Advertisement
Advertisement
Advertisement
Advertisement
Medications for the management of Parkinson's disease improve the symptoms of tremor Tremor Cyclical movement of a body part that can represent either a physiologic process or a manifestation of disease. Intention or action tremor, a common manifestation of cerebellar diseases, is aggravated by movement. In contrast, resting tremor is maximal when there is no attempt at voluntary movement, and occurs as a relatively frequent manifestation of parkinson disease. Myotonic Dystrophies, rigidity Rigidity Continuous involuntary sustained muscle contraction which is often a manifestation of basal ganglia diseases. When an affected muscle is passively stretched, the degree of resistance remains constant regardless of the rate at which the muscle is stretched. This feature helps to distinguish rigidity from muscle spasticity. Megacolon, and postural instability by increasing dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS levels in the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification. While levodopa is the drug of choice in individuals of any age with moderate or severe symptoms, other agents can be used as monotherapy for milder symptoms or in conjunction with levodopa–carbidopa for symptom control. Other classes of medications work by preventing central and peripheral dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS metabolism (monoamine oxidase Oxidase Neisseria (MAO) type B inhibitors, catechol O-methyltransferase (COMT) inhibitors, and carbidopa), or by exerting an antidyskinetic effect ( amantadine Amantadine An antiviral that is used in the prophylactic or symptomatic treatment of influenza A. It is also used as an antiparkinsonian agent, to treat extrapyramidal reactions, and for postherpetic neuralgia. The mechanisms of its effects in movement disorders are not well understood but probably reflect an increase in synthesis and release of dopamine, with perhaps some inhibition of dopamine uptake. Antivirals for Influenza). Serious side effects include arrhythmias and psychiatric symptoms ranging from mood disorders to hallucinations Hallucinations Subjectively experienced sensations in the absence of an appropriate stimulus, but which are regarded by the individual as real. They may be of organic origin or associated with mental disorders. Schizophrenia and psychosis. Abrupt withdrawal can result in neuroleptic malignant syndrome Neuroleptic malignant syndrome Neuroleptic malignant syndrome (NMS) is a rare, idiosyncratic, and potentially life-threatening reaction to antipsychotic drugs. Neuroleptic malignant syndrome presents with ≥ 2 of the following cardinal symptoms: fever, altered mental status, muscle rigidity, and autonomic dysfunction. Neuroleptic Malignant Syndrome–like symptoms, which can be life-threatening. Drug interactions may occur with other agents that are metabolized by the hepatic cytochrome P450 Cytochrome P450 A superfamily of hundreds of closely related hemeproteins found throughout the phylogenetic spectrum, from animals, plants, fungi, to bacteria. They include numerous complex monooxygenases (mixed function oxygenases). In animals, these p450 enzymes serve two major functions: (1) biosynthesis of steroids, fatty acids, and bile acids; (2) metabolism of endogenous and a wide variety of exogenous substrates, such as toxins and drugs (biotransformation). They are classified, according to their sequence similarities rather than functions, into cyp gene families (>40% homology) and subfamilies (>59% homology). For example, enzymes from the cyp1, cyp2, and cyp3 gene families are responsible for most drug metabolism. Drug-Induced Liver Injury enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes, and caution must be used to avoid serotonin Serotonin A biochemical messenger and regulator, synthesized from the essential amino acid l-tryptophan. In humans it is found primarily in the central nervous system, gastrointestinal tract, and blood platelets. Serotonin mediates several important physiological functions including neurotransmission, gastrointestinal motility, hemostasis, and cardiovascular integrity. Receptors and Neurotransmitters of the CNS syndrome.
Last updated: Feb 28, 2023
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Parkinson’s disease ( PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease) is a degenerative disease of the basal ganglia Basal Ganglia Basal ganglia are a group of subcortical nuclear agglomerations involved in movement, and are located deep to the cerebral hemispheres. Basal ganglia include the striatum (caudate nucleus and putamen), globus pallidus, substantia nigra, and subthalamic nucleus. Basal Ganglia: Anatomy characterized by a clinical syndrome manifesting with diminished facial expression, bradykinesia Bradykinesia Parkinson’s Disease, festinating gait Gait Manner or style of walking. Neurological Examination (progressively shortened and accelerated steps), cogwheel rigidity Cogwheel Rigidity Parkinson’s Disease, and a “pill-rolling” tremor Tremor Cyclical movement of a body part that can represent either a physiologic process or a manifestation of disease. Intention or action tremor, a common manifestation of cerebellar diseases, is aggravated by movement. In contrast, resting tremor is maximal when there is no attempt at voluntary movement, and occurs as a relatively frequent manifestation of parkinson disease. Myotonic Dystrophies at rest.
