High-risk headaches, sometimes also referred to as red-flag headaches, encompass secondary causes of headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess that can result in irreversible end-organ damage, neurologic deficits, loss of vision Vision Ophthalmic Exam, and even death. Entities such as subarachnoid hemorrhage Subarachnoid Hemorrhage Subarachnoid hemorrhage (SAH) is a type of cerebrovascular accident (stroke) resulting from intracranial hemorrhage into the subarachnoid space between the arachnoid and the pia mater layers of the meninges surrounding the brain. Most SAHs originate from a saccular aneurysm in the circle of Willis but may also occur as a result of trauma, uncontrolled hypertension, vasculitis, anticoagulant use, or stimulant use. Subarachnoid Hemorrhage, meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis/ encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis, and intracranial tumors carry high morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status risks if not recognized and treated immediately. Diagnosis of a high-risk headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess requires a high degree of clinical suspicion and is made by conducting a thorough clinical evaluation followed by a targeted workup for the most likely etiology. Management depends on the etiology but consists of prompt treatment of the underlying cause and stabilization of accompanying organ dysfunction.
Last updated: Mar 6, 2023
A high-risk headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess is any new and sudden onset, typically severe, headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess with the potential to cause damage to cerebral or precerebral structures or functions.
There are many etiologies of high-risk headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess that the clinician Clinician A physician, nurse practitioner, physician assistant, or another health professional who is directly involved in patient care and has a professional relationship with patients. Clinician–Patient Relationship should be aware of and work to rule out when a severe headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess is encountered. The most common etiologies are presented here, separated into vascular, infectious, neoplastic, and miscellaneous causes.
| Clinical entity | Historical clues/risk factors | Clinical features |
|---|---|---|
| Subarachnoid hemorrhage Subarachnoid Hemorrhage Subarachnoid hemorrhage (SAH) is a type of cerebrovascular accident (stroke) resulting from intracranial hemorrhage into the subarachnoid space between the arachnoid and the pia mater layers of the meninges surrounding the brain. Most SAHs originate from a saccular aneurysm in the circle of Willis but may also occur as a result of trauma, uncontrolled hypertension, vasculitis, anticoagulant use, or stimulant use. Subarachnoid Hemorrhage ( SAH SAH Subarachnoid hemorrhage (SAH) is a type of cerebrovascular accident (stroke) resulting from intracranial hemorrhage into the subarachnoid space between the arachnoid and the pia mater layers of the meninges surrounding the brain. Most SAHs originate from a saccular aneurysm in the circle of Willis but may also occur as a result of trauma, uncontrolled hypertension, vasculitis, anticoagulant use, or stimulant use. Subarachnoid Hemorrhage) |
|
|
| Reversible cerebral vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure syndrome (RCVS) |
|
|
| Cervical artery dissection/ vertebral artery Vertebral artery The first branch of the subclavian artery with distribution to muscles of the neck; vertebrae; spinal cord; cerebellum; and interior of the cerebrum. Lateral Medullary Syndrome (Wallenberg Syndrome) dissection |
|
|
| Cerebral vein thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus/dural sinus thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus |
|
|
| Subdural hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception/epidural hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception |
|
|
| Intraparenchymal hemorrhage (IPH) |
|
Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables presentation depending on site of bleed (much like cerebrovascular accident Cerebrovascular accident An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke/ TIA TIA Transient ischemic attack (TIA) is a temporary episode of neurologic dysfunction caused by ischemia without infarction that resolves completely when blood supply is restored. Transient ischemic attack is a neurologic emergency that warrants urgent medical attention. Transient Ischemic Attack (TIA)) |
| Idiopathic Idiopathic Dermatomyositis intracranial hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension |
|
|
| Spontaneous intracranial hypotension Intracranial hypotension Reduction of cerebrospinal fluid pressure characterized clinically by orthostatic headache and occasionally by an abducens nerve palsy; hearing loss; nausea; neck stiffness, and other symptoms. This condition may be spontaneous or secondary to cerebrospinal fluid leak; spinal puncture; neurosurgical procedures; dehydration; uremia; trauma; and other processes. Chronic hypotension may be associated with subdural hematomas or hygromas. Subdural Hemorrhage |
