Malassezia is a lipophilic yeast Yeast A general term for single-celled rounded fungi that reproduce by budding. Brewers' and bakers' yeasts are saccharomyces cerevisiae; therapeutic dried yeast is yeast, dried. Mycology commonly found on the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions surfaces of many animals Animals Unicellular or multicellular, heterotrophic organisms, that have sensation and the power of voluntary movement. Under the older five kingdom paradigm, animalia was one of the kingdoms. Under the modern three domain model, animalia represents one of the many groups in the domain eukaryota. Cell Types: Eukaryotic versus Prokaryotic, including humans. In the presence of certain environments or triggers, this fungus can cause pathologic diseases ranging from superficial skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions conditions (tinea versicolor and dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema)) to invasive disease (e.g., Malassezia folliculitis, catheter-associated fungemia Fungemia The presence of fungi circulating in the blood. Opportunistic fungal sepsis is seen most often in immunosuppressed patients with severe neutropenia or in postoperative patients with intravenous catheters and usually follows prolonged antibiotic therapy. Chronic Granulomatous Disease, meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis, and urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with tinea versicolor develop an asymptomatic or mildly pruritic hypopigmented or hyperpigmented rash Rash Rocky Mountain Spotted Fever on the chest, back, abdomen, or face. Seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) presents with an erythematous, pruritic rash Rash Rocky Mountain Spotted Fever with greasy scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions and yellow crust Crust Dried exudate of body fluids (blood, pus, or sebum) on an area of damaged skin Secondary Skin Lesions, most commonly affecting areas of the face, upper trunk, or intertriginous regions. The presentation of Malassezia folliculitis is similar to that of bacterial folliculitis, with pruritic, monomorphic papules or pustules in a follicular pattern. The diagnosis of the superficial skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions conditions is primarily by exam, but may be confirmed by microscopy of skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions scrapings. Management entails the use of topical and oral antifungal Antifungal Azoles agents.
Last updated: Jun 27, 2025
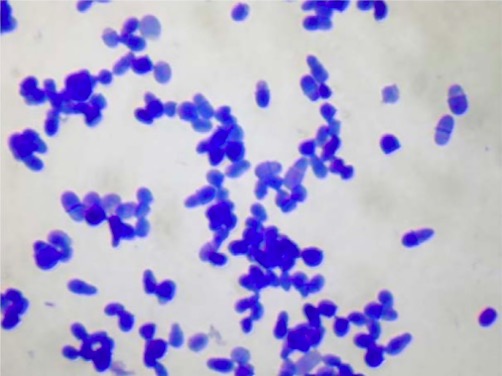
Methylene blue staining of Malassezia yeast
Image: “2916” by Allergy Unit, Department of Dermatology, University Hospital of Zurich, Gloriastrasse 31, 8091 Zurich, Switzerland. License: CC BY 4.0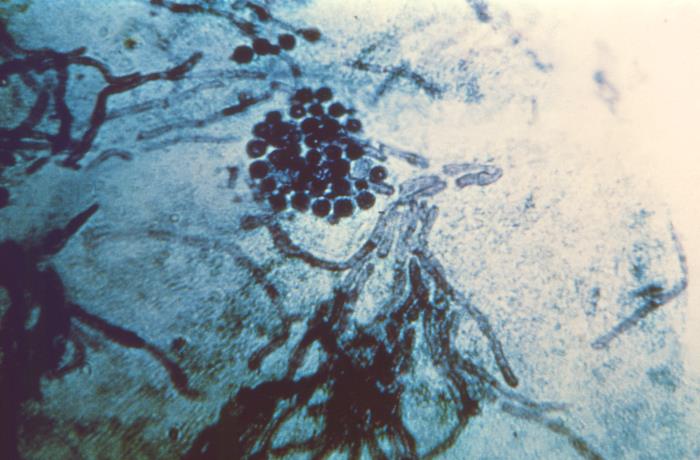
Photomicrograph of a skin scraping sample in a patient with tinea versicolor:
Note the presence of spherical, yeast-like fungal cells, and short hyphae of Malassezia species.
Microscopic appearance of Malassezia furfur fungal cells and hyphae from skin scraping in tinea versicolor
Image: “3938” by CDC. License: Public DomainThere are a number of recognized species:
Tinea versicolor:
Malassezia folliculitis:
Malassezia are part of the normal skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions flora in humans and animals Animals Unicellular or multicellular, heterotrophic organisms, that have sensation and the power of voluntary movement. Under the older five kingdom paradigm, animalia was one of the kingdoms. Under the modern three domain model, animalia represents one of the many groups in the domain eukaryota. Cell Types: Eukaryotic versus Prokaryotic.