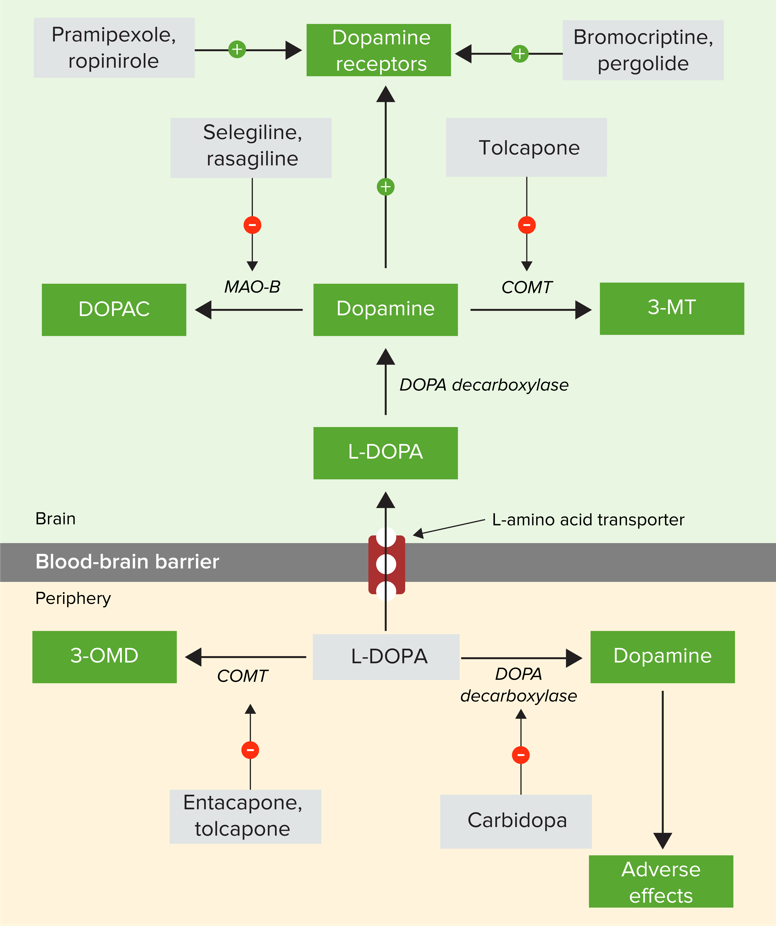
Pharmacologic strategies for the management of Parkinson’s disease
COMT: catechol O-methyltransferase
3-MT: 3-Methoxytyramine
3-OMD: 3-O-methyldopa
DOPAC: 3,4-dihydroxy-phenylacetic acid
L-DOPA: levodopa
MAO-B: monoamine oxidase type B
Recommended as 1st-line therapy for moderate to severe symptoms of PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease
While generally a well-tolerated medication, there are some side effects to be aware of:
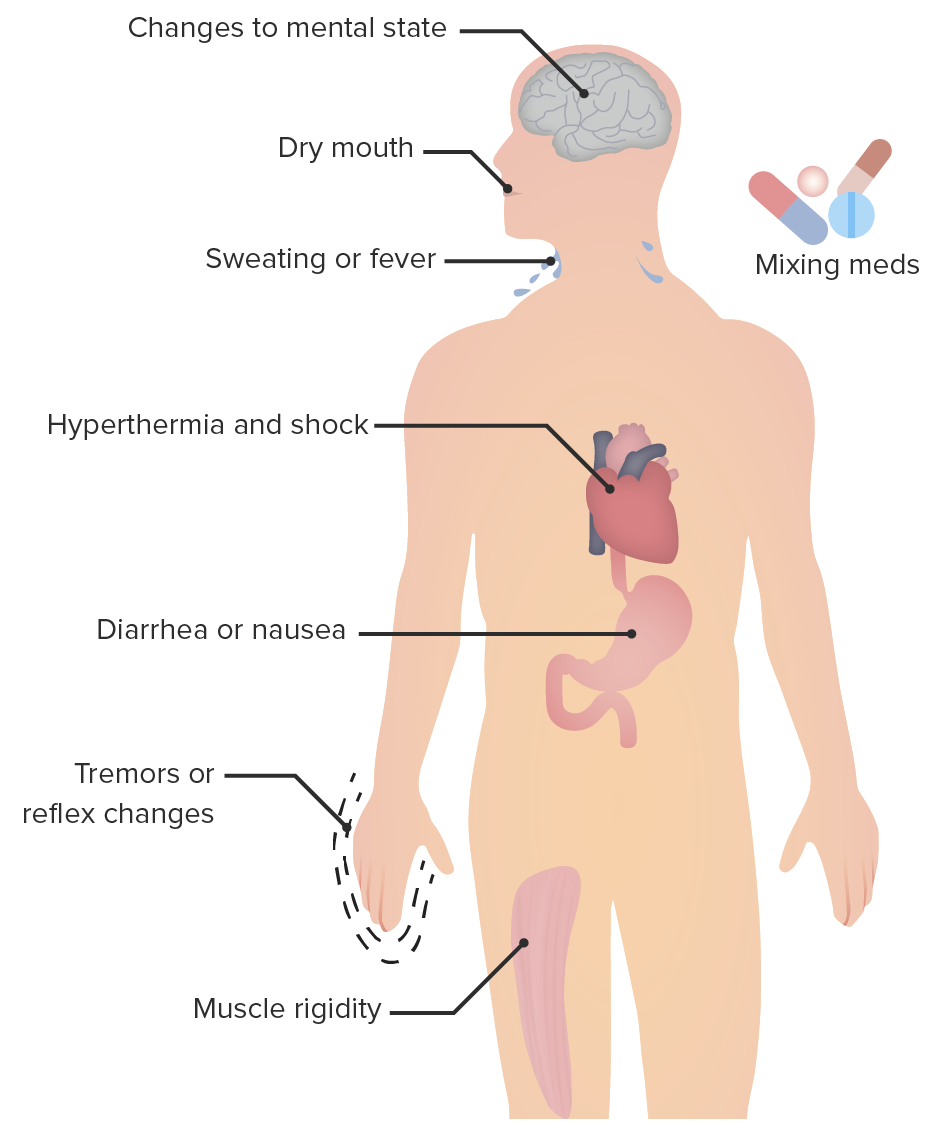
Clinical characteristics of serotonin syndrome:
Serotonin syndrome occurs from any combination of drugs that have the net effect of increasing serotonergic neurotransmission, causing altered mental status, autonomic instability, and neuromuscular abnormalities.
For mild PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease symptoms that have a minimal impact on daily living
| Agent | Mechanism of action | Indications | Side effects | Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation |
|---|---|---|---|---|
| Levodopa | Decarboxylated into dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS | Moderate to severe PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease symptoms |
|
Combination with MAOIs MAOIs Monoamine oxidase inhibitors are a class of antidepressants that inhibit the activity of monoamine oxidase (MAO), thereby increasing the amount of monoamine neurotransmitters (particularly serotonin, norepinephrine, and dopamine). The increase of these neurotransmitters can help in alleviating the symptoms of depression. Monoamine Oxidase Inhibitors |
| Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS agonists | Increase dopaminergic activity by binding to postsynaptic dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors | Current 1st-line therapy for mild to moderate PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease symptoms that impact daily living |
|
|
| Amantadine Amantadine An antiviral that is used in the prophylactic or symptomatic treatment of influenza A. It is also used as an antiparkinsonian agent, to treat extrapyramidal reactions, and for postherpetic neuralgia. The mechanisms of its effects in movement disorders are not well understood but probably reflect an increase in synthesis and release of dopamine, with