Carotid and vertebral artery Vertebral artery The first branch of the subclavian artery with distribution to muscles of the neck; vertebrae; spinal cord; cerebellum; and interior of the cerebrum. Lateral Medullary Syndrome (Wallenberg Syndrome) dissections occur when the integrity of the arterial wall structure fails, usually abruptly, resulting in intramural hematoma Hematoma A collection of blood outside the blood vessels. Hematoma can be localized in an organ, space, or tissue. Intussusception formation and a false lumen False lumen Aortic Dissection between the tunica media Tunica media The middle layer of blood vessel walls, composed principally of thin, cylindrical, smooth muscle cells and elastic tissue. It accounts for the bulk of the wall of most arteries. The smooth muscle cells are arranged in circular layers around the vessel, and the thickness of the coat varies with the size of the vessel. Arteries: Histology and the intimal or adventitial layers. This may result in aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS), or occlusion. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with unilateral head or neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and/or stroke-like symptoms. Minor trauma or neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess manipulation are common preceding events. Dissections require imaging to confirm and are treated with medical and sometimes surgical management. Complications can include cerebrovascular stroke and, in severe cases, death.
Last updated: Jan 16, 2024
Arterial dissection is a violation of the structural integrity of the arterial wall that results in blood accumulating between the layers.
Dissection formation:
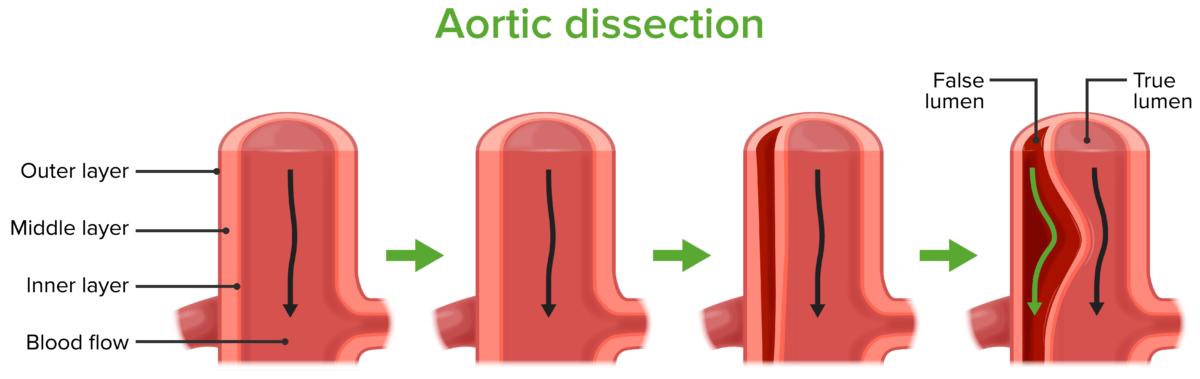
Process of dissection formation
Image by Lecturio.Most common locations:
Pathophysiologic effects:
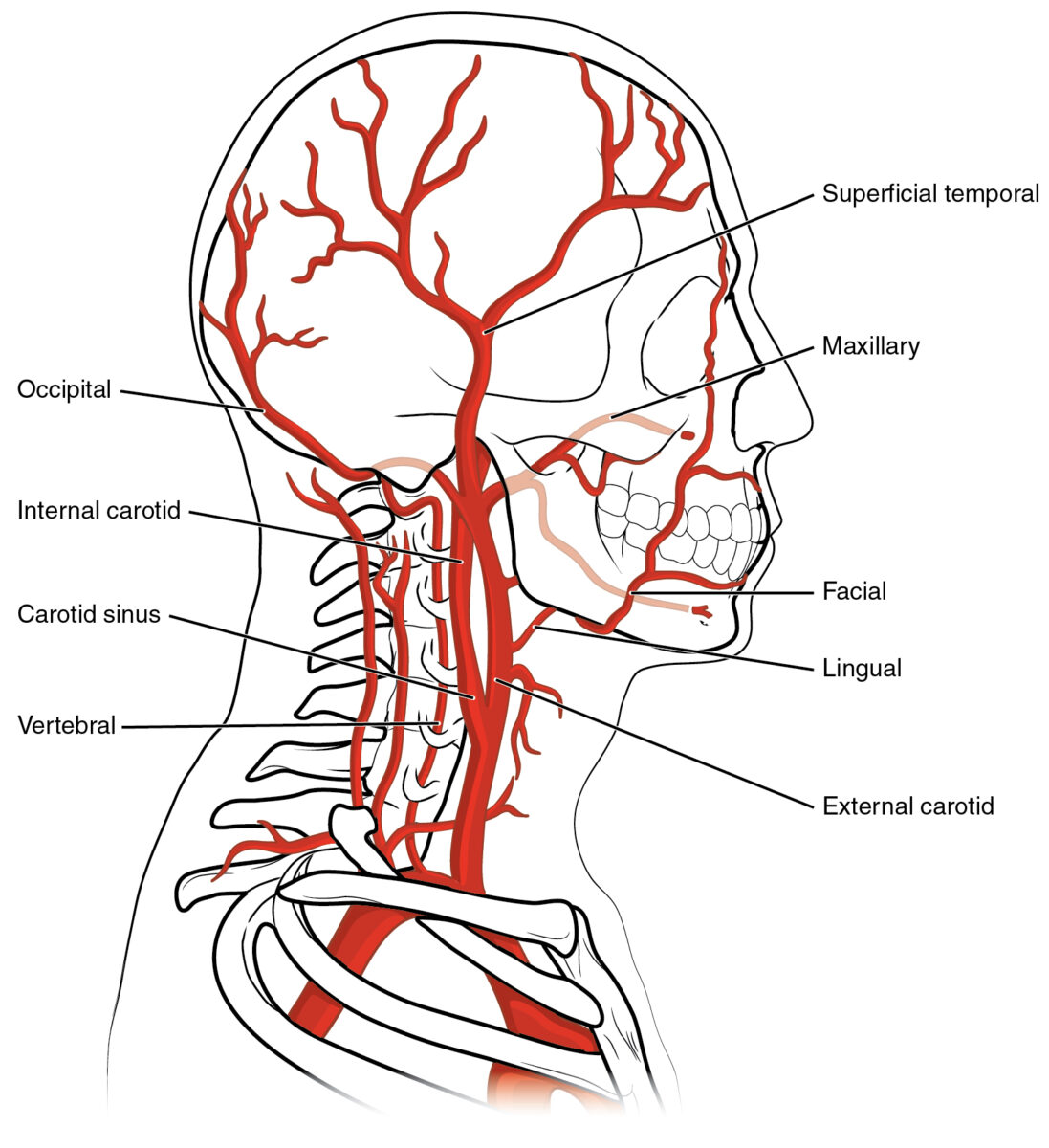
Anatomy of vertebral and carotid arteries
Image: “2122 Common Carotid Artery” by OpenStax College. License: CC BY 3.0Local symptoms:
Ischemic symptoms:
Subarachnoid hemorrhage Subarachnoid Hemorrhage Subarachnoid hemorrhage (SAH) is a type of cerebrovascular accident (stroke) resulting from intracranial hemorrhage into the subarachnoid space between the arachnoid and the pia mater layers of the meninges surrounding the brain. Most SAHs originate from a saccular aneurysm in the circle of Willis but may also occur as a result of trauma, uncontrolled hypertension, vasculitis, anticoagulant use, or stimulant use. Subarachnoid Hemorrhage:
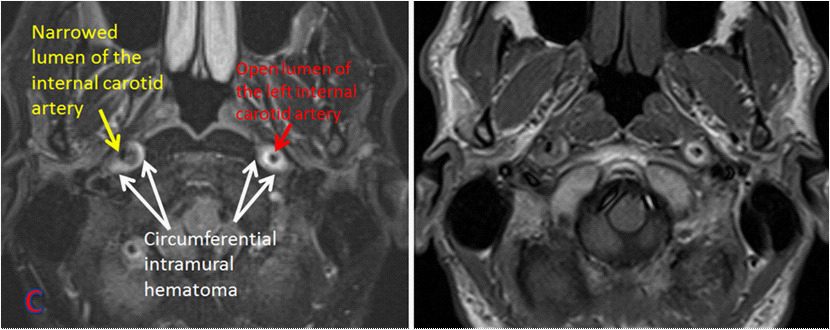
MRA of bilateral internal carotid dissection
Image: “MR angiography of bilateral internal carotid dissection” by Shazia Mirza and Sankalp Gokhale. License: CC BY 4.0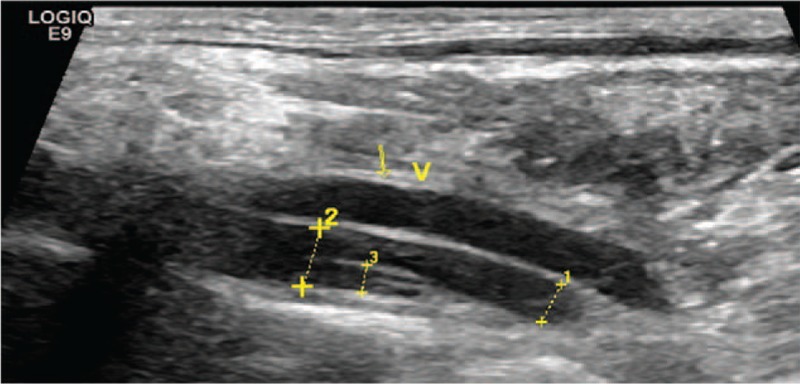
Vertebral artery dissection: ultrasound showing intimal flap in left vertebral artery
Image: “The advantage of ultrasonography in the diagnosis of extracranial vertebral artery dissection” by Medicine. License: CC BY 4.0