Predisposing risk factors for disease include:
Tinea versicolor:
Seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema):
Malassezia folliculitis:
Symptoms:
Physical exam:

Patchy, erythematous rash on a patient’s chest, neck, and abdomen consistent with tinea versicolor
Image: “22849” by CDC/Dr. Lucille K. Georg. License: Public Domain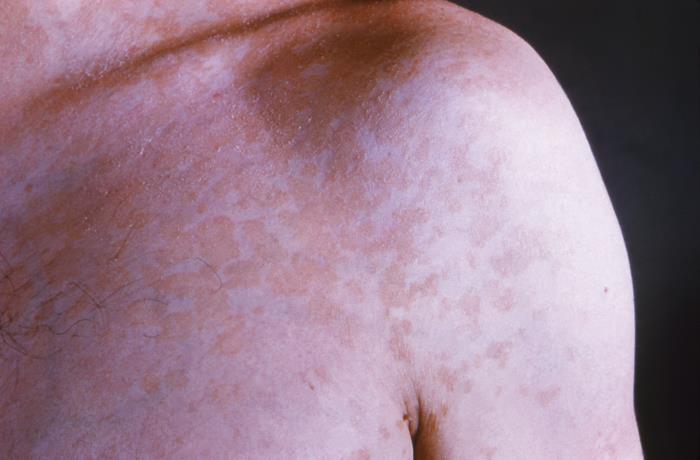
Plaque-like, blotchy, erythematous rash on a patient’s left shoulder due to tinea versicolor
Image: “22847” by CDC/Dr. Lucille K. Georg. License: Public Domain
Close-up view of a patient’s skin surface showing hyperpigmented lesions of tinea versicolor
Image: “22848” by CDC/Dr. Lucille K. Georg. License: Public Domain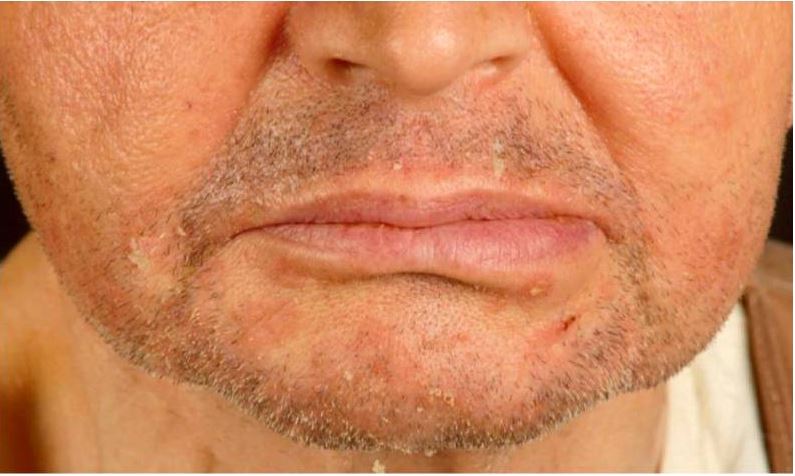
Seborrheic dermatitis in a renal transplant recipient:
Note erythematous scaly papules on the chin and nasolabial folds.
This condition may appear similar to acne vulgaris Acne vulgaris Acne vulgaris, also known as acne, is a common disorder of the pilosebaceous units in adolescents and young adults. The condition occurs due to follicular hyperkeratinization, excess sebum production, follicular colonization by Cutibacterium acnes, and inflammation. Acne Vulgaris or bacterial folliculitis:
The diagnosis is most often made clinically on the basis of the history and examination. Additional evaluation can include:
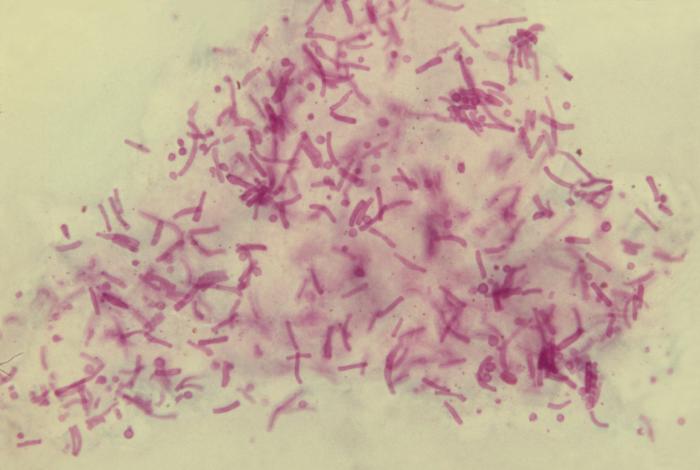
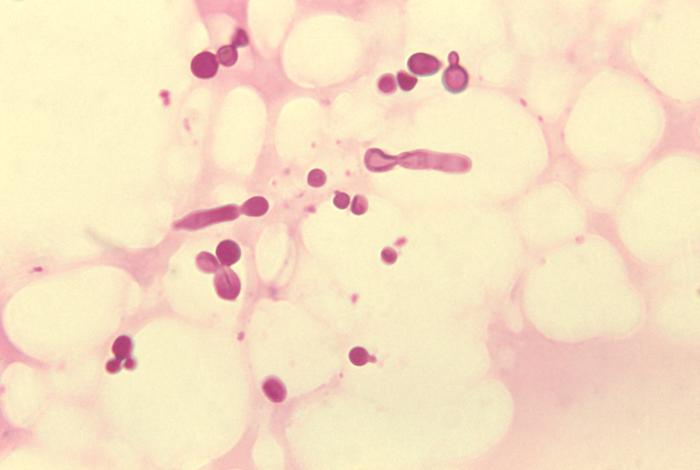
Malassezia furfur fungal organisms:
This photomicrograph of a skin scale tissue sample reveals the presence of numerous M. furfur fungal organisms. Note the spaghetti-and-meatballs appearance due to the presence of both yeast and hyphae.
Recurrences of tinea versicolor and seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) can be prevented with topical antifungal Antifungal Azoles prophylaxis Prophylaxis Cephalosporins.