perhaps some inhibition of dopamine uptake. Antivirals for Influenza ( NMDA antagonist NMDA antagonist Alzheimer Disease) | Antagonist of the NMDA-type glutamate Glutamate Derivatives of glutamic acid. Included under this heading are a broad variety of acid forms, salts, esters, and amides that contain the 2-aminopentanedioic acid structure. Synthesis of Nonessential Amino Acids receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors → antidyskinetic effect | Recommended for mild PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease symptoms that have minimal impact on daily living |
|
|
| MAO-B inhibitors | MAO-B is selectively inhibited → increased intracerebral concentration of dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS | Recommended for mild PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease symptoms that have minimal impact on daily living |
|
Individuals receiving meperidine, tramadol Tramadol A narcotic analgesic proposed for severe pain. It may be habituating. Opioid Analgesics, methadone Methadone A synthetic opioid that is used as the hydrochloride. It is an opioid analgesic that is primarily a mu-opioid agonist. Opioid Analgesics, propoxyphene, cyclobenzaprine Cyclobenzaprine Spasmolytics, or St. John’s wort → increased risk of serotonin Serotonin A biochemical messenger and regulator, synthesized from the essential amino acid l-tryptophan. In humans it is found primarily in the central nervous system, gastrointestinal tract, and blood platelets. Serotonin mediates several important physiological functions including neurotransmission, gastrointestinal motility, hemostasis, and cardiovascular integrity. Receptors and Neurotransmitters of the CNS syndrome |
| Catechol O-methyltransferase (COMT) inhibitors | Selective inhibition of COMT → increased bioavailability Bioavailability Pharmacokinetics and Pharmacodynamics of levodopa → prolonged action of levodopa | Recommended for mild PD PD Parkinson’s disease (PD) is a chronic, progressive neurodegenerative disorder. Although the cause is unknown, several genetic and environmental risk factors are currently being studied. Individuals present clinically with resting tremor, bradykinesia, rigidity, and postural instability. Parkinson’s Disease symptoms that have minimal impact on daily living |
|
|