußsyndrom” by Papa1234. License: Public Domain