Seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) is a common chronic, relapsing skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disorder that presents as erythematous plaques with greasy, yellow scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions in susceptible areas (scalp, face, and trunk). Seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) has a biphasic incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency, occurring in two peaks: first in infants, then in adolescence and early adulthood. Although the exact etiology is unknown, pathologic mechanisms have been observed involving the sebaceous glands and Malassezia Malassezia Malassezia is a lipophilic yeast commonly found on the skin surfaces of many animals, including humans. In the presence of certain environments or triggers, this fungus can cause pathologic diseases ranging from superficial skin conditions (tinea versicolor and dermatitis) to invasive disease (e.g., Malassezia folliculitis, catheter-associated fungemia, meningitis, and urinary tract infections). Malassezia Fungi on the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. Topical medications are used for acute exacerbation or maintenance treatment. These options aim to inhibit skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions colonization Colonization Bacteriology ( antifungal Antifungal Azoles agents), reduce inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation ( steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors, calcineurin inhibitors Calcineurin Inhibitors Compounds that inhibit or block the phosphatase activity of calcineurin. Immunosuppressants), and loosen scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions and crusts (keratolytic agents). Severe and refractory seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) may warrant the use of systemic antifungal Antifungal Azoles medications.
Last updated: May 17, 2024
Seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) is a common chronic skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions disorder that is characterized by erythematous patches Patches Vitiligo with greasy, yellowish scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions that most often appear in areas with prominent sebaceous glands (scalp, face, upper trunk, and anogenital area).
Unclear, but may be affected by the following:

Images demonstrate typical findings of seborrheic dermatitis in newborns. Note the common involvement of intertriginous areas and the scalp.
Image: “Seborrheic dermatitis.” by Siegfried EC, Hebert AA. License: CC BY 4.0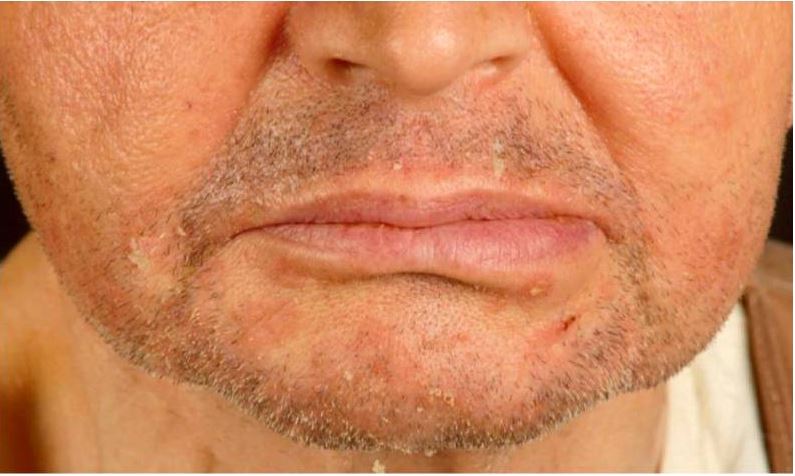
Seborrheic dermatitis in a renal transplant recipient.
Note the erythematous scaly papules on the chin and nasolabial folds.
Differential diagnoses of seborrheic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema) include the following conditions:
| Site | Differential diagnosis |
|---|---|
| Scalp | Psoriasis Psoriasis Psoriasis is a common T-cell-mediated inflammatory skin condition. The etiology is unknown, but is thought to be due to genetic inheritance and environmental triggers. There are 4 major subtypes, with the most common form being chronic plaque psoriasis. Psoriasis, dandruff, atopic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema), tinea capitis Tinea capitis Ringworm of the scalp and associated hair mainly caused by species of Microsporum; Trichophyton; and Epidermophyton, which may occasionally involve the eyebrows and eyelashes. Dermatophytes/Tinea Infections |
| Face | Psoriasis Psoriasis Psoriasis is a common T-cell-mediated inflammatory skin condition. The etiology is unknown, but is thought to be due to genetic inheritance and environmental triggers. There are 4 major subtypes, with the most common form being chronic plaque psoriasis. Psoriasis, impetigo Impetigo Impetigo is a highly contagious superficial bacterial infection typically caused by Staphylococcus aureus (most common) and Streptococcus pyogenes. Impetigo most commonly presents in children aged 2 to 5 years with lesions that evolve from papules to vesicles to pustules, which eventually break down to form characteristic “honey-colored” crusts. Impetigo, contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination |
| Ear canal | Psoriasis Psoriasis Psoriasis is a common T-cell-mediated inflammatory skin condition. The etiology is unknown, but is thought to be due to genetic inheritance and environmental triggers. There are 4 major subtypes, with the most common form being chronic plaque psoriasis. Psoriasis, contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination |
| Eyelids Eyelids Each of the upper and lower folds of skin which cover the eye when closed. Blepharitis | Atopic dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema), demodex folliculorum Demodex Folliculorum Infectious Folliculitis infestation |
| Chest and trunk | Pityriasis rosea Pityriasis rosea Pityriasis rosea is an acute, self-limited skin disease. The etiology is not known, and it commonly occurs in young adults. Patients initially present with a single, ovoid “herald patch.” This is followed by diffuse, pruritic, scaly, oval lesions over the trunk (often in a “Christmas tree” distribution on the back) and extremities. Pityriasis Rosea, tinea versicolor Tinea versicolor A common chronic, noninflammatory and usually symptomless disorder, characterized by the occurrence of multiple macular patches of all sizes and shapes, and varying in pigmentation from fawn-colored to brown. It is seen most frequently in hot, humid, tropical regions and is mostly caused by Malassezia furfur (formerly Pityrosporum orbiculare). Malassezia Fungi |
| Intertriginous areas Intertriginous areas Malassezia Fungi | Psoriasis Psoriasis Psoriasis is a common T-cell-mediated inflammatory skin condition. The etiology is unknown, but is thought to be due to genetic inheritance and environmental triggers. There are 4 major subtypes, with the most common form being chronic plaque psoriasis. Psoriasis, candidiasis Candidiasis Candida is a genus of dimorphic, opportunistic fungi. Candida albicans is part of the normal human flora and is the most common cause of candidiasis. The clinical presentation varies and can include localized mucocutaneous infections (e.g., oropharyngeal, esophageal, intertriginous, and vulvovaginal candidiasis) and invasive disease (e.g., candidemia, intraabdominal abscess, pericarditis, and meningitis). Candida/Candidiasis |
| All sites, rule out | Secondary syphilis Secondary Syphilis Syphilis, pemphigus, scabies Scabies Scabies is an infestation of the skin by the Sarcoptes scabiei mite, which presents most commonly with intense pruritus, characteristic linear burrows, and erythematous papules, particularly in the interdigital folds and the flexor aspects of the wrists. Scabies |