Dystonia is a hyperkinetic movement disorder characterized by the involuntary contraction of muscles, resulting in abnormal postures or twisting and repetitive movements. Dystonia can present in various ways as may affect many different skeletal muscle groups. Dystonia may be inherited, acquired, or idiopathic Idiopathic Dermatomyositis. The diagnosis is made clinically, and genetic testing Genetic Testing Detection of a mutation; genotype; karyotype; or specific alleles associated with genetic traits, heritable diseases, or predisposition to a disease, or that may lead to the disease in descendants. It includes prenatal genetic testing. Myotonic Dystrophies is recommended in individuals with a family history Family History Adult Health Maintenance of dystonia. Management is with botulinum toxin Botulinum toxin Toxic proteins produced from the species Clostridium botulinum. The toxins are synthesized as a single peptide chain which is processed into a mature protein consisting of a heavy chain and light chain joined via a disulfide bond. The botulinum toxin light chain is a zinc-dependent protease which is released from the heavy chain upon endocytosis into presynaptic nerve endings. Once inside the cell the botulinum toxin light chain cleaves specific snare proteins which are essential for secretion of acetylcholine by synaptic vesicles. This inhibition of acetylcholine release results in muscular paralysis. Botulism or other drugs that target the various neurotransmitters involved in the pathogenesis of dystonia.
Last updated: Jan 13, 2023
Dystonia is a group of movement disorders characterized by involuntary muscle contractions that cause abnormal control of movement and posture. Dystonia is a focal or generalized hyperkinetic disorder that presents with an excessive muscle-contraction response.
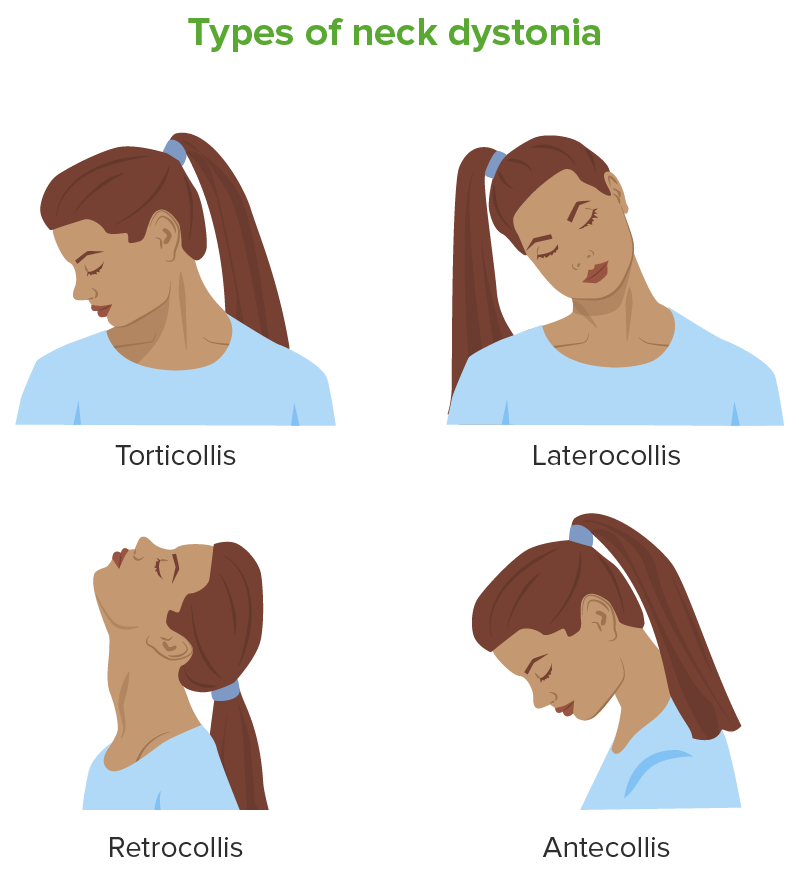
Cervical dystonia presentations
Image by Lecturio.| Name | Type | Onset | Characteristics |
|---|---|---|---|
| Early-onset dystonia | Primary (inherited in an AD AD The term advance directive (AD) refers to treatment preferences and/or the designation of a surrogate decision-maker in the event that a person becomes unable to make medical decisions on their own behalf. Advance directives represent the ethical principle of autonomy and may take the form of a living will, health care proxy, durable power of attorney for health care, and/or a physician’s order for life-sustaining treatment. Advance Directives pattern) generalized | Childhood |
|
| DYT-TOR1A dystonia | Primary (inherited in an AD AD The term advance directive (AD) refers to treatment preferences and/or the designation of a surrogate decision-maker in the event that a person becomes unable to make medical decisions on their own behalf. Advance directives represent the ethical principle of autonomy and may take the form of a living will, health care proxy, durable power of attorney for health care, and/or a physician’s order for life-sustaining treatment. Advance Directives pattern) generalized | Childhood |
|
| DYT-THAP1 dystonia | Primary (inherited in an AD AD The term advance directive (AD) refers to treatment preferences and/or the designation of a surrogate decision-maker in the event that a person becomes unable to make medical decisions on their own behalf. Advance directives represent the ethical principle of autonomy and may take the form of a living will, health care proxy, durable power of attorney for health care, and/or a physician’s order for life-sustaining treatment. Advance Directives pattern) generalized | Adolescence |
|
| DYT-KMT2B dystonia | Primary (usually de novo mutations) | Childhood |
|
| Cervical dystonia (spasmodic torticollis Torticollis A symptom, not a disease, of a twisted neck. In most instances, the head is tipped toward one side and the chin rotated toward the other. The involuntary muscle contractions in the neck region of patients with torticollis can be due to congenital defects, trauma, inflammation, tumors, and neurological or other factors. Cranial Nerve Palsies) |
|
Age: 30–50 years |
|
| Limb dystonia |
|
Adulthood |
|
| Laryngeal dystonia (isolated) |
|
Adulthood |
|
| Blepharospasm (isolated) |
|
Adulthood |
|
| Primary generalized torsion dystonia |
|
Childhood |
|
| Meige syndrome | Primary segmental | Usually adulthood |
|
| Drug-induced dystonia | Secondary | After exposure to offending drugs |
|
| Heredodegenerative disorders | Secondary | Varies |
|
| Dystonia-plus syndromes | Secondary | Usually in childhood |
|
Excessive and frequent muscle contractions leading to abnormal postures and/or repetitive movements are the hallmark of dystonia.
Can affect any part of the body:
Worsened by voluntary action:
Most often occurs in anatomically distinct sites:
May present early in life (early-onset dystonia):
May present later in life (late-onset dystonia):
May have temporal dominance:
May have dynamic features:
May present with comorbid movement disorders:
Dystonia is diagnosed clinically based on a thorough history and physical examination, with a particular focus on musculoskeletal and nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification examination findings.
Treatment is largely symptomatic as there is no cure for dystonia.