Subclavian steal syndrome occurs when narrowing/occlusion of the subclavian artery proximal to the origin of the vertebral artery Vertebral artery The first branch of the subclavian artery with distribution to muscles of the neck; vertebrae; spinal cord; cerebellum; and interior of the cerebrum. Lateral Medullary Syndrome (Wallenberg Syndrome) causes a reversal of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure in the ipsilateral vertebral artery Vertebral artery The first branch of the subclavian artery with distribution to muscles of the neck; vertebrae; spinal cord; cerebellum; and interior of the cerebrum. Lateral Medullary Syndrome (Wallenberg Syndrome) to continue perfusing the ipsilateral arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy. The most common cause is atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis. Symptoms are rare, but when they occur are usually triggered by physical exertion of the arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy and subsequent hypoperfusion of the arm Arm The arm, or "upper arm" in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy or brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may present with claudication, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, pallor, paresthesias Paresthesias Subjective cutaneous sensations (e.g., cold, warmth, tingling, pressure, etc.) that are experienced spontaneously in the absence of stimulation. Posterior Cord Syndrome, and weakened pulse in the affected extremity. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may also present with transient neurologic disturbances concerning for a stroke. Diagnosis is made by clinical findings and imaging (ultrasound, CT, MRI). In addition to appropriate management of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis, symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may need angioplasty Angioplasty Reconstruction or repair of a blood vessel, which includes the widening of a pathological narrowing of an artery or vein by the removal of atheromatous plaque material and/or the endothelial lining as well, or by dilatation (balloon angioplasty) to compress an atheroma. Except for endarterectomy, usually these procedures are performed via catheterization as minimally invasive endovascular procedures. Cardiac Surgery/stenting or surgical revascularization Revascularization Thromboangiitis Obliterans (Buerger Disease).
Last updated: Dec 1, 2024
Subclavian steal syndrome is the reversal of blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure in the vertebral artery Vertebral artery The first branch of the subclavian artery with distribution to muscles of the neck; vertebrae; spinal cord; cerebellum; and interior of the cerebrum. Lateral Medullary Syndrome (Wallenberg Syndrome) on the side of a stenotic subclavian artery that produces symptoms of arterial insufficiency in the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification or upper extremity.
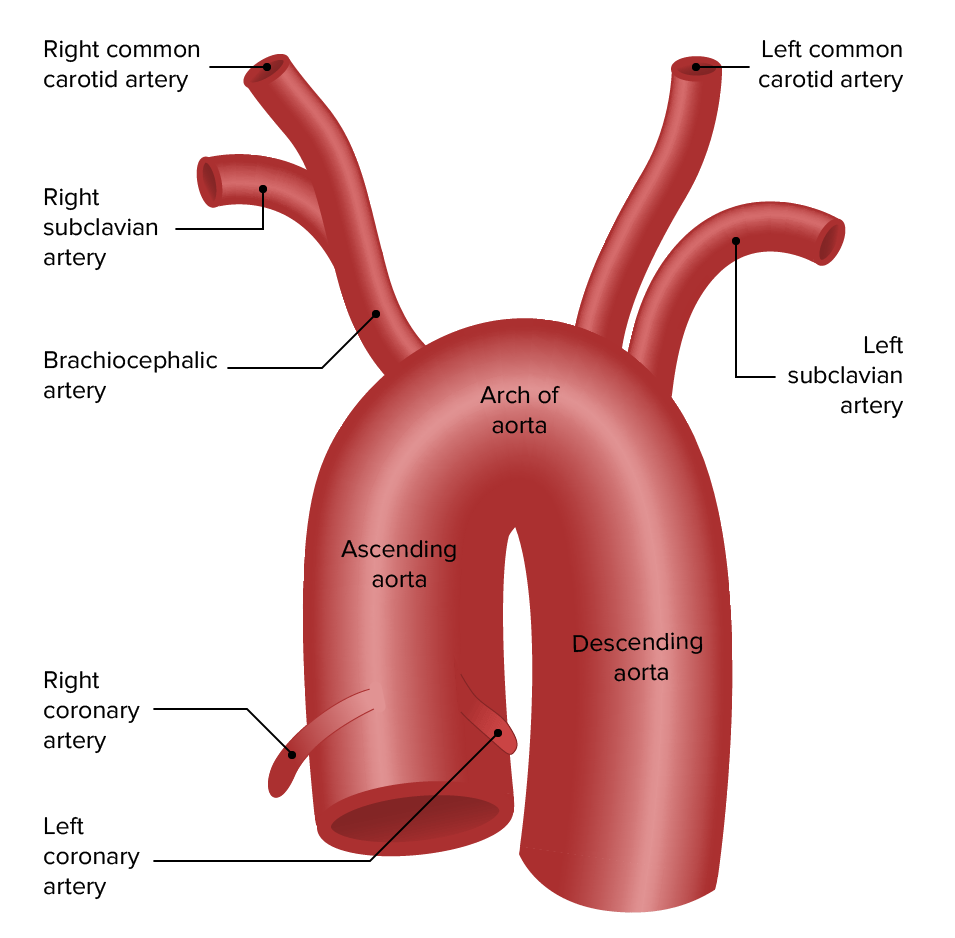
Anatomy of the aortic arch
Image by Lecturio.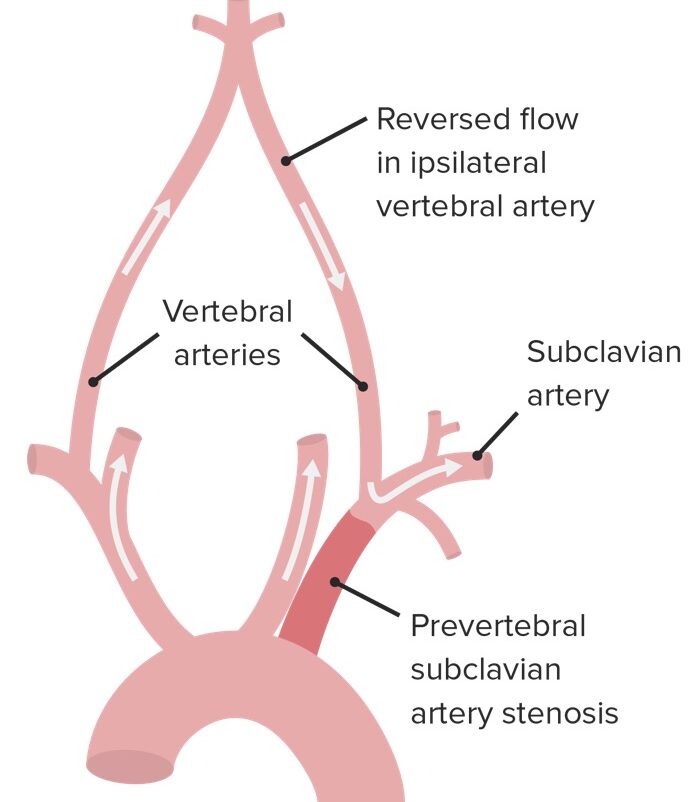
Pathophysiology of subclavian steal syndrome:
Note the reversed blood flow in the ipsilateral vertebral artery.
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with subclavian stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS)/steal are asymptomatic.
Symptoms of (ipsilateral) limb ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage/hypoperfusion:
Symptoms related to cerebral hypoperfusion/vertebrobasilar insufficiency:

Percutaneous transradial catheter angiogram showing critical ostial subclavian artery stenosis that caused coronary subclavian steal syndrome
Image: “Critical ostial subclavian artery stenosis” by Section of Cardiology, Christiana Care Health System, Newark, DE 19718, USA. License: CC BY 3.0