|
|
| Giant-cell arteritis Giant-cell arteritis A systemic autoimmune disorder that typically affects medium and large arteries, usually leading to occlusive granulomatous vasculitis with transmural infiltrate containing multinucleated giant cells. The temporal artery is commonly involved. This disorder appears primarily in people over the age of 50. Symptoms include fever; fatigue; headache; visual impairment; pain in the jaw and tongue; and aggravation of pain by cold temperatures. Vasculitides |
|
|
| Hypertensive encephalopathy Encephalopathy Hyper-IgM Syndrome |
|
|
| Posterior reversible encephalopathy Encephalopathy Hyper-IgM Syndrome syndrome |
|
|
| Clinical entity | Historical clues/risk factors | Clinical features |
|---|---|---|
| Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis and/or encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis |
|
|
| Brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease |
|
|
| Clinical entity | Historical clues/risk factors | Clinical features |
|---|---|---|
| Brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification tumor Tumor Inflammation |
|
|
| Colloid Colloid Colloid solutions include large proteins or cells that do not readily cross capillary membranes. They remain in the ecf and do not distribute into the icf (similar to crystalloids). Intravenous Fluids cyst of 3rd ventricle |
|
|
| Pituitary apoplexy Pituitary apoplexy The sudden loss of blood supply to the pituitary gland, leading to tissue necrosis and loss of function (panhypopituitarism). The most common cause is hemorrhage or infarction of a pituitary adenoma. It can also result from acute hemorrhage into sella turcica due to head trauma; intracranial hypertension; or other acute effects of central nervous system hemorrhage. Clinical signs include severe headache; hypotension; bilateral visual disturbances; unconsciousness; and coma. Hypopituitarism |
|
|
| Clinical entity | Historical clues/risk factors | Clinical features |
|---|---|---|
| Acute narrow-angle glaucoma Glaucoma Glaucoma is an optic neuropathy characterized by typical visual field defects and optic nerve atrophy seen as optic disc cupping on examination. The acute form of glaucoma is a medical emergency. Glaucoma is often, but not always, caused by increased intraocular pressure (IOP). Glaucoma |
|
|
| CO toxicity Toxicity Dosage Calculation |
|
|
| Preeclampsia Preeclampsia A complication of pregnancy, characterized by a complex of symptoms including maternal hypertension and proteinuria with or without pathological edema. Symptoms may range between mild and severe. Pre-eclampsia usually occurs after the 20th week of gestation, but may develop before this time in the presence of trophoblastic disease. Hypertensive Pregnancy Disorders/ eclampsia Eclampsia Onset of hyperreflexia; seizures; or coma in a previously diagnosed pre-eclamptic patient (pre-eclampsia). Hypertensive Pregnancy Disorders |
|
|
It is important to take a focused, thorough history:
It is important to do a focused, thorough examination:
Suspected infectious etiology:
Suspected hematologic/vascular etiology:
Suspected neoplastic etiology:
Thunderclap headache Thunderclap Headache Subarachnoid Hemorrhage:
Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis or encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis:
Increased ICP Increased ICP Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage:
CO toxicity Toxicity Dosage Calculation:
Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess with neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways:
Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess in adults > 50 years of age:
Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess in immunosuppressed individuals:
Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess in individuals with cancer:
Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess during pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care/postpartum:
Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess with visual impairment, periorbital Periorbital Orbital and Preseptal Cellulitis pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, ophthalmoplegia Ophthalmoplegia Paralysis of one or more of the ocular muscles due to disorders of the eye muscles, neuromuscular junction, supporting soft tissue, tendons, or innervation to the muscles. Orbital and Preseptal Cellulitis:

Subarachnoid hemorrhage:
CT scan showing intracranial bleeding
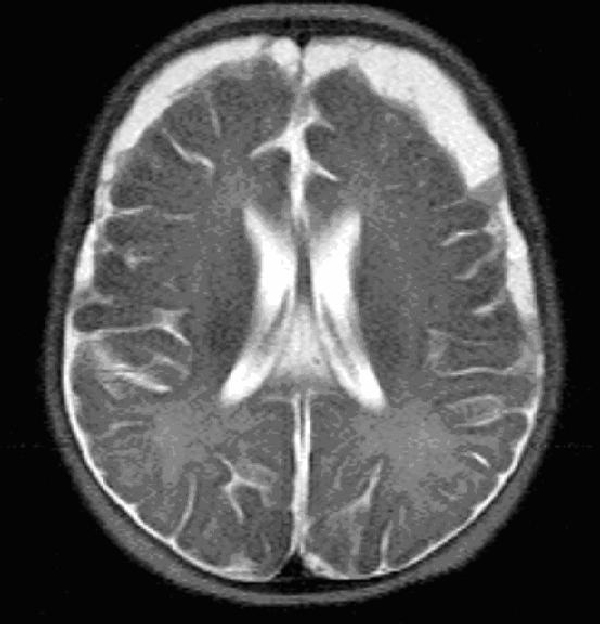
MRI in meningitis:
Note the bifrontal/bitemporal subdural empyema Image: “MRI HEAD (axial) without contrast” by Yip K et al. License: CC BY 3.0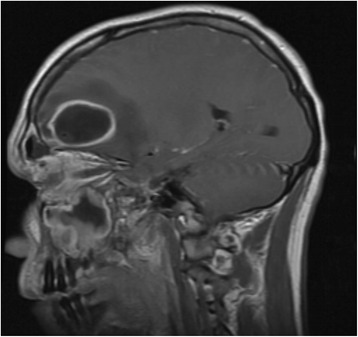
Head MRI showing frontal abscess:
Note the hyperintensity extending from the frontal sinus to the abscess cavity.